Mini Review
Mini Review
Manifestations, Diagnosis, and Treatment of Pediatric Psychocutaneous Diseases
Sahithi Talasila BS*
Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, Pennsylvania, USA
Sahithi Talasila BS, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, Pennsylvania, USA.
Received Date: June 28, 2024; Published Date: July 05, 2024
Abstract
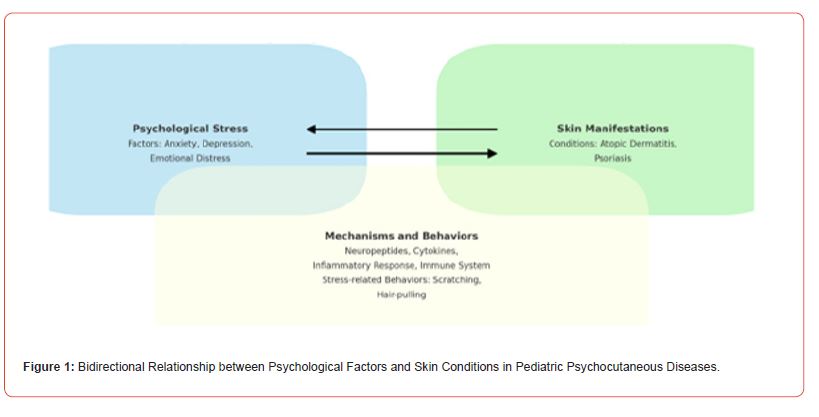
Pediatric psychocutaneous diseases represent a complex interplay between dermatological and psychological factors, presenting significant challenges in clinical management. These disorders, such as atopic dermatitis, psoriasis, trichotillomania, excoriation disorder, and acne excoriée, demonstrate a bidirectional relationship where psychological stressors exacerbate skin conditions and vice versa. Studies show that 20-30% of children with chronic skin conditions experience significant psychological comorbidities, including higher rates of anxiety and depression.
Effective management requires an interdisciplinary approach, integrating dermatological treatments with psychological interventions. Cognitive-behavioral therapy (CBT) and pharmacotherapy are crucial in addressing both dermatological and psychological symptoms. Early intervention and continuous management are essential to prevent recurrence and improve the quality of life for affected children.
This review examines the epidemiology, pathophysiology, clinical presentation, and management strategies of pediatric psychocutaneous diseases. By providing an integrated framework, it aims to enhance diagnostic accuracy, treatment efficacy, and overall patient care. Understanding the mind-skin connection and fostering interdisciplinary collaboration are vital for advancing clinical outcomes and supporting the well-being of pediatric patients with psychocutaneous disorders.
Keywords: Psychocutaneous diseases; Trichotillomania; Excoriation disorder; Pediatric dermatology
Introduction
Pediatric psychocutaneous diseases present unique challenges in clinical practice due to their complex and multifactorial nature. These disorders underscore the intricate and bidirectional relationship between the skin and the psyche, where psychological fac tors can significantly influence skin health and vice versa (Figure 1). Effectively managing these conditions requires an interdisciplinary approach that integrates dermatological and psychological expertise [1-3].
Pediatric psychocutaneous diseases are particularly challenging due to the interplay of developmental, psychological, and social factors that influence disease expression and patient management. Common examples include atopic dermatitis, psoriasis, trichotillomania, excoriation disorder, and acne excoriée, all of which can be exacerbated by psychological stressors such as anxiety, depression, and obsessive-compulsive behaviors [4-6]. Studies indicate that approximately 20-30% of children with chronic skin conditions, such as atopic dermatitis and psoriasis, experience significant psychological comorbidities [7]. For instance, children with atopic dermatitis have a 2-6 times higher prevalence of anxiety and depression compared to their healthy peers [8]. Similarly, pediatric psoriasis is associated with increased rates of psychological issues, including suicidal ideation, affecting about 5-10% of these patients in severe cases [9].
