 Research Article
Research Article
Using Phage T4 as a Model in Assessing Face Masks in Preventing SARS-CoV-2 Transmission
Vy Huyen1, Daniel P Herman2 and Sasha A. Showsh2*
1Department of Biological Sciences, University of Wisconsin – Milwaukee, USA
2Department of Biology, University of Wisconsin – Eau Claire, USA
Sasha A Showsh, Department of Biology, University of Wisconsin - Eau Claire, Eau Claire, WI 54702-4004, USA.
Received Date:September 26, 2022; Published Date:October 10, 2022
Abstract
\The Center for Disease Control and Prevention and World Health Organization both recommend the use of face masks as one of the methods to reduce the transmission of severe acute respiratory syndrome virus 2 (SARS-CoV-2), the causative agent of COVID-19 (corona virus disease 2019). Here, we tested various masks for their ability to prevent transmission of droplets/aerosols after challenge from a spray bottle. We used phage T4 as a model for SARS-CoV-2 transmission. We found that two- and three-layered masks provided a 99.9% reduction in transmission of phage T4. The popular single-layered neck gaiter was not as effective as it provided a 93.9% reduction in transmission under these conditions, a 6% decrease in protection compared to two- and three-layered masks. This data will provide the public with information on selecting the best available masks for protection against transmission of droplets/aerosols in the COVID-19 (corona virus disease 2019) pandemic.
Keywords: Facemasks; COVID-19; SARS-CoV-2; Bacteriophage
Abbreviations:SARS-CoV-2; Severe acute respiratory syndrome virus 2; COVID- 19: Corona virus disease 2019
Introduction
COVID-19 (corona virus disease 2019) is a contagious disease caused by severe acute respiratory syndrome virus 2 (SARS-CoV-2) first identified in Wuhan, China in December 2019 [1]. SARS-CoV-2 is transmitted primarily by exposure to infectious respiratory droplets. Transmission of the virus can occur through inhalation of respiratory droplets/aerosols or by contamination of mucous membranes with virus containing fluids [2]. Since the original outbreak, the disease has spread and is now a global pandemic with over 596 million cases resulting in over 6.4 million deaths [3]. There have been over 93.6 million cases of COVID-19 in the US with over 1 million deaths [3]. To control the spread of COVID-19 by infectious droplets, the Centers for Disease Control and Prevention (CDC) recommends the use of face masks, among other preventative measures [4]. There are many different masks with different fabric components available on the market that reduce the expo sure to aerosols at different levels. The aerosol filtration efficiency is influenced by the type of fabric used in cloth masks [5]. There is also information on specialty masks (N95) and their effectiveness against the spread of COVID-19 [6].
In this experiment we tested the efficacy of commonly available masks in preventing transmission of droplets/aerosols. We specifically wanted to look at some common cloth masks available online to determine how effective they are in preventing the transmission of viruses. We used phage T4 as a model for SARS-CoV- 2 transmission due to size similarity. Phage T4 is approximately 200nm [7], which is close to the average size of 150nm for the SARS-CoV-2 virus [8]. Moreover, phage T4 is not a human pathogen and thus did not require additional laboratory safety requirements that are necessary when working with human pathogens.
Materials and Method
Bacterial strain and phage
For the phage assay we used a laboratory strain of Escherichia coli K12. Overnight cultures of E. coli were grown at 37 ᵒC in Todd- Hewitt broth (THB, BBL Cockeysville, MD). Coliphage T4 (T4r+, Lot No. A4-327), was purchased from Carolina Biological Supply (Burlington, NC). The sterile peptone broth suspension that was used to simulate the droplets/aerosols had an initial titer of 5.3X109 PFU/ ml (Plaque Forming Units/milliliter) as indicated by the supplier.
Phage Assay
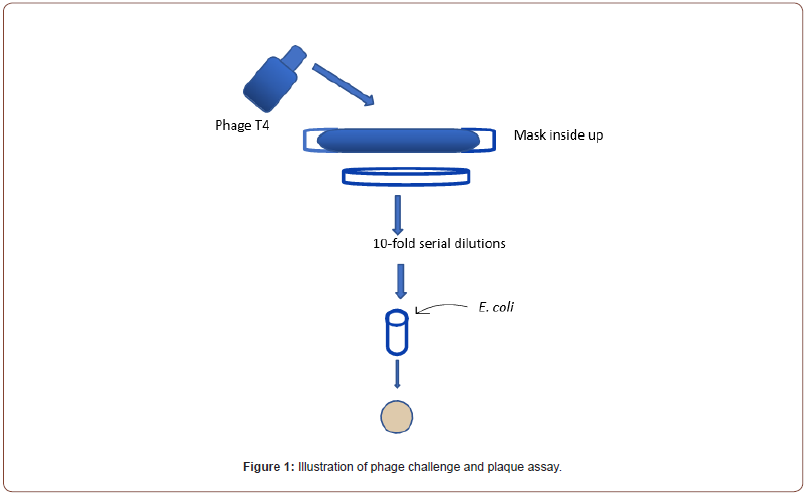

