 Review Article
Review Article
Telemedicine and Remote Patient Monitoring: Transforming Healthcare Delivery
Awez A Sikkalgar1 Kalpesh R Yeole1 Naina Chaurasiya1 Devendra K Jadhav2 Zubair Saghir Ahmed Shaikh2 and Sagar A More1
1Department of Pharmacology, Shri Vile Parle Kelavani Mandal’s Institute of Pharmacy, Dhule 424001, Maharashtra, India
2Department of Pharmaceutics, P.S.G.V.P. M’s College of Pharmacy, Shahada 425409, Maharashtra, India
Sagar A More, Department of Pharmacology, Shri Vile Parle Kelavani Mandal’s Institute of Pharmacy, Dhule 424001, Maharashtra, India
Received Date: June 24, 2025; Published Date: July 08, 2025
Abstract
Telemedicine and Remote Patient Monitoring (RPM) are revolutionizing modern healthcare by enhancing accessibility, improving patient outcomes, and reducing costs. This chapter explores the transformative potential of these technologies, driven by advancements in wearable devices, IoT integration, and AI-powered analytics. It delves into the technological infrastructure enabling telemedicine and RPM, including communication platforms, wearable devices, and data management systems. The chapter examines clinical applications across various specialties, emphasizing their role in chronic disease management, post-operative care, and rural healthcare. Benefits such as improved patient engagement, reduced healthcare costs, and enhanced clinical decision-making are discussed. It also addresses regulatory hurdles, privacy concerns, and technological barriers. The evolving landscape of reimbursement policies and their impact on adoption is explored. Case studies illustrate successful implementations and lessons learned. The chapter concludes by discussing future trends, including AI integration, personalized medicine, and the role of telemedicine and RPM in global health initiatives. We emphasize the importance of evidence-based practice and the need for ongoing research to optimize these technologies’ use in healthcare delivery. By providing a comprehensive overview, this work aims to inform healthcare providers, policymakers, and researchers about the opportunities and implications of telemedicine and RPM..
Keywords:Artificial intelligence; modern healthcare; telemedicine; remote patient monitoring
Introduction
Telemedicine and RPM have emerged as transformative forces in healthcare delivery, particularly after the COVID-19 pandemic. These technologies leverage information and communication technology to facilitate healthcare services over distances, thereby enhancing access to medical care for patients who may otherwise face barriers due to geographical, physical, or economic constraints. The historical roots of telemedicine can be traced back to the 1980s when it was primarily utilized in disaster medicine and rural healthcare settings. However, the rapid advancement of technology, including the internet, mobile devices, and artificial intelligence (AI), has significantly expanded the scope and effectiveness of telemedicine, making it a vital component of modern healthcare systems [1,2].
Historically, telemedicine began with simple telephone consultations and has evolved into sophisticated systems that integrate various technologies for remote monitoring and patient engagement. The development of implantable cardiac devices, such as pacemakers and defibrillators, has particularly benefited from RPM, allowing for continuous monitoring of patient’s heart health without requiring frequent in-clinic visits [3]. Studies have demonstrated that RPM can significantly reduce hospital visits and healthcare costs while maintaining or even improving patient outcomes [4]. For instance, the Home Guide Registry confirmed that continuous remote monitoring of cardiac implantable electronic devices (CIEDs) can be effectively integrated into standard clinical practice, reducing patient visits by nearly 50%.
The importance of telemedicine and RPM in healthcare cannot be overstated. These modalities have improved patient outcomes, particularly for individuals with chronic conditions. For instance, studies indicate that telemedicine can effectively manage chronic diseases, enhance patient satisfaction, and reduce healthcare costs by minimizing the need for in-person visits [5]. Moreover, telemedicine has proven invaluable for older adults and those residing in rural areas, where access to healthcare facilities is often limited. By offering convenience and flexibility, telemedicine facilitates more consistent management of chronic conditions, ultimately leading to improved health outcomes [5,6].
The COVID-19 pandemic catalyzed the widespread adoption of telemedicine, as healthcare systems sought to maintain continuity of care while adhering to social distancing measures. This shift has underscored the potential of telemedicine to alleviate the burden on overtaxed healthcare systems and improve access to care for vulnerable populations [7]. This chapter aims to provide a comprehensive overview of the current state of telemedicine and RPM, highlighting their historical evolution, significance in contemporary healthcare, and the challenges that lie ahead. It will explore the various telemedicine applications, including virtual consultations, remote monitoring of chronic diseases, and the integration of advanced technologies such as mobile health applications (mHealth) and wearable devices. Furthermore, the chapter will address the barriers to effective telemedicine implementation, such as technological disparities, privacy concerns, and regulatory challenges [8,9]. By examining these aspects, the chapter aims to contribute to the ongoing discourse on how telemedicine can be optimized to enhance healthcare delivery and patient outcomes.
