Research Article
Research Article
Epidemiological Profile of Atopic Dermatitis in Infants in Dakar
Diatta Boubacar Ahy*, Mendy Patrice, Diop Khadim, Elharrar Loubna, Ndiaye Mame Téné, Diadie Saer, Diop Assane, Ndiaye Maodo, Diallo Moussa, Ly Fatimata and Niang Suzanne Oumou
Dermatologist, allergist Cheikh Anta Diop University of Dakar, Senegal
Professor Boubacar Ahy Diatta, MD dermatologist, allergist Cheikh Anta Diop University of Dakar, 30 Pasteur Road Dakar, Senegal.
Received Date: July 17, 2023; Published Date: July 28, 2023
Introduction
Atopic dermatitis is a common chronic inflammatory dermatosis in children with early-onset in infants [1]. It affects about 15-20% of children and 1-10% of adults in the general population [2]. It is the source of a costly economic cost of medical care and a significant deterioration in the quality of life of children and their parents [3]. It is essentially a disturbance of the sleep of the child and his parents by the pruritus and the cutaneous inflammatory symptoms as well as the bacterial complications observed [4]. Few works have been reported in the African literature on atopic dermatitis in infants. The objective of this study was to describe the epidemiological, clinical, therapeutic, and evolution aspects of atopic dermatitis in infants in Dakar.
Patients and Methods
We carried out a descriptive, analytical multicenter study in the three Dermatology departments in Dakar over a period of 6 months from June first to First November 2021. We included all infants aged between 0-30 months followed for atopic dermatitis. The diagnosis of atopic dermatitis was made according to the diagnostic criteria of the United Kingdom Working Party [5].
The presence of atopic equivalents such as asthma, allergic conjunctivitis, and allergic rhinitis. The existence of pruritus and cutaneous signs such as eczema on the folds, on the extension faces of the limbs, on the convex areas, cutaneous xerosis, and minor signs of atopy (periorbital hyperpigmentation, Dennie-Morgan’s double fold, keratosis pilaris, palmoplantar hyperlinearity, follicular eczema, achromic eczema, pulpitis, cheilitis). A sensitization to pneumoallergens was sought with a prick test pneumallergens.
Data entry and analysis were performed using Sphinx software and SPSS 20.0.
Results
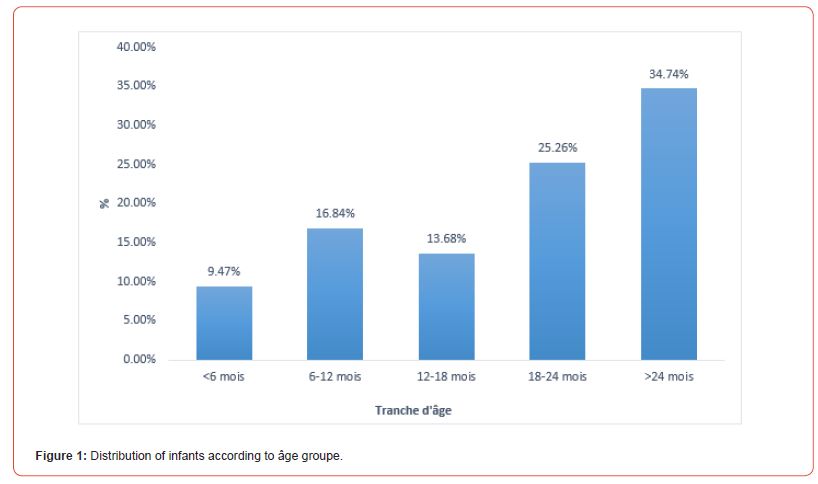
We identified 95 cases of atopic dermatitis in infants out of a cohort of 2160 children seen during this study period, ie a hospital frequency of 13.8%. They were 54 boys and 41 girls with an average age of 18 months with extremes of 2 months to 30 months. The 24-month age group was the most represented at 34.74% (n=33).