Psychodermatological disorders are a heterogeneous group of skin conditions significantly associated with mental disorders. Dermatoses in this category often have a substantial negative impact on mental health or may run a clinical course determined by the primary psychiatric or psychological disorder. For example, skin conditions can precipitate serious psychiatric illnesses in individuals without preexisting mental health problems, while primary psychiatric conditions such as trichotillomania may present primarily with skin complaints. In these cases, the skin conditions may be the sole manifestation of the underlying psychiatric conditions, and the patient may first present to the dermatologist [10-15].
The relationship between skin conditions and mental health is often bidirectional, complex, and incompletely understood. Psychological factors can trigger or aggravate skin conditions, and exacerbated dermatoses can induce further psychological problems, creating a vicious cycle. This cycle is characteristic of typical psych dermatological disorders and is particularly pronounced in pediatric populations due to their developmental stages [16-18].
The concept of a bidirectional relationship between the mind and the skin is well-documented, with several mechanisms proposed to explain this interaction. The skin, being the largest organ of the body, has an extensive network of nerves and is highly responsive to emotional and psychological states. Psychological stress can lead to the release of neuropeptides and cytokines that influence skin inflammation and immune responses, exacerbating conditions like psoriasis and atopic dermatitis. Conversely, chronic skin conditions can significantly impact a child’s psychological well-being, leading to emotional distress, social anxiety, and depression. The visible nature of skin diseases can result in stigmatization and decreased self-esteem, further perpetuating the cycle of psychological and dermatological symptoms [16,17].
Managing pediatric psychocutaneous diseases is more challenging than in adults. Children are in critical stages of psychological and social development, making them more vulnerable to the impacts of chronic illness. The visible symptoms can lead to bullying and social isolation, compounding the psychological burden. Moreover, children may have difficulty understanding and articulating their symptoms, complicating diagnosis and treatment [18- 20].
The impact of these conditions extends beyond individual patients to their families and caregivers, who often experience considerable emotional and financial burdens. The chronic and recurrent nature of these diseases necessitates ongoing medical care, which can strain family resources and contribute to caregiver stress. Effective management strategies must therefore address not only the patient but also provide support for the entire family unit [21,22].
This literature review aims to examine the epidemiology, pathophysiology, clinical presentation, and management strategies of pediatric psychocutaneous diseases. By highlighting the unique challenges and complexities associated with these conditions, this review seeks to provide an integrated framework for clinicians to improve diagnostic accuracy, treatment efficacy, and overall patient care in this vulnerable population.
Review
Pediatric psychocutaneous disorders, although often underreported, are relatively prevalent and pose significant challenges in clinical practice. These disorders encompass a variety of conditions where psychological factors significantly influence dermatological health. The prevalence of psychocutaneous disorders among pediatric populations varies widely depending on the specific condition and demographic factors.
For instance, atopic dermatitis, one of the most common psychocutaneous disorders, affects approximately 15-20% of children worldwide. Research indicates that children with AD are more likely to experience psychological comorbidities, such as anxiety and depression, compared to their healthy peers. Psoriasis, another prevalent condition, is estimated to affect about 0.5-2% of children, with significant psychological impacts including increased rates of anxiety, depression, and even suicidal ideation in severe cases [23].
Trichotillomania and excoriation disorder are also notable among pediatric psychocutaneous conditions. These disorders often present in childhood or adolescence and can lead to significant distress and impairment. The prevalence of trichotillomania in children is estimated to be around 1-2%, while excoriation disorder is believed to affect approximately 1-5% of the population, though exact figures in children are less clear due to underreporting [24].
The epidemiology of pediatric psychocutaneous disorders is further complicated by the bidirectional relationship between psychological and dermatological symptoms. Chronic skin conditions can lead to significant psychological distress, while psychological factors can exacerbate or trigger dermatological symptoms. This interplay underscores the need for comprehensive epidemiological studies that consider both the dermatological and psychological aspects of these conditions [25].
The pathophysiology of pediatric psychocutaneous disorders is multifaceted, involving complex interactions between the skin, the nervous system, and the immune system. The skin, as the largest organ of the body, is highly innervated and responsive to psychological stressors. This responsiveness is mediated by various neuroendocrine and immune mechanisms that link psychological states to skin health [26].
