 Research Article
Research Article
“Medical Adhesive Related Skin Injury” (MARSI), After Removal of Epidural Catheter Dressing”: Retrospective Audit
Mohammad Abdelmumen Abu Asal1*, Ban Alkanani2, Abdullah Fathi Nazal3, Muntaha Elayyan4 and Kristine Espinosa5
1Pain Management Nurse, HMC, Al Wakra Hospital, Qatar
2Arab board in Anesthesia and ICU Specialist Anesthesiologist in Wakra General Hospital, Qatar
3CCT Consultant Anesthesiologist and Pain Management in Wakra General Hospital, Qatar
4Pain Management, HMC, Al Wakra Hospital, Qatar
5Pain Management, HMC, Al Wakra Hospital, Qatar
Mohammad Abu Asal, Pain Management Nurse, HMC, Al Wakra Hospital, Qatar
Received Date: December 15, 2022; Published Date: January 04, 2023
Abstract
Background: It’s well known that after any surgical procedure, wound dressing, fixing epidural catheter, tubes or drains to the skin may lead to skin damage that may occur when medical adhesives are not selected, applied and/or removed properly. In mild cases, there may not be any visible trauma. But in other cases, the injury can be more serious, requiring additional treatment. This can be presented as blisters, skin sluffing, and rash which is called Medical Adhesive Related Skin Injury (MARSI).
MARSI is therefore could be a reason for postoperative morbidity, increase patient discomfort and sometime prolong hospital stay.
The purpose of this retrospective audit is to identify the possible causes of MARSI following removal of epidural dressing in Al Wakra Hospital and offers solutions that could help reducing the incident of MARSI.
Methods: The 67 patients have been reviewed in this audit. All patients were under pain management team care for epidural analgesia follow up after surgery.
This audit conducted in Al Wakra Hospital from Jan 2021 till end of August 2022 after acquiring Hamad Medical Corporation Research Ethical Committee approval, Pain team gathered data collected retrospectively from two sources: the patients file and pain management follow up record. The data were imported into a database (Microsoft Excel) and analysed by pain team staff.
Result: The MARSI developed in 18 patients of the 67 patients included in the audit. The result shown that there were two types of skin injury occurred: Tension injury / blister in 10 cases (56%) and Skin Stripping in eight cases (44%). Lumber region, neck and shoulder were the most common affected area among patients, they were (33%), (22%) respectively.
Conclusion: This audit suggests that MARSI occurs due to the material of dressing itself, component of adhesive material and mechanical stretching in addition to the condition of underlying skin.
Introduction
Epidural analgesia or Patient Controlled Epidural Analgesia (PCEA) is an effective technique to control acute postoperative pain and in some surgical procedures considered as gold standard postoperative pain management that proved to reduce complications, improve patient satisfaction and early mobilization.
Pain management is a cornerstone in any healthcare system, therefore, all healthcare professionals across many specialties are seeking to provide a high level of care in pain management documentation, evaluations, outcomes, and avoid complications. So, the healthcare sectors around the world has recognized the importance of The Acute pain Service and the role of specialize pain management nurses [24]. Medical Adhesive Related Skin Injury (MARSI) is “Skin damage related to the use of medical adhesive products such as tapes, wound dressings, stoma products, electrodes, medication patches and wound closure strips” [1].
MARSI can increase length of hospital stays, patient discomfort, negatively affects wound healing and increased risk of infection.
Skin is considered the first line of defence against any infection. So, loss of skin integrity put patients under risk of infection, nerve endings damage and pain from irritation [2].
Components of mechanical medical adhesive-related skin injury
Skin stripping: Removal of one or more layers of stratum corneum occurring following removal of adhesive tape or dressing, lesions are frequently shallow and irregular in shape and skin may appear shiny, open lesion may be accompanied by erythema and blister formation.
Tension injury or blister: Injury (separation of epidermis from the dermis) caused by shear force as a result of distension of skin under an unyielding adhesive tape or dressing, inappropriate strapping of tape or dressing during application or when a joint or other area of movement is covered with an unyielding tape.
Skin tear: Wound caused by shear, friction and/or blunt force resulting in separation of skin layers, can be partial or full thickness.
