 Research Article
Research Article
Patterns of Serum Immuno-Biomarkers in Allergic Bronchial Asthma Patients
Opeoluwa Yusuf1, Daniel Ugbomoiko2, Temitope Ogunleye3, Olumide Festus Adegeye4 and Elizabeth Abodunrin5*
1Department Of Medical Laboratory Science, College of Health Science, Igbinedion University Okada, Nigeria
2Department Of Medical Laboratory Science, College of Health Science, Igbinedion University Okada, Nigeria
3Advocate Health Care, Trinity Hospital, Illinois, USA
4East Kent Hospital University NHS Foundation Trust, UK
5Biological Sciences, Lead City University, Nigeria
Elizabeth Abodunrin, Biological Sciences, Lead City University, 0000- 0002-1467-4132, Nigeria
Received Date: June 27, 2025; Published Date: July 08, 2025
Abstract
Objectives: Bronchial asthma is a diverse chronic inflammatory and obstructive pulmonary condition characterized by augmented mucus,
airway hyperactivity, secretion, tissue remodeling, declining airway function, as a result, leading to long-term, functional and structural lung tissue alterations. This study examined patterns of some immune-biomarkers and their impact on asthma severity and management in Nigerian adults.
Methods: Ninety adult asthmatic patients and ninety healthy controls were enrolled in this study. The socio-demographic and anthropometric
data were collected using a modified WHO stepwise questionnaire and instruments at the XXXXXX. Five milliliters of blood were collected and
then analyzed for hs-CRP, IgE, and IL-4 using an ELISA assay. Descriptive and analytical statistical methods were employed to investigate the data
systematically. A p-value of 0.05 was considered statistically significant.
Results: The Serum IgE, hs-CRP, and IL-4 levels were found to be significantly higher in the asthmatic group compared to the control group,
respectively. There was a positive correlation, whereas IgE and hs-CRP showed a negative correlation. Conclusion: The immune response ratios of
the parameters studied could serve as potential biomarkers for diagnosing, diagnosing, and managing allergic asthma in adults.
Keywords: Allergy; biomarkers; bronchial asthma; immunity; inflammation
Introduction
Asthma is a chronic inflammatory respiratory disease characterized by airways inflammation and hyper-responsiveness in the lungs, leading to structural changes that narrow the passage [1]. This constriction often cause difficulties in breathing and uneasiness [1]. Symptoms include intermittent dyspnea, wheezing and cough. However, because these symptoms are nonspecific in nature, differentiating asthma from other respiratory conditions can often be challenging [2]. The expression of asthma results from a complex interaction between genetic predisposition and environmental influences, including allergens, diet and exposure to passive smoke [3]. These factors collectively shape disease susceptibility, severity, and overall respiratory health. Asthma manifests as two major phenotypes, atopic (extrinsic) and nonatopic (intrinsic). Atopic asthma is more common during childhood and young adulthood, whereas the non-atopic form becomes predominant in older age groups [4,5]. Over the years, there has been advancements in asthma treatment that has improved patient outcomes. However, there are still differences in how care is provided between high- and low-income countries with variations in access to medication, diagnostic tools, and healthcare infrastructure [2].
The World Health Organization (WHO) reported that asthma affected approximately 262 million people in the year 2019, and accounted for about 455,000 deaths globally [6]. There are studies that examined the prevalence of asthma across about 17 countries showing different rates, which range from 3.4% to 6% for adults and children in India, Nigeria, Taiwan, Kosovo, and Russia, and higher rates of 17% to 33% for Honduras, Brazil, Costa Rica, and New Zealand [7]. Asthma poses a major public health challenge in Nigeria, with an approximate estimate of 13 million Nigerians been affected by asthma, which makes it one of the highest burdens in Africa [8]. Asthma impacts all age groups, sex and race. Research have shown that girls are less affected than boys in childhood and the prevalence tends to equalize and subsequently, more women may become affected than men possibly due to hormonal influences and differences in immune responses [9]. No single gene or environmental factor has been identified as the sole cause of atopic asthma, however, a genetic predisposition to trigger a localized mucosal immunoglobulin (Ig) response plays a significant role in its development [10]. Type II T lymphocyte helper (Th2)- associated inflammation and immunoglobulin E (IgE) production are key features of non-atopic (intrinsic) asthma. Cytokines play an important role in regulating IgE synthesis, while eosinophil count and activity significantly contribute to disease progression.