One key mechanism involves the hypothalamic-pituitary-adrenal (HPA) axis, which plays a central role in the body’s response to stress. Psychological stress activates the HPA axis, leading to the release of cortisol and other stress hormones. These hormones can have direct effects on the skin, including altering immune responses and increasing inflammation. For example, in atopic dermatitis, stress-induced activation of the HPA axis can exacerbate inflammation and itch, leading to a worsening of symptoms [26].
Neuropeptides, such as substance P and calcitonin gene-related peptide (CGRP), also play a significant role in the pathophysiology of psychocutaneous disorders. These neuropeptides are released in response to stress and can modulate immune responses in the skin. Substance P, for instance, can increase the production of pro-inflammatory cytokines, contributing to conditions like psoriasis and atopic dermatitis [27].
The skin’s own neuroendocrine system also plays a critical role. Keratinocytes, the predominant cell type in the epidermis, can produce and respond to neuropeptides and hormones. This local neuroendocrine activity can modulate skin inflammation and barrier function, linking psychological stress to skin health. For example, stress can impair the skin barrier function, leading to increased trans epidermal water loss and making the skin more susceptible to irritants and allergens [28].
Another important aspect of the pathophysiology is the role of the immune system. Chronic stress can dysregulate immune function, leading to a shift towards a pro-inflammatory state. In conditions like psoriasis, this can result in the overactivation of T cells and the production of inflammatory cytokines such as TNF-alpha and IL-17, driving the characteristic skin lesions [28].
The microbiome of the skin also appears to be influenced by psychological stress. Stress can alter the composition of the skin microbiota, which in turn can affect skin health. Dysbiosis, or an imbalance in the microbial community, has been linked to various skin disorders, including atopic dermatitis and acne. The exact mechanisms by which stress influences the skin microbiome are still being explored, but they likely involve changes in skin barrier function and immune responses [28].
The pathophysiology of pediatric psychocutaneous disorders involves a complex interplay between psychological stress, neuroendocrine responses, immune function, and the skin microbiome. These interactions underscore the need for a holistic approach to understanding and managing these conditions, integrating dermatological and psychological care to address both the physical and mental health aspects of pediatric psychocutaneous diseases [28].
Clinical presentations of pediatric psychocutaneous diseases are diverse. Children with conditions like atopic dermatitis and psoriasis often exhibit exacerbated symptoms due to psychological stress, which can manifest as severe itching, scratching, and other skin lesions. Trichotillomania and excoriation disorder are characterized by repetitive behaviors such as hair-pulling and skin-picking, leading to visible damage and potential infections. Psychogenic itch and urticaria, linked to emotional distress, further complicate the clinical picture by adding layers of discomfort and social stigmatization [29].
Diagnosing these conditions involves a comprehensive evaluation that includes detailed histories of dermatological and psychological symptoms, as well as assessments of psychosocial stressors. Effective diagnosis requires collaboration between dermatologists and mental health professionals to identify underlying psychological factors contributing to the skin condition. Tools such as the Child Behavior Checklist (CBCL) and the Strengths and Difficulties Questionnaire (SDQ) are instrumental in assessing psychiatric comorbidities. Advanced diagnostic techniques, including psychometric assessments and, in some cases, imaging studies, help to differentiate between primary dermatologic disorders with psychiatric components and purely psychiatric conditions with dermatologic manifestations [29].
Treatment approaches are multifaceted, combining pharmacological and psychotherapeutic interventions. Psychotherapy, particularly cognitive-behavioral therapy (CBT), is effective in managing stress, anxiety, and compulsive behaviors associated with psychocutaneous diseases. CBT helps children develop healthier coping mechanisms, thereby reducing the psychological triggers of dermatological symptoms. Pharmacotherapy may include the use of antidepressants or anxiolytics to manage underlying psychiatric conditions, along with dermatological treatments like topical corticosteroids and antihistamines to alleviate physical symptoms [27].
Family involvement is crucial in the management of pediatric psychocutaneous diseases. Educating families about the nature of these conditions and involving them in the treatment process can enhance treatment adherence and efficacy. Families play a vital role in providing emotional support and helping to implement behavioral strategies at home. Support groups and psychoeducation programs for families can provide additional resources and a sense of community, which are beneficial in managing the chronic nature of these conditions [30].