Components of MARSI due to Dermatitis
Irritant Contact Dermatitis: Non allergic contact dermatitis occurring due to chemical irritation; a well-defined area correlated with the area of exposure; may appear reddened, swollen and vesicles may be present; typically, of shorter duration.
Allergic dermatitis: Cell-mediated immunologic response to a component of tape adhesive or backing; typically appears as an area of erythematous, vascular, pruritic dermatitis corresponding to the area of exposure and/or beyond; persists for up to week.
Factors that could increase the risk of MARSI
Extreme of Age, Race, Dermatologic condition (skin diseases), dehydration, malnourishment, and underlying medical conditions (Diabetic, Renal problems, Low immunity) and skin infection [3-5].
Methodology
All epidural catheters were inserted inside the operation theatre under aseptic technique by anesthesiologist, skin sterilization used either:
ChloraPreP with active ingredients are (2%) chlorhexidine gluconate (CHG) and (70%) Isopropyl alcohol (IPA) Patient Preoperative Skin Preparation (26ml).
DuraPreP with active ingredients are Iodine Povacrylex (0.7% Available iodine) and Isopropyl Alcohol (74% w/v) Patient Preoperative Skin Preparation (26ml).
After 20sec, the insertion procedure of epidural catheter starts then the epidural catheter secured first with small sponge over the insertion site and with two pieces of Transparent Adhesive Waterproof Film (OPSITE 28 x 15cm).
The OPSITE is a transparent, adhesive film. The film is moisture vapor permeable, conformable, and extensible”. OPSITE dressing has many benefits such as keeping the wound environments moist, suitable for superficial skin injury, used as a secondary dressing, it is considered as water-resistant or waterproof items, and be able to use it over all part of the body [6].
On the other hand, there are many precautions that should be considered during the use of this item like keeping the patients under close observation and change the dressing daily.
Each patient is monitored and followed up by Clinical Specialist Nurse and two Pain Management Nurses, from the Recovery Room to the ward, the same team responsible for removal of epidural catheter and asses the skin condition after that.
Every patient with epidural catheter get assessed and examined by the acute pain team and the findings are documented using acute pain follow up record sheet both pre-and post-epidural catheter removal, then the documentation of each patient got uploaded to our electronic medical record software called Cerner.
The primary team is always notified after identifying the blister or skin redness to initiate proper management, while pain team keeps following the patients up until healing process of blister has been completed, then the progress updated in the patient’s record. Finally, all these information were updated on designated Excel spreadsheet; developed by pain team to meet their goals. All this information was confidentiality secured as per the hospital policy [9,10].
Data Collection Procedure
All the data were collected retrospectively from the patients file and pain management follow up record after the approval of the HMC Research Ethical Committee. data collection form (see Appendix A) is designed to collect necessary data needed for this audit [11].
The following information is recorded on the data collection form: Patient demographic data, Speciality, comorbidity, Number of days on PCEA, Categories of skin lesion, Number of blisters, Site of blister or lesion, Laterality, and other causes [12].
Results
During the period from Jan 2021 till end of August 2022 All anesthesiologists use standardized dressing technique.
Results showed:
i. Number of patients included in this audit are 67 patients (18) of them develop MARSI.
ii. All patients had their epidural catheter dressing on for one day or 48hrs only (Figure 1).
iii. Females were 51 (76.12%) compared to Males were 18 (23.88%) (See Figure 2).
iv. Two types of skin lesion noted Tension injury / blister 10 cases (56%) and Skin Stripping 8 cases (44%) (See Figure 3).
v. Lumber region, neck and shoulders were the most common affected area among patients (33%), (22%) respectively.
vi. The site of epidural insertion was the least common affected area with (6%) (Figure 4).