A plaque assay (Figure 1) for phage virus titer was performed to quantify the number of phage in the 3ml THB sample (in the 60 x 16 mm petri dish) following the challenge from the spray bottle. For each trial, serial ten-fold dilutions were performed on the 3ml samples. After performing the dilutions, 100ml was taken from each dilution and added to 5ml soft top agar (Tryptic Soy Broth with 0.7% agar Beckton Dickson Co., Sparks, MD) that was inoculated with 2 drops from an overnight culture of E. coli. The contents were gently mixed and poured onto Tryptic Soy Agar (TSA) plates. The plates were allowed to solidify and were incubated at 37 ᵒC for 24 hours before counting plaque forming units (PFU) formed in the bacterial lawn.
Mask challenge
Table 1 lists the masks that were evaluated for their ability to block phage containing droplets/aerosols generated by a 33ml spray bottle (Insta Clears, Clarity Brand Products, Cleveland OH). Figure 1 represents the mask challenge setup. Each mask was placed over a 60 x 16mm plastic petri dish containing 3ml sterile THB. Phage were sprayed onto the mask side that is normally in contact with the mouth. The spray bottle was placed 5cm away from the mask. Two full squirts were used for each challenge. The control sample was challenged in the same way but without the mask over the petri dish. After the mask challenge, the THB content in the 60 x 16mm petri dish was used for the phage assay as described. Each mask challenge and control were performed three different times.
Mask efficiency
We used phage T4 as a model for SARS-CoV-2 transmission through different face masks. To quantify the efficiency of masks on the transmission of phage we used the following formula:

Results
Mask efficiency
Several masks with different designs and compositions were analyzed for their ability to prevent the spread of phage T4. In this experiment, phage T4 was used as model for SARS-CoV-2 transmission. The data are presented in Table 2. Based on three different trials the spray bottle was delivering on average 2.8 x 108 PFU/ml as determined from the control trials. That was approximately a 10- fold decrease from the concentration as reported by the manufacturer. Moreover, the concentration of aerosolized phage was very consistent between trials indicating a consistent dispensing method. All the masks, except the neck gaiter were able to reduce the transmission of phage T4 by 99.99% under these conditions. Interestingly, both Whitestone mask and Whitestone modified with paper insert had the same reduction (99.9%) in transmission under these conditions. The neck gaiter was the least effective as it reduced phage transmission by 93.93%. This represents an increase in transmission by 6% as compared to the other masks tested.


1N. A. = Not Applicable.
Discussion
In this experiment we used phage T4 as a model for SARS-CoV-2 transmission. We demonstrated that wearing masks provides some degree of protection against the transmission of phage. The best protection results from the use of multi-layered masks that were able to reduce transmission of phage T4 by 99.9%. Interestingly, placing a paper towel between two layers did not affect the final transmission of the phage under these conditions. It may be that this single-fold paper towel does little to prevent transmission, or the size of the paper towel did not cover the whole spray area. Repeat ing the experiment using only the single- fold paper towel would provide data on the efficacy of the single-fold paper towel alone. The use of single- layer protection, such as the neck gaiter, resulted in reduction of phage transmission by 93.9%. This represents a 6% increase over the transmission observed for multi-layer masks. The data demonstrate that face masks are an effective method in reducing the transmission of phage T4. Moreover, to achieve maximal protection, masks with multiple layers are more effective than ones with a single layer.
Conclusion
The experimental results demonstrate that facemasks and neck gaitors are effective at limiting the aerosol transmission of viruses. All facemasks tested provided a 99% reduction in phage transmission under the test conditions while the neck gaitor only achieved a 96% reduction in phage transmission. While mask mandates are not in place in most locations in the US, situational use of facemasks in crowded situations can help to limit the spread of viruses, such as SARS-CoV-2, and contribute to enhanced public health.
Acknowledgment
Support for this research was provided by the University of Wisconsin – Eau Claire Office of Research and Sponsored Programs.
Conflict of Interest
The authors do not have any conflicts of interest related to this research.
References
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, et al. (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 588(7836): E6.
- Buonanno G, Stabile L, Morawska L (2020) Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ Int 141: 105794.
- Johns Hopkins University of Medicine. Corona Virus Resource Center.
- Schuchat A (2021) Summary of Guidance Review. CDC.
- Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, et al. (2020) Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Masks. ACS Nano 14(5): 6339-6347.
- Bartoszko JJ, Farooqi MAM, Alhazzani W, Loeb M (2020) Medical masks vs N95 respirators for preventing COVID-19 in healthcare workers: A systematic review and meta-analysis of randomized trials. Influenza Other Respir Viruses 14(4) :365-373.
- Rao VB, Black LW (2010) Structure and assembly of bacteriophage T4 head. Virol J 7: 356.
- Neuman BW, Adair BD, Yoshioka C, Quispe JD, Orca G, et al. (2006) Supramolecular architecture of severe acute respiratory syndrome coronavirus revealed by electron cryomicroscopy. J Virol 80(16): 7918-7928.
-
Vy Huyen, Daniel P Herman and Sasha A. Showsh*. Using Phage T4 as a Model in Assessing Face Masks in Preventing SARSCoV- 2 Transmission. Sci J Biol & Life Sci. 2(4): 2022. SJBLS.MS.ID.000542. DOI: 10.33552/SJBLS.2022.02.000542
-
Biology; Facemasks; COVID-19; SARS-CoV-2; Bacteriophage; SARS-CoV-2 Transmission; Droplets; Aerosols; Escherichia coli; Biological Supply; Human pathogens; Reduction
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