Technological Foundations of Telemedicine and RPM
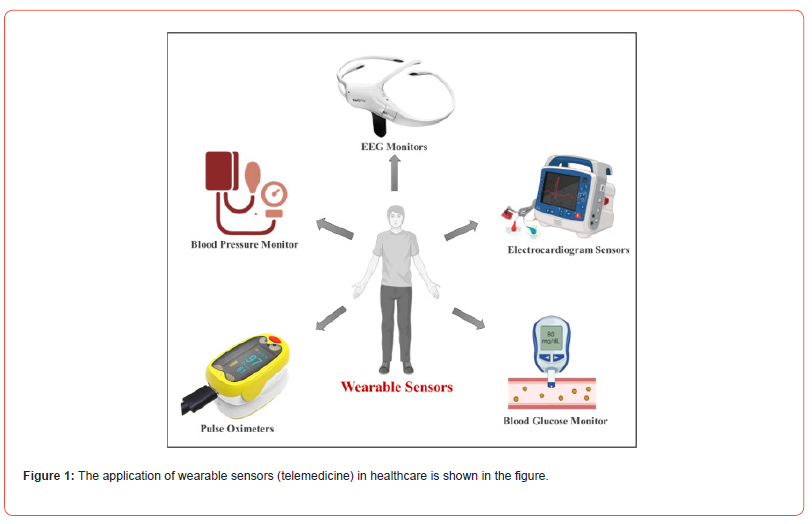
Telemedicine and RPM have revolutionized healthcare delivery by leveraging advanced technologies to enhance patient care, accessibility, and efficiency. The technological foundations of telemedicine and RPM encompass various components, including communication platforms, wearable devices, AI, cloud computing, and security measures, all crucial for effective remote healthcare delivery. Communication platforms are integral to telemedicine, facilitating real-time interactions between healthcare providers and patients. Video conferencing tools enable virtual consultations, allowing healthcare professionals to assess and diagnose patients remotely. The rise of mHealth has further enhanced this capability, providing patients with tools to manage their health and communicate with providers seamlessly. Asynchronous telehealth, or “store-and-forward” telehealth, allows for the collection and transmission of patient data, such as electronic health records (EHRs) and images, which can be reviewed later by healthcare professionals, thus improving efficiency and accessibility [10,11]. Wearable devices and the Internet of Things play a pivotal role in RPM by enabling continuous health monitoring. These devices collect vital signs and health metrics, which are then transmitted to healthcare providers for analysis. Integrating IoT with wearable technology allows real-time data collection and monitoring, significantly enhancing patient management, especially for chronic conditions [12,3]. For instance, smart devices can alert healthcare providers to critical patient condition changes, facilitating timely interventions [14,15]. The basic details of telemedicine as shown in Figure 1.
AI and data analytics transform remote healthcare by enabling predictive analytics and personalized medicine. AI algorithms can analyze vast amounts of data collected from wearable devices and EHRs to identify trends and predict health outcomes. This capability enhances decision-making processes, allowing healthcare providers to tailor interventions based on individual patient needs [16,17]. Moreover, AI-driven tools can assist in diagnosing conditions and recommending treatment plans, thereby improving the overall quality of care [18]. Cloud computing is the backbone of telemedicine and RPM, providing data storage, management, and sharing infrastructure. It enables healthcare providers to access patient data from anywhere, facilitating collaboration and continuity of care [19]. The scalability of cloud solutions allows healthcare organizations to manage large volumes of data efficiently, ensuring that patient information is readily available for analysis and decision-making [20]. Furthermore, cloud computing supports integrating various telemedicine services, enhancing the healthcare delivery system [21].
The successful implementation of telemedicine and RPM necessitates robust infrastructure and reliable connectivity. Highspeed internet access is essential for seamless communication and data transfer between patients and healthcare providers. In rural and underserved areas, improving connectivity can significantly enhance access to telemedicine services, bridging the gap in healthcare delivery [22,23]. Bandwidth considerations are critical, as high-quality video consultations require substantial data transmission capabilities to ensure clear communication without interruptions [17]. Security and privacy are paramount in telemedicine, given the sensitive nature of health data. Implementing stringent security measures, such as encryption and secure access protocols, is essential to protect patient information from unauthorized access [24,25]. Additionally, compliance with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) is crucial to ensure patient data is handled securely and ethically. By prioritizing security, healthcare providers can foster patient trust, encouraging the adoption of telemedicine services [26,27].
Clinical Applications of Telemedicine and RPM
Chronic diseases such as diabetes, hypertension, and cardiovascular diseases are prevalent globally, necessitating effective management strategies. Telemedicine facilitates continuous monitoring and management of these conditions, allowing healthcare providers to track patients’ health metrics remotely. For instance, RPM technologies enable real-time data collection on blood glucose levels in diabetic patients, which can lead to timely interventions and adjustments in treatment plans. Studies have shown that patients with chronic conditions who engage in telemedicine report higher satisfaction levels and improved health outcomes than traditional care methods [28,29]. Furthermore, telemedicine reduces the need for frequent in-person visits, which can be burdensome for patients with mobility issues or those living in remote areas [30].
Telemedicine offers innovative solutions for post-operative care, and rehabilitation is critical to patient recovery. Remote monitoring allows healthcare providers to assess recovery progress without necessitating patient visits to healthcare facilities, which can be particularly advantageous during the COVID-19 pandemic [31]. For instance, patients recovering from surgery can use telemedicine to report symptoms, receive guidance on rehabilitation exercises, and have their progress monitored by healthcare professionals. This approach has been associated with reduced readmission rates and improved patient satisfaction [32]. Additionally, telemedicine facilitates access to rehabilitation services for patients in rural areas, where specialized care may not be readily available [33].
Telemedicine is vital in addressing healthcare disparities in rural and underserved populations. Many individuals in these areas face significant barriers to accessing healthcare, including long travel distances and limited availability of specialists [34,35]. Telemedicine bridges this gap by providing remote access to healthcare services, enabling patients to consult with specialists without the need for extensive travel [36]. For example, telemedicine initiatives in rural India have demonstrated a significant reduction in maternal mortality rates by improving access to prenatal care. Furthermore, telemedicine has been shown to reduce overall healthcare costs for patients in rural settings, as it minimizes travel expenses and time away from work [37]. The successful implementation of telemedicine in these communities requires ongoing investment in technology and infrastructure to ensure equitable access [38].