The prognosis for pediatric psychocutaneous diseases varies depending on the specific condition and the effectiveness of the treatment approach. With a comprehensive, multidisciplinary treatment plan, many children can achieve significant improvement in both dermatological and psychological symptoms. Early intervention and continuous management are key to preventing the recurrence of symptoms and improving overall quality of life [30].
The current state of the field reflects a growing recognition of the importance of integrating dermatology and psychiatry. There is increasing awareness among healthcare providers about the necessity of interdisciplinary collaboration to effectively manage these complex conditions. Research is focusing on better understanding the underlying mechanisms of psychocutaneous diseases, exploring the role of neuroimmunology in the mind-skin connection, and developing more effective diagnostic tools and treatment modalities [30].
The future of pediatric psychocutaneous diseases is promising, with advancements expected in both understanding and managing these conditions. Continued research and interdisciplinary collaboration will be key to improving clinical outcomes. Developing standardized protocols for the diagnosis and treatment of psychocutaneous diseases, along with enhancing training for healthcare providers, will contribute to better care for affected children. Additionally, increasing public and professional awareness about the significance of the mind-skin connection will further support the holistic management of these complex disorders.
Pediatric psychocutaneous diseases are complex and multifaceted, requiring a comprehensive and integrated approach for effective management. Advances in research, diagnosis, and treatment, along with enhanced interdisciplinary collaboration, hold the promise of improved outcomes and quality of life for children affected by these challenging conditions.
Conclusion
In conclusion, pediatric psychocutaneous diseases exemplify the complex interplay between dermatological and psychological factors, necessitating an integrated approach to diagnosis and treatment. These conditions, which include atopic dermatitis, psoriasis, trichotillomania, and excoriation disorder, are influenced by psychological stressors that exacerbate dermatological symptoms and vice versa. The bidirectional relationship between the mind and the skin highlights the importance of multidisciplinary care involving dermatologists, psychiatrists, and other healthcare professionals. Effective management strategies should encompass pharmacological treatments, psychotherapeutic interventions, and family involvement to address both the psychological and dermatological components. Early intervention and continuous management are crucial for improving clinical outcomes and quality of life for affected children. Future research should focus on elucidating the underlying mechanisms of these diseases, developing standardized diagnostic and treatment protocols, and enhancing interdisciplinary collaboration to better serve this vulnerable population. With continued advancements and a holistic approach, there is a promising outlook for improved care and outcomes in pediatric psychocutaneous diseases.
Acknowledgment
None.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
- Gupta MA, Gupta AK (2013) Psychiatric and psychological co-morbidity in patients with dermatologic disorders. Clinics in Dermatology 4(12): 833-842.
- Kimyai Asadi A, Usman A (2001) The role of psychological stress in skin disease. Journal of Cutaneous Medicine and Surgery 5(2): 140-145.
- Arck PC, Paus R (2006) From the brain-skin connection: the neuroendocrine-immune misalliance of stress and itch. Neuroimmunomodulation 13(5-6): 347-356.
- Peters EM, Ericson ME, Hosoi J, Botchkarev VA (2006) The biology of neuropeptides in skin and their role in dermatological diseases. Clinics in Dermatology 24(1): 7-16.
- Picardi A, Pasquini P, Cattaruzza MS, Gaetano P (2004) Stress, social support, emotional regulation, and exacerbation of alopecia areata. Journal of Investigative Dermatology 122(2): 200-206.
- Schmitt J, Apfelbacher C, Heinric J, Weidinger S, Romanos M, et al. (2013) Association of atopic eczema and attention-deficit/hyperactivity disorder–meta-analysis of epidemiologic studies. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie 41(1): 35-42.
- Tollefson MM, Crowson CS, Mc Evoy MT, Kremers HM (2010) Incidence of psoriasis in children: a population-based study. Journal of the American Academy of Dermatology 62(6): 979-987.
- Chamlin SL (2006) The psychosocial burden of childhood atopic dermatitis. Archives of Dermatology 19(2): 104-107.