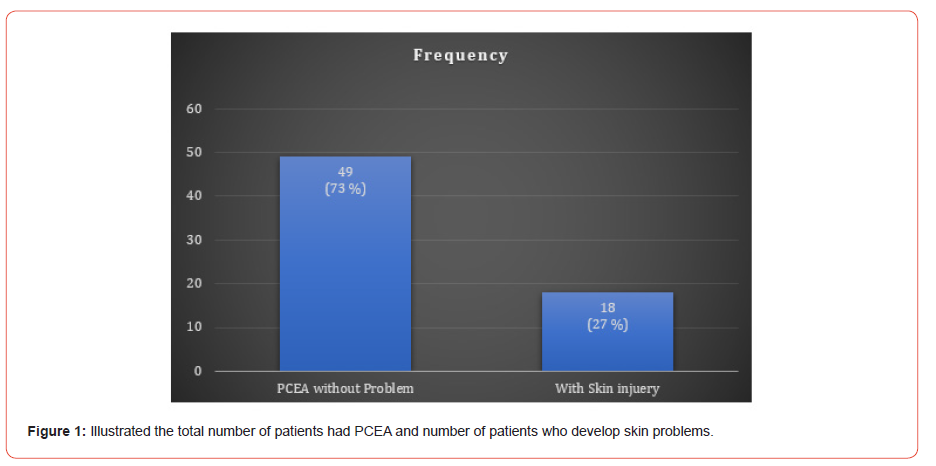
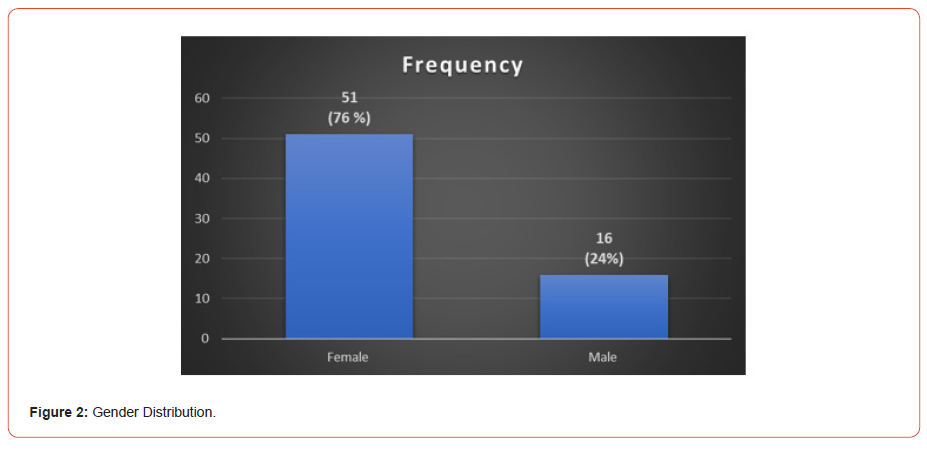
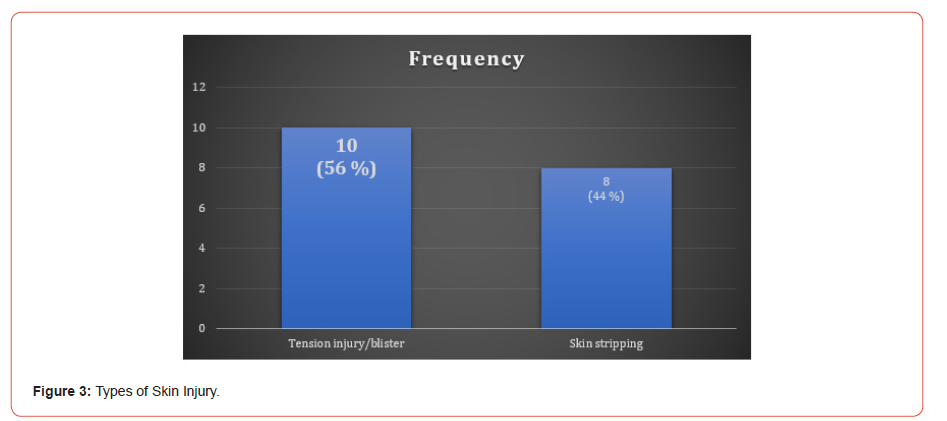
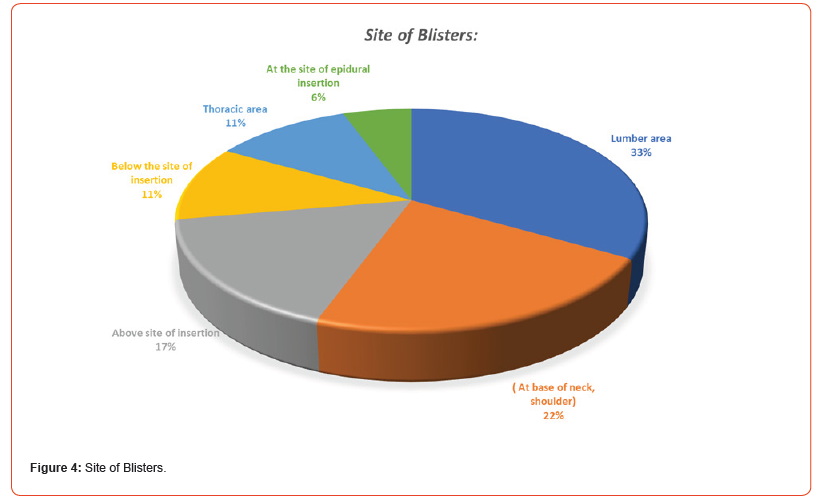
Figure 4 details the frequency distribution of the affected areas encountered. The most affected areas were lumbar region, neck and shoulder (respectively, 33% and 22%). Followed by the area above the epidural catheter insertion which was (17%). Thoracic area and inferior to the epidural catheter insertion where (11%) each. The least affected area was at the place of epidural catheter insertion which was (6%) [13-15].
Discussion
Investigating and analysing the possible cause of such complications pointed out to the application of OPSITE dressing use for epidural catheter fixation [16-18].
OPSITE dressing recommendation that it should be changed daily which will increase the load on nursing staff, increase cost , keep the patient under stress, prolong hospital stay and finally frequent change of dressing will lead to a high incident rate of epidural catheter migration and dislodgment. There is no need to mechanically stretch the dressing during application because this may cause skin to wrinkle and fold under. It may also result in blistering or skin-stripping when the dressing is removed [19-24].
Conclusion
We concluded that MARSI may be caused by the following predisposing factors: putting the dressing on wet skin, stretching, leaving the dressing on for an excessive amount of time, patient having a condition like diabetes or a weakened immune system, having a skin condition like dry skin or another skin disease, being bedridden for an extended period of time, which may affect the circulation at the catheter site, and not changing the dressing every day.
Limitation
I. Number of patients is limited.
II. Most of the patients had their epidural catheter removed after 24hrs as per surgeon’s decision