The integration of telemedicine into mental health services has significantly transformed care delivery. Teletherapy and remote counseling have become increasingly popular, allowing patients to receive mental health support from the comfort of their homes [39]. This modality has been particularly beneficial for individuals in rural areas, where mental health resources may be scarce [40]. Studies indicate that teletherapy is as effective as in-person therapy for many patients, leading to improved access to care and reduced stigma associated with seeking help. Furthermore, telemedicine facilitates ongoing support for patients with chronic mental health conditions, enabling regular check-ins and adjustments to treatment plans as needed [41].
Benefits of Telemedicine and RPM
Telemedicine and RPM have emerged as transformative components of modern healthcare delivery, particularly during the COVID-19 pandemic. These technologies enhance patient care and improve healthcare efficiency, accessibility, and costeffectiveness. This chapter discusses the multifaceted benefits of telemedicine and RPM, supported by recent research findings. One of the primary advantages of telemedicine is its ability to provide timely and accessible healthcare services. By facilitating virtual consultations, telemedicine reduces the need for in-person visits, minimizing patient travel time and associated costs. Walker et al. highlight that remote monitoring in peritoneal dialysis supports timely care and fosters patient education, which is crucial for chronic disease management [42]. Similarly, the use of RPM in cardiac care has been shown to enhance patient outcomes by enabling early detection of arrhythmias and device malfunctions, leading to timely interventions [43]. The COVID-19 pandemic accelerated the adoption of these technologies, demonstrating their effectiveness in maintaining continuity of care while adhering to social distancing guidelines [44].
Moreover, telemedicine and RPM significantly enhance patient engagement and self-management. In real-time, patients with remote monitoring devices can track their health metrics, such as blood pressure and heart rate. This capability empowers patients to take an active role in their healthcare, fostering a sense of autonomy and responsibility. Research by El-Rashidy et al. emphasizes that RPM systems facilitate the collection of vital signs, enabling healthcare providers to make informed decisions promptly [45]. Additionally, smartphone-assisted monitoring has been shown to improve communication between patients and healthcare providers, further enhancing patient satisfaction and adherence to treatment plans [46].
The economic implications of telemedicine and RPM are also noteworthy. By reducing the frequency of in-person visits, healthcare systems can lower operational costs while reallocating resources to more critical areas of patient care. Hwang and Bae report that remote monitoring of CIEDs not only decreases unnecessary outpatient visits but also enhances patient satisfaction [47]. Furthermore, integrating RPM in chronic disease management has been associated with reduced healthcare utilization, as evidenced by studies showing lower hospitalization rates among patients engaged in remote monitoring programs. This economic efficiency is particularly relevant in resource-limited settings, where the cost of care can be a significant barrier to access [48].
In addition to economic benefits, telemedicine and RPM contribute to improved healthcare outcomes. For instance, a study on remote monitoring of implantable cardioverter defibrillators (ICDs) found that it led to more rapid clinical event detection and a reduction in inappropriate shocks, which are critical for patient safety [47]. Similarly, Goto et al. reported that remote monitoring in pacemaker patients provided a sense of safety comparable to traditional follow-ups while also facilitating early detection of potential issues [43]. These findings underscore the potential of telemedicine and RPM to enhance clinical outcomes through proactive monitoring and timely interventions.
However, the implementation of telemedicine and RPM is not without challenges. Data privacy concerns, technological barriers, and the need for adequate training for patients and healthcare providers can hinder the effective use of these technologies. Lindsay et al. note that the lack of understanding and support for the necessary work involved in remote monitoring can impede its routine adoption in clinical practice [49]. Additionally, disparities in digital literacy among patients can affect the overall effectiveness of RPM interventions, as highlighted by research indicating that younger, more educated individuals are more likely to benefit from remote monitoring [50].
Despite these challenges, the potential benefits of telemedicine and RPM are substantial. The ongoing evolution of healthcare technology and increasing acceptance of virtual care models suggest a promising future for these modalities. Integrating advanced technologies such as the Internet of Things (IoT) and AI into telemedicine and RPM systems can enhance their effectiveness and user-friendliness [51]. For instance, IoT-enabled devices can provide continuous monitoring and real-time feedback, making it easier for patients to manage their health conditions effectively.
Challenges and Barriers
The advent of telemedicine and RPM has revolutionized healthcare delivery, particularly during the COVID-19 pandemic. However, several challenges and barriers impede its widespread adoption and effectiveness. These challenges include regulatory and legal issues, technological limitations, and patient and provider adoption barriers. One of the primary challenges in telemedicine is navigating the complex regulatory landscape. Licensing and cross-border telemedicine practices pose significant hurdles. Each jurisdiction has licensing requirements, which complicate care provision across state or national lines. During the COVID-19 pandemic, many countries relaxed regulations to facilitate telemedicine use, but these changes were often temporary and varied significantly across regions [52,53]. The lack of a standardized framework can lead to confusion among healthcare providers and patients alike, as they may be unsure about the legality of telemedicine practices in different locations.
Moreover, compliance with data protection regulations such as HIPAA in the United States and GDPR in Europe is critical yet challenging. Telemedicine involves the exchange of sensitive health information, necessitating robust security measures to protect patient data [54]. The rapid implementation of telemedicine during the pandemic highlighted vulnerabilities in data security, as many healthcare providers were unprepared for the increased risk of data breaches [55]. Therefore, establishing clear legal frameworks and ensuring compliance with data protection regulations are essential for fostering trust in telemedicine services.
Technological barriers are another significant challenge in the implementation of telemedicine. Connectivity issues in remote areas can severely limit access to telehealth services. Many patients in rural or underserved regions lack reliable internet access, which can hinder their ability to participate in virtual consultations [56]. This digital divide exacerbates existing health disparities, as those who would benefit most from telemedicine may be the least able to access it. Additionally, device interoperability and integration challenges present obstacles to effective telemedicine. Many healthcare providers utilize different platforms and technologies, leading to fragmented care and inefficiencies [57,58]. The lack of standardized protocols for telemedicine can complicate the integration of various devices and systems, making it difficult for providers to share information seamlessly and coordinate care effectively.