- Fried RG, Gupta MA (2004) Current concepts in psychodermatology. Dermatologic Clinics 22(4): 487-495.
- Goodman R (1997) The Strengths and Difficulties Questionnaire: a research note. Journal of Child Psychology and Psychiatry 38(5): 581-586.
- Kupfer DJ, Regier DA (2011) Neuroscience, clinical evidence, and the future of psychiatric classification in DSM-5. American Journal of Psychiatry 168(7): 672-674.
- Franklin ME, Zagrabbe K, Benavides KL (2011) Trichotillomania and its treatment: a review and recommendations. Expert Review of Neurotherapeutics 11(8): 1165-1174.
- Kabat Zinn J (2003) Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice 10(2): 144-156.
- Stewart AL, Ware JE (1992) Measuring functioning and well-being: the Medical Outcomes Study approach. Duke University Press.
- Al Hawsawi K, Pope E (2011) Pediatric psychocutaneous disorders: a review of primary psychiatric disorders with dermatologic manifestations. American Journal of Clinical Dermatology 12(4): 247-257.
- American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association.
- Grant JE, Odlaug BL (2009) Updates on pathological skin picking. Current Psychiatry Reports 11(4): 283-288.
- Jafferany M (2007) Psychodermatology: a guide to understanding common psychocutaneous disorders. Primary Care Companion Journal of Clinical Psychiatry 9(3): 203-213.
- Folks DG, Warnock JK (2001) Psychocutaneous disorders. Current Psychiatry Reports 3(3): 219-225.
- Lee CS, Accordino R, Howard J, Koo J (2008) Psychopharmacology in dermatology. Dermatologic Therapy 21(1): 69-82.
- Jafferany M, Feng Y, Hornung RL (2009) Trichodaganomania: the compulsive habit of biting one’s own hair. Journal of the American Academy of Dermatology 60(4): 689-691.
- Duke DC, Keeley ML, Geffken G R, Storch EA (2010) Trichotillomania: a current review. Clinical Psychology Review 30(2): 181-193.
- Van Minnen A, Hoogduin KA, Keijsers GP, Hellenbrand I, Hendriks GJ, et al. (2003) Treatment of trichotillomania with behavioral therapy or fluoxetine: a randomized, waiting-list controlled study. Archives of General Psychiatry 60: 517-522.
- Seedat S, Stein DJ, Harvey BH (2001) Inositol in the treatment of trichotillomania and compulsive skin picking. Journal of Clinical Psychiatry 62: 60-61.
- Sandoz A, Koenig T, Kusnir D (2008) Psychocutaneous disorders. In Wolff K, Goldsmith LA, Katz SI (), Fitzpatrick’s Dermatology in General Medicine (7th edn) New York: McGraw Hill pp: 912-921.
- Ressmann AC, Butterworth T (1952) Localized acquired hypertrichosis. AMA Archives of Dermatology and Syphilology 65(4): 458-463.
- Heaton KW, Mountford RA (1992) Nail-biting in the population and its relationship to irritable bowel syndrome. Journal of the Royal Society of Medicine 85: 457.
- Williams TI, Rose R, Chisholm S (2007) What is the function of nail biting: an analog assessment study. Behavior Research and Therapy 45: 989-995.
- Luker J (2006) Diseases of the oral mucosa and tongue. In Harper J, Oranje A, Prose N (Eds.), Textbook of Pediatric Dermatology (2nd edn) Boston, MA: Blackwell Scientific Publications pp: 1725-1749.
- Gattu S, Rashid RM, Khachemoune A (2009) Self-inflicted skin lesions: a review of dermatitis artefacta. Cutis 84(5): 247-251.
-
Sahithi Talasila BS*. Manifestations, Diagnosis, and Treatment of Pediatric Psychocutaneous Diseases. World Journal of Dermatology & Cosmetics. 1(3): 2024. WJDC.MS.ID.000512.
-
Pediatric psychocutaneous diseases, Psoriasis, Trichotillomania, Excoriation disorder, Acne excoriee, Psychiatric illnesses, Pathophysiology, Neuroendocrine system, Chronic stress, Skin microbiome
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.