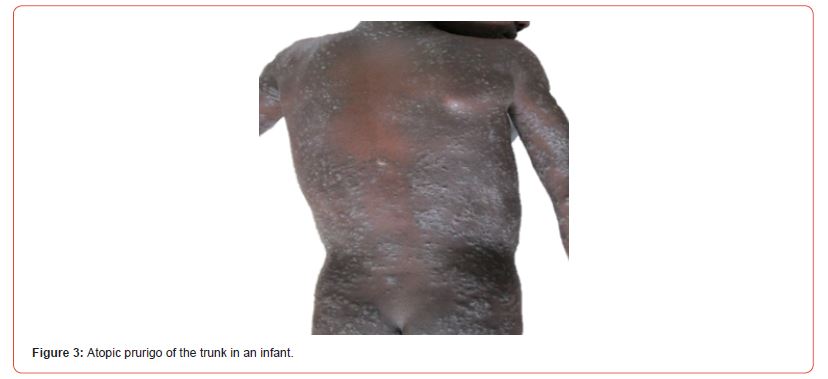
Familial atopy was noted in 96.7% of the type of allergic rhinitis, allergic conjunctivitis, and asthma. A food allergy was associated in 2 cases. Pruritus was noted in 60%. The skin lesions were acute eczema (Figure 2) in 54 cases, dyshidrotic eczema in 4 cases, cutaneous xerosis in 75 cases, keratosis pilaris in 30 cases, and prurigo (Figure 3) in 3 cases. The lesions were localized to the lower limbs in 38.95%, to the trunk in 36%, to the scalp in 33%, to the upper limbs in 28.42%, to the neck in 17%, and the face in 40.2%. Atopic dermatitis was associated with diaper contact dermatitis (Figure 4) in 15 cases, seborrheic dermatitis in 12 cases, psoriasis in one case, and vulvar vitiligo in one case. Infants had received topical corticosteroids in 80 cases and emollients in 89 cases. A therapeutic education was established with the parents in all cases. The evolution was marked by a complete remission in 81% with progressive infectious complications in 15.6%. It was a staphylococcal bacterial superinfection in 12.6%, oral candidiasis in 1.06%, herpetic superinfection in 1.06%, and scabies in 3.16%.


Discussion
We report 95 cases of atopic dermatitis in infants over a period of 6 months. Our study is particular by the high hospital frequency of 13% of atopic dermatitis despite the particular context of the Covid 19 pandemic during the study period.
Atopic dermatitis is on the rise in the world with a prevalence of 10% in previous studies [6]. Indeed, this phenomenon seems to be related to the industrialization processes associated with a change in the way of life of populations in urban areas [7]. In France, atopic dermatitis is also on the rise, affecting 10 to 20% of children in industrialized countries [7]. The prevalence of atopic dermatitis in Africa ranges from 16 to 18% [8]. The children were 18 months old on average with extremes of 2 months to 30 months with family atopy in 82%. The ISAAC study in Germany had shown that the existence of familial atopy increased the risk of the onset of AD and its persistence in adolescents [8]. As for food allergy, our study did not note a significant association with severe AD. However, many authors report the severity of atopic dermatitis in the event of an associated food allergy. In particular, a study in Germany which had shown that sensitization to food allergens such as cow’s milk and the chicken egg was significantly associated with the severity of AD in young children.
In our study, the clinical manifestations of atopic dermatitis were classic in infants with a predominance of cutaneous xerosis and skin fold eczema. However, severe symptoms were noted such as keratosis pilaris and diffuse prurigo. Keratosis pilaris was found in 8% of our patients. Its frequency was 38.8% in the Ivorian study [4] and 54.1% in Nigeria [9]. Pruritus is often suggestive, manifested by restlessness, twitching of the limbs, body trunk, and friction of the cheeks against the sheets and clothing [10, 11]. Depending on its intensity, it can affect the quality of the child’s sleep as much.
In addition, contact dermatitis of the seat was noted in 15.79% of infants. This could be favored by the fragility of the cutaneous barrier with the ground of atopy as well as the care used for the toilet of the seat which can increase the risks of poly sensitization [12]. All children received symptomatic treatment with topical corticosteroids and emollients with good clinical remission of skin lesions in 81% of cases. Staphylococcal complications were noted in 12.6%. These complications are also noted in many African series on AD [12].
Antimicrobial peptide deficiency, increased pH and trans epidermal water loss are the main factors contributing to the colonization and proliferation of Staphylococcus aureus on atopic skin [13]. Scabies represents 3.16% of the complications as it was characterized by a very itchy palmoplantar pustulosis with a chronic course. Appropriate treatment of scabies considerably improves the quality of life of atopic infants.
Conclusion
Atopic dermatitis in infants remains common in sub-Saharan Africa. It is particularly by its clinical severity, its chronicity, and its major retention on the quality of life of children and their parents. Good therapeutic education of the parents improves the prognosis and the experience of the disease by the children and finally prevents the infectious complications frequently noted in atopic skin.
Acknowledgement
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
-
Diatta Boubacar Ahy*, Mendy Patrice, Diop Khadim, Elharrar Loubna and Ndiaye Mame Téné. Epidemiological Profile of Atopic Dermatitis in Infants in Dakar. World Journal of Dermatology & Cosmetics. 1(1): 2023. WJDC.MS.ID.000503.
-
Inflammatory symptoms, Atopic dermatitis, Dermatology, Allergic conjunctivitis, Allergic rhinitis, Skin lesions, Food allergy, Atopy, Atopic skin
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.