Adoption barriers among patients and providers also play a crucial role in telemedicine’s challenges. Digital literacy is a significant concern, particularly among older adults and individuals from lower socioeconomic backgrounds. Many patients may struggle to navigate telemedicine platforms, leading to frustration and reluctance to use these services [59,60]. Training and educational resources are essential to enhance digital literacy and ensure that patients can effectively engage with telehealth technologies [61]. Furthermore, ethical concerns in virtual diagnosis can deter both patients and providers from fully embracing telemedicine. The inability to conduct physical examinations can lead to apprehensions about the quality of care delivered through virtual consultations [62,63]. Providers may feel less confident in diagnosing and treating patients remotely, impacting their willingness to adopt telemedicine practices [64]. Addressing these ethical concerns through clear guidelines and best practices is vital for fostering confidence in telemedicine.
Reimbursement Policies and Economic Considerations
The integration of telemedicine and RPM into healthcare systems has been accelerated by the COVID-19 pandemic, prompting significant changes in reimbursement policies and economic considerations. As healthcare providers increasingly adopt these technologies, understanding the financial implications and reimbursement frameworks becomes crucial for sustainable implementation. Reimbursement for telehealth services has historically been inconsistent and influenced by various factors, including state regulations, payer policies, and the services’ nature. For instance, differences in reimbursement rates for video versus telephone consultations have created disparities in access to care [65]. The pandemic prompted emergency legislation that temporarily relaxed restrictions on telehealth reimbursement, allowing for broader coverage by insurance companies [66]. This shift has been essential for maintaining continuity of care during heightened demand for remote services [67]. However, the longterm sustainability of these changes remains uncertain, as many providers express concerns about the permanence of these policies [68].
Economic considerations surrounding telemedicine extend beyond reimbursement rates. The cost-effectiveness of RPM technologies, particularly in managing chronic diseases, has been a focal point of research. Studies indicate that RPM can lead to reduced hospitalizations and lower overall healthcare costs by facilitating timely interventions and improving patient outcomes [69]. For example, a systematic review highlighted the potential of RPM to enhance disease management in cardiovascular patients, suggesting that it could be a cost-effective alternative to traditional in-person visits [70]. However, the economic benefits of RPM are often contingent on adequate reimbursement structures that incentivize its use [71].
Moreover, the implementation of telehealth services has revealed disparities in access and utilization, particularly among vulnerable populations. Higher telehealth utilization rates among Medicaid patients have been attributed to state-level policy changes that expanded coverage [72]. This indicates that equitable reimbursement policies are essential to ensure all patient demographics can benefit from telemedicine services. Additionally, the need for ongoing education and support for both patients and providers is critical to maximize the effectiveness of RPM systems [44]. The need for technological infrastructure and training also shapes the economic landscape of telemedicine. Investments in telehealth platforms and training for healthcare professionals are necessary to ensure effective service delivery [73]. However, these initial costs can be a barrier for some healthcare systems, particularly smaller practices that may lack the resources to implement comprehensive telehealth solutions [74]. Reimbursement policies must account for these initial investments to encourage widespread adoption.
Case Studies: Successful Implementations and Lessons Learned
Telemedicine and RPM have emerged as transformative forces in healthcare delivery, particularly in managing chronic diseases, enhancing access to care in rural areas, and leveraging AI for predictive healthcare. This chapter explores three case studies that exemplify these advancements: Remote Monitoring for Chronic Disease Management, Telehealth in Rural Healthcare Systems, and AI-Powered Telemedicine in Predictive Healthcare.
Case Study 1: Remote Monitoring for Chronic Disease Management
Remote monitoring has proven to be a pivotal strategy in managing chronic diseases such as diabetes, hypertension, and chronic obstructive pulmonary disease (COPD). Studies indicate that telemedicine interventions significantly improve diseasespecific outcomes, including better glycemic control in diabetic patients and enhanced blood pressure management in hypertensive individuals [75]. The integration of RPM technologies allows healthcare providers to collect real-time health data from patients, facilitating timely interventions and personalized care plans [70]. For instance, the inSight program demonstrated that pharmacists could effectively manage chronic diseases through telephone and remote monitoring, improving patient outcomes. Furthermore, a systematic review highlighted that RPM not only enhances patient engagement but also reduces hospital admissions and emergency visits, showcasing its efficacy in chronic disease management [76].
Case Study 2: Telehealth in Rural Healthcare Systems
Telehealth has been particularly beneficial in rural healthcare systems, where access to traditional healthcare services is often limited. Research indicates that telehealth interventions have led to decreased travel costs and times for patients while maintaining similar levels of patient satisfaction compared to in-person visits [77]. For example, an extensive integrated healthcare system in New York utilized telemedicine to provide express care for minor complaints, effectively addressing the healthcare needs of rural populations [78]. Additionally, the COVID-19 pandemic accelerated the adoption of telehealth services, which played a critical role in maintaining healthcare access for underserved communities [79]. The ability to conduct remote consultations has proven essential in managing chronic conditions, particularly during public health emergencies, thereby reducing the burden on healthcare facilities [80].