The Th2-related cytokines are IL2, IL4, IL5, IL10 and IL3 are involved in the pathogenesis and expression of Asthma [11]. C-reactive protein (CRP) is a key biomarker of inflammation. Monitoring CRP levels serves as a valuable diagnostic tool for early inflammation detection, treatment evaluation and acutephase disease assessment [12]. CRP levels increase in allergic and autoimmune disorders and act as a sensitive marker for inflammation, tissue damage and allergens. Also CRP plays a role in host defense against infection by activating the complement pathway. Studies show a positive correlation between elevated high-sensivity CRP (hs-CRP) levels, asthma, respiratory impairment and bronchial hyper-reactivity [13]. Recent studies have highlighted serum levels of hs-CRP as a valuable tool for detecting systemic inflammation in asthma, this suggests that hs-CRP serves as an effective alternative marker for predicting the severity of inflammation of bronchus in asthma [14]. However, future research is needed to compare the efficiency and accuracy of hs-CRP levels with other methods for assessing asthma exacerbation. In most asthmatic patients, inflammation remain persistent even in the absence of symptoms [15]. This means that managing asthma by only symptom control may lead to persistent, unopposed inflammation in the lungs, potentially leading to irreversible structural changes in the lungs and declining lung function [16]. The study aimed to determine the pattern of biomarkers in bronchial asthmatic patients in Ibadan, Nigeria.
Materials and Methods
Study place and design
Patient recruitment was conducted at the Respiratory Unit of the Clinical Out-patient Department, XXXXXX. This is a case-control observational study. Total number of adult participants were one hundred and eighty, comprising of ninety subjects whose age and sex were marched with ninety healthy control subjects.
Ethics approval
Study was done with prior approval of the XXXXXX. Hospital Joint Research Ethics Committee, Nigeria on the 5th Aug, 2024 (NHREC/05/01/2008a) after taking informed consent from all the participants.
Patients and data collection
Each participant was issued an informed consent before data collection. A questionnaire was issued to gather demographic characteristics, nutritional history, family background, and other relevant details. The collected data was systematically recorded for analysis.
Inclusion criteria
a. Participants between the ages of eighteen to sixty years as
at the time of the study.
b. Participants must have a clinically confirmed diagnosis of
allergic bronchial asthma.
Exclusion criteria
a. Participants who do not sign the written informed
consent.
b. Individuals that are HIV and or Hepatitis positive.
c. Individuals who are hypertensive or diabetic patients.
Laboratory Investigation
Five milliliters of venous blood sample was collected aseptically by venepuncture from the participants into plain bottle, and it was allowed to clot then centrifuged at 4000rpm for 10 minutes. The serum was separated into plain bottles and then analyzed for hs- CRP, IgE and IL-4.
Enzyme-linked Immunosorbent Assay (ELISA)
Expression levels of four selected enzymes, IL-4, hs-CRP and IgE were verified through ELISA. The micro-titer that was plate provided in the kit was pre-coated with each antibody respectively. Standard samples and Horse Radish Peroxidase (HRP) conjugated antibody were added to the wells. The uncombined enzyme was removed by incubating and washing each plate, after which Chromogen A and B Solution were added. The color changes of each result was measured using the spectrophotometry at 450 nm wavelength. The IgE, hs-CRP and IL-4 concentrations in the samples were determined by comparing the Optical Density (O.D) of the samples to the standard curve.
Statistical Analysis
The results from this study were presented as Mean ± standard deviation (SD). All data was analyzed statistically using SPSS statistical software (IBM SPSS Statistics 20; Chicago, IL, USA). The results were analyzed using independent‘t’ test and pearson correlation to estimate correlations. The statistically significant difference minimal limit for values was at p < 0.05.
