Case Report
Case Report
Cutaneous Sarcoidosis Successfully Treated with Mycophenolate Sodium
Cagdas Boyvadoglu1 and Huseyin Serhat Inaloz2*
1Department of Dermatology, Ceyhan State Hospital, Adana, Turkey
2Department of Dermatology, University of Gaziantep Faculty of Medicine, Gaziantep, Turkey
Huseyin Serhat Inaloz, Department of Dermatology, University of Gaziantep Faculty of Medicine, Gaziantep, Turkey.
Received Date: April 06, 2023; Published Date: April 26, 2023
Abstract
Sarcoidosis is a multisystem disorder that can affect practically any organ of the body. Involvement of the skin is the most common extrathoracic manifestation of sarcoidosis. Glucocorticoids are the cornerstone of the treatment of sarcoidosis. The most commonly used disease-modifying antirheumatic drugs (DMARDs) for skin sarcoidosis include hydroxychloroquine, chloroquine, and methotrexate. So far as we know, no cases of cutaneous sarcoidosis treated with mycophenolate have been reported. Mycophenolate therapy stands out among other DMARDs due to its rapid onset of action and limited toxicity. Our case shows that cutaneous sarcoidosis can be successfully treated with mycophenolate therapy.
Keywords: Cutaneus Sarcoidosis; Mycophenolate sodium; Systemic therapy; Case report
Introduction
Sarcoidosis is a multisystem condition; it can affect virtually any organ in the body. Sarcoidosis can sometimes progress with only cutaneous findings. Due to the risk of systemic involvement, patients with cutaneous sarcoidosis should be checked regularly [1]. There are still no treatment guidelines for cutaneous sarcoidosis. Most of the experience in systemic therapy comes from treating patients with systemic sarcoidosis with cutaneous findings. Cases using mycophenolate sodium in the treatment of systemic sarcoidosis have been reported, but as far as we know, there is no case of cutaneous sarcoidosis treated with mycophenolate sodium in the literature. Here, we present a case of cutaneous sarcoidosis responding to mycophenolate sodium therapy.
Case Report
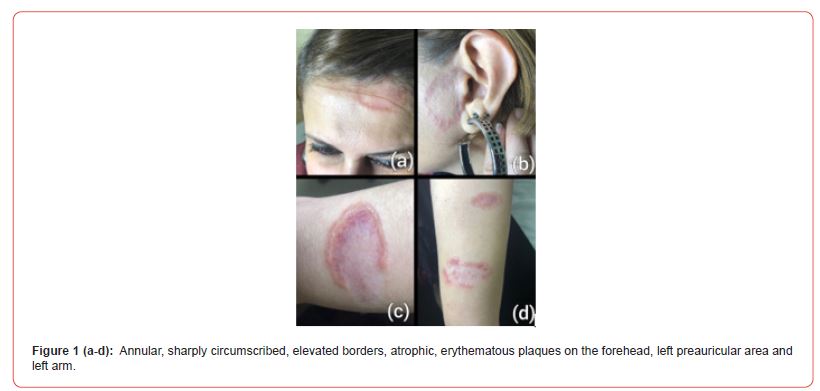
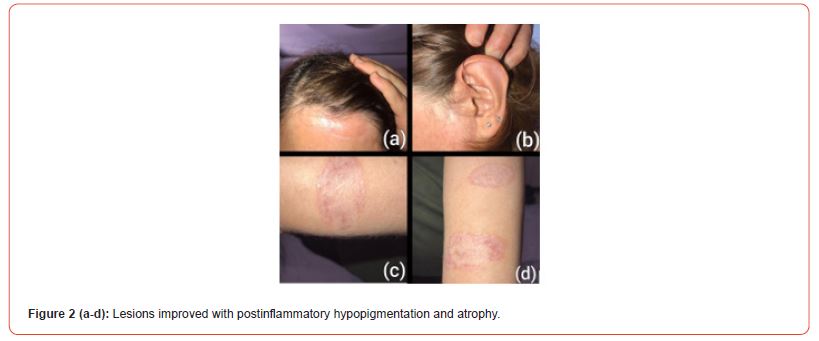
A 45-year-old female patient was diagnosed with sarcoidosis 7 years ago after a biopsy was taken from her facial lesion. No systemic involvement was observed in the examination of the patient who was consulted in pulmonology. First, systemic steroid therapy was started for the patient. Due to the recurrence of lesions during systemic steroid dose reduction, treatment was stospped. Partial improvement was observed in the lesions of the patient, who used systemic hydroxychloroquine (400 mg/day) and topical tacrolimus treatments for the next 4 years. Treatment was discontinued due to an increase in her lesions. Dermatologic examination revealed annular, sharply circumscribed, elevated borders, atrophic, erythematous plaques on the forehead, left preauricular area, and left arm (Figure 1). Oral mycophenolate sodium (1440 mg/day) treatment was initiated 3 years ago based on the current findings. It was observed that the patient’s lesions had improved six months after the start of the treatment, with postinflammatory hypopigmentation and atrophy (Figure 2). No systemic involvement was observed in the follow-up of the patient. In the patient receiving ongoing mycophenolate sodium treatment, no new lesions were noticed for three years. No side effects were observed in the follow-up.
Discussion
Skin involvement is the most common sign of sarcoidosis outside of the lungs. It can occur in up to one-third of patients. Treatment is not usually necessary because spontaneous remission occurs frequently. The cornerstone of sarcoidosis treatment is glucocorticoids. Patients who do not react to glucocorticoids or who experience severe side effects frequently get second- and thirdline therapy with glucocorticoid-sparing medicines and biologic therapies. Hydroxychloroquine, chloroquine, and methotrexate are some of the DMARDs that are most frequently prescribed for cutaneous sarcoidosis [1].
The medical literature has minimal evidence about the efficacy of mycophenolate mofetil in treating sarcoidosis. The vast majority of reported cases include extrapulmonary sarcoidosis (e.g., neurologic and ophthalmologic involvement). Mycophenolate mofetil does not seem to have any benefits over methotrexate in neurologic sarcoidosis, according to the collected data. The benefits of mycophenolate mofetil treatment rely on its rapid start of action and low hematological and infectious adverse effects. [2]. According to one trial, mycophenolate mofetil seems to give no further benefit to systemic sarcoidosis patients resistant to prior steroid-sparing medicines, although it may be advantageous to those intolerant of their previous therapy. [3].
As far as we know, no cases of cutaneous sarcoidosis treated with mycophenolate have been reported. Mycophenolate therapy stands out among other DMARDs due to its rapid onset of action and limited toxicity. Our case shows that cutaneous sarcoidosis can be successfully treated with mycophenolate therapy. For these reasons, we think that mycophenolate therapy is an agent that should be preferred primarily in the treatment of cutaneous sarcoidosis.
Acknowledgements
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflict of interest
The authors have no conflicts of interest to declare.
References
-
Cagdas Boyvadoglu and Huseyin Serhat Inaloz*. Cutaneous Sarcoidosis Successfully Treated with Mycophenolate Sodium. World Journal of Dermatology & Cosmetics. 1(1): 2023. WJDC.MS.ID.000501.
-
sarcoidosis, Glucocorticoids, hydroxychloroquine, toxicity, mycophenolate, hypopigmentation, atrophy
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.