Case Study 3: AI-Powered Telemedicine in Predictive Healthcare
The integration of AI into telemedicine represents a significant advancement in predictive healthcare. AI-enhanced remote monitoring systems facilitate continuous health monitoring and data analysis, allowing for proactive management of chronic diseases [81]. These systems can identify patterns and predict potential health crises, enabling timely interventions to prevent hospitalizations [82]. For instance, wearable devices with AI capabilities can track vital signs and alert healthcare providers to anomalies, thus improving patient outcomes. Moreover, the Internet of Medical Things (IoMT) has emerged as a critical component in this domain, enabling seamless data transmission and real-time monitoring of patients’ health conditions. Combining AI and telemedicine enhances healthcare delivery efficiency and empowers patients to manage their health actively.
Conclusion
Telemedicine and RPM have significantly transformed modern healthcare by improving accessibility, patient outcomes, and costeffectiveness This chapter has explored these evolving healthcare modalities’ technological foundations, clinical applications, benefits, challenges, and economic considerations. The integration of telemedicine with communication platforms, wearable devices, AI, and cloud computing has enabled real-time patient monitoring and data-driven decision-making. These advancements have particularly benefited chronic disease management, postoperative care, rural healthcare, and mental health services. One of the most profound impacts of telemedicine and RPM is their role in improving patient engagement and self-management. By facilitating continuous health monitoring, these technologies empower patients to take an active role in their healthcare while reducing the burden on healthcare systems. Furthermore, the COVID-19 pandemic accelerated their adoption, demonstrating their potential to maintain continuity of care during crises. Despite these advantages, challenges such as regulatory barriers, data privacy concerns, digital literacy issues, and disparities in access to telehealth remain significant obstacles to widespread implementation. Addressing these challenges requires policy reforms, enhanced security measures, and investment in digital infrastructure, particularly in underserved areas.
The economic implications of telemedicine and RPM also underscore their potential to optimize healthcare costs. Studies have shown that RPM reduces hospitalizations and emergency visits, leading to substantial cost savings for patients and healthcare providers. However, sustaining these technologies requires supportive reimbursement policies and financial incentives for healthcare systems. The future of telemedicine lies in integrating AI, the Internet of Medical Things (IoMT), and predictive analytics to enhance personalized medicine and early disease detection. In conclusion, telemedicine and RPM represent a paradigm shift in healthcare delivery. While challenges persist, these technologies’ continued advancement and strategic implementation can bridge healthcare disparities, improve patient outcomes, and shape the future of global healthcare systems.
References
- Vudathaneni VKP, Lanke RB, Mudaliyar MC, Movva KV, Kalluri LM, et al. (2024) The impact of telemedicine and remote patient monitoring on healthcare delivery: a comprehensive evaluation. Cureus 16(3): e55534-e55539.
- Toritsemogba Tosanbami Omaghomi, Oluwafunmi Adijat Elufioye, Opeoluwa Akomolafe, Evangel Chinyere Anyanwu, Ifeoma Pamela Odilibe (2024) A Comprehensive Review of Telemedicine Technologies: Past, Present, And Future Prospects. Int Med Sci Res J 4(2): 183–193.
- Pinnock H, Hanley J, McCloughan L, Todd A, Krishan A, et al. (2013) The effectiveness of telemonitoring integrated into existing clinical services on hospital admission for chronic obstructive pulmonary disease exacerbation: researcher blind, multicentre, randomised controlled trial. BMJ 347(1): f6070–f6070.
- Akar JG, Bao H, Jones P, Wang Y, Chaudhry SI, et al. (2013) Use of Remote Monitoring of Newly Implanted Cardioverter-Defibrillators: Insights from the Patient Related Determinants of ICD Remote Monitoring (PREDICT RM) Study. Circulation 128(22): 2372–2383.
- Gershon Davydov (2023) Revolutionizing Healthcare Delivery: The Transformative Impact of Telemedicine in the Post-Pandemic Era. J Int Med Grad 2(1): 01-03.
- Ananthakrishnan M, Chaitra CM (2023) Qualitative Study of Community Health Officers’ Experiences With telemedicine in A Rural Block of Madhya Pradesh. PARIPEX INDIAN J Res 12(8): 15–7.
- Singhal A, Riley JP, Cowie MR (2023) Benefits and challenges of telemedicine for heart failure consultations: a qualitative study. BMC Health Serv Res 23(1): 847-850.
- Bange EM, Li Y, Kumar P, Doucette A, Gabriel P, et al. (2024) The association between telemedicine, advance care planning, and unplanned hospitalizations among high‐risk patients with cancer. Cancer 130(4): 636–644.
- Mamta Kale (2023) Telemedicine Revolution: Bridging Gaps in Access to Healthcare. Int J Recent Innov Trends Comput Commun 11(7): 394–399.
- McGrowder DA, Miller FG, Vaz K, Anderson Cross M, Anderson Jackson L, et al. (2021) The Utilization and Benefits of Telehealth Services by Health Care Professionals Managing Breast Cancer Patients during the COVID-19 Pandemic. Healthcare 9(10): 1401-1405.
- Kissi J, Dai B, Dogbe CS, Banahene J, Ernest O (2020) Predictive factors of physicians’ satisfaction with telemedicine services acceptance. Health Informatics J 26(3): 1866–1880.
- Dahan F, Alroobaea R, Alghamdi WaelY, Mustafa Khaja Mohammed, Hajjej F, et al. (2023) A smart IoMT based architecture for E-healthcare patient monitoring system using artificial intelligence algorithms. Front Physiol. 14(2): 1125952-1125958.
- Iranpak S, Shahbahrami A, Shakeri H (2021) Remote patient monitoring and classifying using the internet of things platform combined with cloud computing. J Big Data 8(1): 120-125.
- Obira JO, Sinde R (2021) Development of a Sensor-Based Heartbeat and Body Temperature Monitoring System for Remote Chronic Patients. Eng Technol Appl Sci Res 11(4): 7375–7380.