Recommendation
i. Use the barrier film before applying the dressing.
ii. Make adequate skin preparation.
iii. Dryness should be permitted after sterilisation.
iv. Use swap stick close to site of insertion and spray the back.
v. To keep 5–15cm away from the skin surface during spraying and try to use a sweeping motion.
vi. Ensure that the area becoming dry, after about 30 seconds before applying the adhesive tape.
vii. Do not over stretch the dressing or the skin under during dressing.
viii. Try to use the latest or up to date brand of dressing
ix. Daily assessment of patient back by pain team.
x. Finally, do not attempt to remove an adhesive tape fast and vertical, it is not only more painful, but it also creates a higher skin force than slow removal.
xi. More studies need to be done involving larger number of patients.
xii. Detailed and careful interrogative studies are needed to determine the cause and the mechanism that leads to medical adhesive related injuries MARS
Acknowledgement
The authors are grateful to all members for their valuable contributions in the development of this manuscript: Dr. Almunzer Abduljalil Zakaria and Dr. Sara Morhaf.
Conflict of Interest
We do not have an affiliation; either financial or non-financial, with any pharmaceutical, medical device, or communications and event planning company. We have not received any funding from pharmaceutical or medical device organization.
References
- McNichol L, Lund C, Rosen T, Gray M (2013) Medical adhesives and patient safety: state of the science consensus statements for the assessment, prevention, and treatment of adhesive- related skin injuries. Journal of Wound Ostomy & Continence Nursing 40(4): 267-281.
- Hadfield G, De Freitas A, Bradbury S (2019) Clinical evaluation of a silicone adhesive remover for prevention of MARSI at dressing change. Journal of Community Nursing 33(3).