- Qureshi MA, Qureshi KN, Jeon G, Piccialli F (2022) Deep learning-based ambient assisted living for self-management of cardiovascular conditions. Neural Comput Appl 34(3): 10449–10467.
- Hwang DK, Hsu CC, Chang KJ, Chao D, Sun CH, et al. (2019) Artificial intelligence-based decision-making for age-related macular degeneration. Theranostics 9(1): 232–245.
- Sugandi MS, Mulyana D, Elita RFM, Rusmana A (2023) Lessons Learned from the Pandemic in Indonesia: Enhancing Doctor-Patient Medical Communication to Improve Diagnostic Certainty in Telemedicine. J Law Sustain Dev. 11(11): e2076-e2078.
- Antony LPL (2025) Revolutionizing Neurostimulator Care: Enhancing Remote Health Monitoring through SDN-Cloud Networks. Telecommunication Systems 88(12): 1-10.
- Raghavan A, Demircioglu MA, Taeihagh A (2021) Public Health Innovation through Cloud Adoption: A Comparative Analysis of Drivers and Barriers in Japan, South Korea, and Singapore. Int J Environ Res Public Health 18(1): 334-338.
- Shankar GS, Onyema EM, Kavin BP, Gude V, Prasad BS (2024) Breast Cancer Diagnosis Using Virtualization and Extreme Learning Algorithm Based on Deep Feed Forward Networks. Biomed Eng Comput Biol 15(4): 11795972241278907-11795972241278909.
- Kotzias K, Bukhsh FA, Arachchige JJ, Daneva M, Abhishta A (2023) Industry 4.0 and healthcare: Context, applications, benefits and challenges. IET Softw 17(3): 195–248.
- Zhao H, Zhang Z, Tang J (2024) Enhancing rural healthcare through internet-based remote collaborative outpatient services: A comprehensive evaluation in Changzhi, Shanxi Province. Medicine (Baltimore) 103(36): e39614-e39619.
- Yang DM, Chang TJ, Hung KF, Wang ML, Cheng YF, et al. (2023) Smart healthcare: A prospective future medical approach for COVID-19. J Chin Med Assoc 86(2): 138–146.
- Zhang J, Yang H (2023) A Privacy-Preserving Remote Heart Rate Abnormality Monitoring System. IEEE Access 11(1): 97089–97098.
- Wang S, Gao T, Zhang Y (2018) Searchable and revocable multi-data owner attribute-based encryption scheme with hidden policy in cloud storage. Lin F, editor. PLOS ONE 13(11): e0206126-e0206129.
- Gallardo MO, Dela Torre J, Ebardo R (2024) The Role of Initial Trust in the Behavioral Intention to Use Telemedicine Among Filipino Older Adults. Gerontol Geriatr Med 10(1): 1-10.
- Syed Irfanul Hoque, Asif Mahbub Karim, Md Rabiul Hossen, Dina Arjumand (2021) Evaluation of Patients’ Satisfaction in Telemedicine Service Quality: A Case Study on Maizbhanderi Foundation, Fatikchari, Bangladesh. Am Econ Soc Rev 8(1): 1–10.
- Vaidya V, Patil V, Oswal J, Narula A, Khare Y, et al. (2024) Healthcare in the Modern Era: Launching a Telemedicine-Based OPD Consultation in Rural Pune (Process, Results, and Challenges). Cureus 16(5): e60310-e60315.
- Shareef SM, Goud BP, Domalapally B, Ashraf TN, Prakash GB, et al. (2024) Assessing Telemedicine Competency Among Doctors in a Tertiary Care Hospital: A Questionnaire-Based Cross-Sectional Study. Cureus 16(4): e57712-e57718.
- Bhaskar S, Bradley S, Chattu VK, Adisesh A, Nurtazina A, et al. (2020) Telemedicine as the New Outpatient Clinic Gone Digital: Position Paper From the Pandemic Health System REsilience PROGRAM (REPROGRAM) International Consortium (Part 2). Front Public Health 8(2): 410-415.
- Libreros Peña L, Quintero JA, Gelves A, Alarcón J, Morales S, et al. (2023) Telemedicine consultation for emergency patients’ attention: a clinical experience from a high complex university hospital from Latin America. BMC Health Serv Res 23(1): 559-566.
- Gupta PP, Uranw S, Gupta S, Das RK, Bhattarai A, et al. (2021) Study of the impact of a telemedicine service in improving pre-hospital care and referrals to a tertiary care university hospital in Nepal. J Fam Med Prim Care 10(12): 4531–4535.
- Prodhan UK, Rahman MZ, Jahan I (2018) Design and implementation of an advanced telemedicine model for the rural people of Bangladesh. Technol Health Care 26(1): 175–180.
- Gao J, Fan C, Chen B, Fan Z, Li L, et al. (2022) Telemedicine Is Becoming an Increasingly Popular Way to Resolve the Unequal Distribution of Healthcare Resources: Evidence From China. Front Public Health 10(8): 916303-916309.
- Omaghomi TT, Arowoogun JO, Akomolafe O, Odilibe IP, Elufioye OA (2024) Telemedicine in rural Africa: A review of accessibility and impact. World J Adv Res Rev 21(2): 421–431.
- Park JH, Lee MJ, Tsai MH, Shih HJ, Chang J (2023) Rural, Regional, Racial Disparities in Telemedicine Use During the COVID-19 Pandemic Among US Adults: 2021 National Health Interview Survey (NHIS). Patient Prefer Adherence 17(65): 3477–3487.
- Said S, Khan A, Talreja C, Nazir N, Ibrahim HF, et al. (2024) Bridging Healthcare Horizons: Illuminating Pakistani Medical Students’ Perspectives on Telemedicine. Int J Health Med Nurs Pract 6(3): 52–61.