- Berg L, Martinez JL, Serena TE, Dhoonmoon L, Ousey K (2019) Meeting report: promoting wound healing by optimizing dressing change frequency. Wounds International 10(3): 44-51.
- Bootun R (2013) Efects of immunosuppressive therapy on wound healing. Int Wound J 10(1): 98-104.
- Farris MK, Petty M, Hamilton J, Walters SA, Flynn MA (2015) Medical adhesive-related skin injury prevalence among adult acute care patients: a single-center observational study. Journal of Wound Ostomy & Continence Nursing 42(6): 589-598.
- Fumarola S, Allaway R, Callaghan R, Collier M, Downie F, Geraghty J, Voegeli D (2020) Overlooked and underestimated: medical adhesive-related skin injuries. Journal of Wound Care 29(Sup3c): S1-S24.
- Gerhardt LC, Lenz A, Spencer ND, Münzer T, Derler S (2009) Skin–textile friction and skin elasticity in young and aged persons. Skin Research and Technology 15(3): 288-298.
- Heale M (2017) Dressing change tips every clinician should know to help prevent Marsi.Wound Source.
- Kelly-O Flynn S, Mohamud L, Copson D (2020) Medical adhesive-related skin injury. British Journal of Nursing 29(6): 20-26.
- Leu HJ (1994) Micro morphologic changes in the skin in primary and secondary (post-thrombotic) chronic venous insufficiency. [Article in German]. Wien Med Wochenschr 144(10-11):201-4.
- Lund CH, Tucker JA (2003) Adhesion and newborn skin. Neonatal skin: structure and function. (2nd), New York, NY: Marcel Dekker, pp. 299-324.
- Miller RD (2005) Anaesthesia. New York: Churchill Livingstone
- Parodi A, Castello M, Corbetta S (2018) Skin and diabetes: an experts’ opinion from the Italian diabetologists and dermatologists of the DiaDex group. G Ital Dermatol Venereol 153(5): 649–658.
- Resnick B (1993) Wound care for elderly. Geriatr. Nurs. (Lond) 14: 26-29.
- Rod Brouhard EMTP (2022) How to treat and prevent skin tears. Verywell Health.
- https://www.verywellhealth.com/treatment-of-skin-tears-1298233
- Royal College of Anaesthetists, Royal College of Nursing, Association of Anaesthetists of Great Britain and Ireland, British Pain Society and European Society of Regional Anaesthesia and Pain Therapy (2004) Good Practice in the Management of Continuous Epidural Analgesia in the Hospital Setting.
- Shannon ML, Lehman CA (1996) Protecting the skin of the elderly patient in the intensive care unit. Critical care nursing clinics of North America 8(1): 17-28.
- Smith-nephew (2022) OPSITE Transparent Waterproof Film | Smith & Nephew - US Professional.
- Smith MA, Jones NM, Page SL, Dirda MP (1984) Pressure-sensitive tape and techniques for its removal from paper. Journal of the American Institute for Conservation 23(2): 101-113.
- Stephen-Haynes J, Bielby A, Searle R (2011) Putting patients first: reducing the human and economic costs of wounds. Wounds UK 7: 47–55.
- Weetman C, Allison W (2006) Use of epidural analgesia in post-operative pain management.Nursing Standard 20(44): 54-64.
- Van de Velde-Kossmann KM (2018) Skin examination: an important diagnostic tool in renal failure patients. Blood Purif 45 (1–3): 187-193.
- Kaasalainen, S., Wickson Griffiths, A., Akhtar Danesh, N., Brazil, K., Donald, F., et al. (2016) The effectiveness of a nurse practitioner-led pain management team in long-term care: A mixed methods study. International Journal of Nursing Studies 62: 156-167.
-
Mohammad Abdelmumen Abu Asal*, Ban Alkanani, Abdullah Fathi Nazal, Muntaha Elayyan and Kristine Espinosa. “Medical Adhesive Related Skin Injury” (MARSI), After Removal of Epidural Catheter Dressing”: Retrospective Audit. Sci J Research & Rev. 3(4): 2023. SJRR.MS.ID.000566.
Skin Injury, Epidural analgesia, Dehydration, Malnourishment, Diabetic, Renal problems, Low immunity
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