- Yankappa N, Kumar A, Prasad A, Tiwari L, Kumar P (2024) Clinicodemographic Profile and Clinical Outcome of Children Presenting to Telemedicine Center at Institute of National Importance of India: A Prospective Observational Study. Int J Telemed Appl 2024(8): 1–9.
- Samira Abdul, Ehizogie Paul Adeghe, Bisola Oluwafadekemi Adegoke, Adebukola Adejumoke Adegoke, Emem Henry Udedeh (2024) A review of the challenges and opportunities in implementing health informatics in rural healthcare settings. Int Med Sci Res J 4(5): 606–631.
- Hubach RD, O Neil AM, Hamrick J, Ernst C, Stowe M, et al. (2021) Assessing the amenability of rural MSM to using telemedicine for medical and mental healthcare. Ann LGBTQ Public Popul Health 2(2): 125–34.
- Walker RC, Tong A, Howard K, Palmer SC (2020) Clinicians’ experiences with remote patient monitoring in peritoneal dialysis: A semi-structured interview study. Perit Dial Int J Int Soc Perit Dial 40(2): 202–208.
- Goto T, Mori K, Nakayama T, Yamamoto J, Shintani Y, et al. (2020) Transmission Rate of Remote Monitoring and Mortality in Patients With Pacemaker. Circ Rep 2(9): 471–478.
- Hwang Y, Bae H (2023) The first pilot study on remote monitoring of implantable cardiac electronic devices in South Korea: rationale and study protocol of a REMOTE-CARE. pp. 1-12.
- El Rashidy N, El Sappagh S, Islam S, M. El Bakry H, Abdelrazek S (2021) Mobile Health in Remote Patient Monitoring for Chronic Diseases: Principles, Trends, and Challenges. Diagnostics 11(4): 607-639.
- Bart Seppen, Jimmy Wiegel, Marieke M Ter Wee, Dirkjan van Schaardenburg, Leo D Roorda (2022) Smartphone-Assisted Patient-Initiated Care Versus Usual Care in Patients With Rheumatoid Arthritis and Low Disease Activity: A Randomized Controlled Trial.Arthritis Rheumatol 74(11): 1737-1745.
- De Larochellière H, Champagne J, Sarrazin J, Steinberg C, Philippon F, et al. (2020) Findings of remote monitoring of implantable cardioverter defibrillators during the COVID‐19 pandemic. Pacing Clin Electrophysiol 43(11): 1366–1372.
- Idris U, Abdulkarim L, Arkwright B (2022) Systematic Overview of Remote Patient Monitoring in Nigeria (West Africa). Telehealth Med Today 7(3): 359-365.
- Lindsay R, Cunnington P, Dixon-Woods M (2024) Why is implementing remote monitoring in virtual wards (Hospital at Home) for people living with frailty so hard? Qualitative interview study. Age Ageing 54(1): afaf003-afaf009.
- Lehmann HI, Sharma K, Bhatia R, Mills T, Lang J, et al. (2023) Real‐World Disparities in Remote Follow‐Up of Cardiac Implantable Electronic Devices and Impact of the COVID‐19 Pandemic: A Single‐Center Experience. J Am Heart Assoc 12(3): e027500-e027502.
- Singh R, Sharma HK, Choudhury T, Mor A, Mohanty S, et al. (2023) Blockchain for IoT-enabled Healthcare. EAI Endorsed Trans Pervasive Health Technol 9(8): 1-7.
- Kaliyadan F, Al Ameer MA, Al Ameer A, Al Alwan Q (2020) Telemedicine practice in Saudi Arabia during the COVID-19 pandemic. Cureus 12(12): e12004-e12009.
- Iyer S, Shafi K, Lovecchio F, Turner R, Albert TJ, et al. (2022) The Spine Physical Examination Using Telemedicine: Strategies and Best Practices. Glob Spine J 12(1): 8–14.
- Nanda M, Sharma R (2021) A Review of Patient Satisfaction and Experience with Telemedicine: A Virtual Solution During and Beyond COVID-19 Pandemic. Telemed E Health 27(12): 1325–1331.
- Cui F, Ma Q, He X, Zhai Y, Zhao J, et al. (2020) Implementation and application of telemedicine in China: cross-sectional study. JMIR MHealth UHealth 8(10): e18426-e18429.
- Mohammadzadeh N, Rezayi S, Saeedi S (2022) Telemedicine for patient management in remote areas and underserved populations. Disaster Med Public Health Prep 17(8): e167-e171.
- Khoong EC, Butler BA, Mesina O, Su G, DeFries TB, et al. (2021) Patient interest in and barriers to telemedicine video visits in a multilingual urban safety-net system. J Am Med Inform Assoc 28(2): 349–353.
- Cheng C, Humphreys H, Kane B (2022) Transition to telehealth: Engaging medical students in telemedicine healthcare delivery. Ir J Med Sci 191(5): 2405–2422.
- Ftouni R, AlJardali B, Hamdanieh M, Ftouni L, Salem N (2022) Challenges of Telemedicine during the COVID-19 pandemic: a systematic review. BMC Med Inform Decis Mak 22(1): 207-209.
- D Domingo J, Karla M Durian G, Andre H Lucido M, Kyla Maru A Magcamit Ma, Louise Z Roque K, et al. (2021) Factors Affecting the Applicability of Telemedicine in Selected Areas of Luzon based on the Perceptions of Medical Professionals. Int J Res Publ 82(1): 110-124.
- Garcia Huidobro D, Rivera S, Valderrama Chang S, Bravo P, Capurro D (2020) System-wide accelerated implementation of telemedicine in response to COVID-19: mixed methods evaluation. J Med Internet Res 22(10): e22146-e22152.
- Elam AR, Sidhom D, Ugoh P, Andrews CA, De Lott LB, et al. (2022) Disparities in Eye Care Utilization During the COVID-19 Pandemic. Am J Ophthalmol 233(9): 163–170.
- Fatabhoy MG, Zhu G, Lajaunie A, Schneiderhan JR, Pierce J (2023) Intimate Partner Violence and Telemedicine Usage and Satisfaction Early in the COVID-19 Pandemic. J Am Board Fam Med 36(5): 755–765.
- Vongsachang H, Lagstein O, Boland MV, Repka MX, Kraus CL, et al. (2021) Telemedicine utilization by pediatric ophthalmologists during the COVID-19 pandemic. J Am Assoc Pediatr Ophthalmol Strabismus. 25(5): 293-295.e1.
- Sawicki GS, Van Citters AD, Dieni O, Sabadosa KA, Willis A, et al. (2021) Financial impacts of the COVID-19 pandemic on cystic fibrosis care: lessons for the future. J Cyst Fibros 20(Suppl 3): 16–20.
- Coto J, Restrepo A, Cejas I, Prentiss S (2020) The impact of COVID-19 on allied health professions. PLOS ONE 15(10): e0241328-e0241335.
- Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, et al. (2020) Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc 27(6): 957–962.
- DeHart D, Iachini A, King LB, LeCleir E, Reitmeier M, et al. (2023) Benefits and Challenges of Telehealth Use during COVID-19: Perspectives of Patients and Providers in the Rural South. Adv Soc Work 22(3): 953–975.
- Isaranuwatchai W, Redwood O, Schauer A, Van Meer T, Vallée J, et al. (2018) A Remote Patient Monitoring Intervention for Patients With Chronic Obstructive Pulmonary Disease and Chronic Heart Failure: Pre-Post Economic Analysis of the Smart Program. JMIR Cardio 2(2): e10319-e10322.
- Zhang Y, Pena MT, Fletcher LM, Swint JM, Reneker JC (2022) Cost of remote patient monitoring for cardiovascular disease: a systematic review protocol. JBI Evid Synth 20(6): 1585–1592.
- Ward K, Vagholkar S, Sakur F, Khatri NN, Lau AYS (2022) Visit Types in Primary Care With Telehealth Use During the COVID-19 Pandemic: Systematic Review. JMIR Med Inform 10(11): e40469-e40472.
- Acharya M, Ali MM, Hayes CJ, Bogulski CA, Magann EF, et al. (2023) Trends in Telehealth Visits During Pregnancy, 2018 to 2021. JAMA Netw Open 6(4): e236630-e236639.
- Shah SS, Gvozdanovic A, Knight M, Gagnon J (2021) Mobile App–Based Remote Patient Monitoring in Acute Medical Conditions: Prospective Feasibility Study Exploring Digital Health Solutions on Clinical Workload During the COVID Crisis. JMIR Form Res 5(1): e23190-e23196.
- Gajarawala SN, Pelkowski JN (2021) Telehealth Benefits and Barriers. J Nurse Pract 17(2): 218–221.
- Alanazi ESS, Alenezi MSK, Alenezi MFM, Albarrak SIR, Aghithi ASM, et al. (2024) Exploring Health Informatics for Chronic Disease Management: A Systematic Review of Tools and Outcomes. J Ecohumanism 3(8): 960–967.
- Oesterle TS, Karpyak VM, Coombes BJ, Athreya AP, Breitinger SA, et al. (2022) Systematic review: Wearable remote monitoring to detect nonalcohol/nonnicotine‐related substance use disorder symptoms. Am J Addict 31(6): 535–545.
- Butzner M, Cuffee Y (2021) Telehealth Interventions and Outcomes Across Rural Communities in the United States: Narrative Review. J Med Internet Res 23(8): e29575-e29579.
- Kolluri S, Stead TS, Mangal RK, Coffee RL, Littell J, et al. (2022) Telehealth in Response to the Rural Health Disparity. Health Psychol Res 10(3): 37445-37449.
- Demeke HB, Merali S, Marks S, Pao LZ, Romero L, et al. (2021) Trends in Use of Telehealth Among Health Centers During the COVID-19 Pandemic - United States, June 26–November 6, 2020. MMWR Morb Mortal Wkly Rep 70(7): 240–244.
- Monaghesh E, Hajizadeh A (2020) The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 20(1): 1193-1199.
- Geneva Tamunobarafiri Igwama, Ejike Innocent Nwankwo, Ebube Victor Emeihe, Mojeed Dayo Ajegbile (2024) AI-Enhanced remote monitoring for chronic disease management in rural areas. Int J Appl Res Soc Sci 6(8): 1824–1847.
- Eman Shukhair Suliman Alanazi, Mona Sanad Khudair Alenezi, Mai Fahad Muqbel Alenezi, Suad Ibrahim Rubaiean Albarrak, Afrah Saud Musabeh Aghithi (2024) Exploring Health Informatics for Chronic Disease Management: A Systematic Review of Tools and Outcomes.Journal of Ecohumanism 3(8): 960-967.
- Shafiq M, Choi JG, Cheikhrouhou O, Hamam H (2023) Advances in IoMT for Healthcare Systems. Sensors 24(1): 10-14.
-
Awez A Sikkalgar, Kalpesh R Yeole, Naina Chaurasiya, Devendra K Jadhav, Zubair Saghir Ahmed Shaikh and Sagar A More*. Telemedicine and Remote Patient Monitoring: Transforming Healthcare Delivery. Sci J Biol & Life Sci. 4(2): 2025. SJBLS. MS.ID.000584.
-
Artificial intelligence; modern healthcare; telemedicine; remote patient monitoring
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