Results
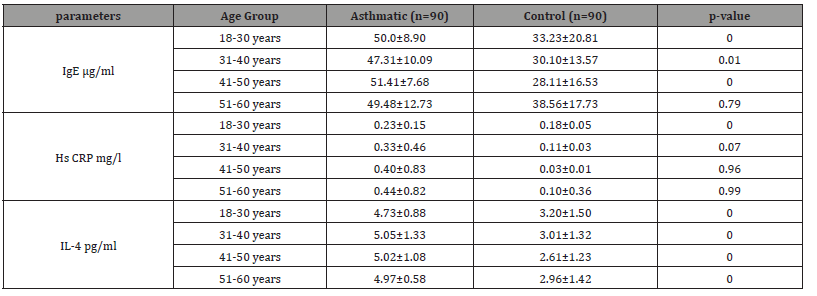
One hundred and eighty (180) asthmatic patients and healthy controls were recruited for this study. The test group were 50(55.6%) male and 40(44.4%) female, while the control group included 35(38.9%) male and 55(61.1%) female. All participants were between 18 and 60 years of age. Table 1 presents the descriptive statistical analysis of the demographic data for each group within the study population. Medical history and information of participants collected showed that, a total of 52 participants (48 asthmatic and 4 control), has family history of asthma, while 48 none. 53 of the participants were on medication while 35 were not. 8 out of 86 were said to be having respiratory tract infection. There were 4 smokers and 7 individuals who consume alcohol regularly among the asthmatic participants. 27 out of 87 were said to have been exposed to dust. Elevated BMI and former smoking status were more prevalent in asthmatic patients. Serum levels of IgE, hs- CRP, and IL-4 effectively distinguished asthmatic individuals from healthy controls. IL-4 showed consistent significance across all age groups, suggesting its central role in asthma-related inflammation (Table 2).
Table 1:Demographic information of the study population.
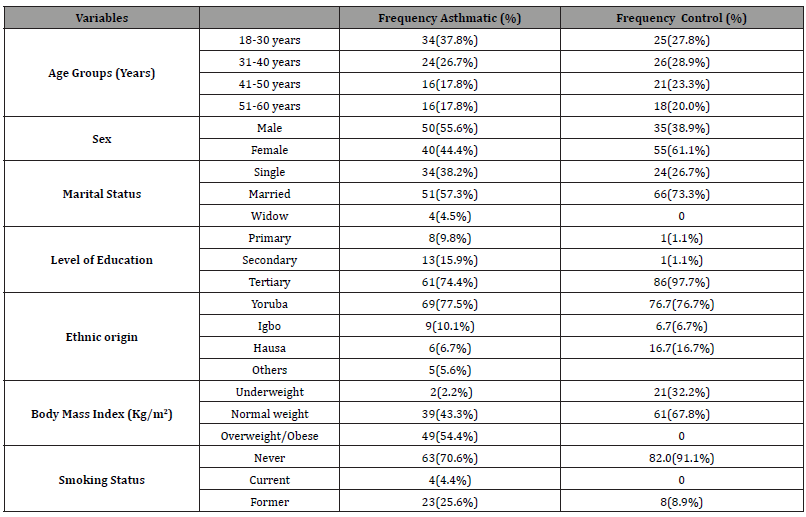
Table 2:Showing the comparison of some selected parameters according to age groups of participants and control.
Biochemical parameters
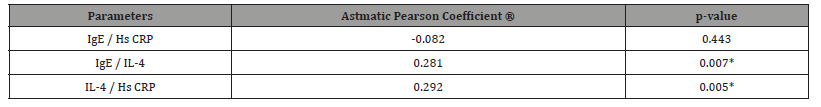
Some selected parameters (IL-4, hs-CRP and IgE) between asthmatic and control groups were investigated. Table 3 presents the descriptive statistical analysis of each parameter within the study population. Table 4 shows the serum levels value of IgE, hs-CRP, and IL-4. The serum levels swere significantly elevated in asthmatic patients compared to healthy controls.
Table 3:Showing the comparisons of biochemical parameters of participants.
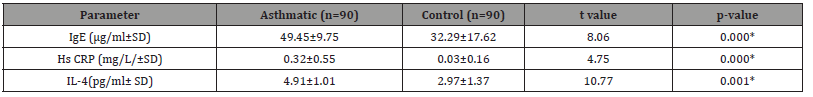
Table 4:Showing Pearson’s correlation of biochemical parameters in asthmatic patients.
Discussion
This study established that the body mass index (BMI), between asthmatic patients and healthy controls is a significantly increased. Numerous studies have identified a positive correlation between increased in body mass index (BMI) and the prevalence of asthma in adults. Research have shown that as obesity rates increases, the incidence of asthma simultaneously increase [17]. A Change in the respiratory mechanics due to obesity leads to a decreased functional residual capacity, and reduced tidal volume that contributes to impaired lung function. Also, sedentary lifestyle and a limited physical activities, are commonly related to obesity, and can also worsen asthma symptoms [18]. Recent Studies has also shown that the inflammatory changes observed in people who are obese may influence the clinical presentation and severity of asthma These alterations can impact airway inflammation, elevate symptoms, and potentially alter treatment efficacy in obese asthma patients [16]. Some studies have shown that elevated serum levels of IL-4 in obese individuals may intensify inflammatory pathways linked to asthma. This heightened inflammatory response can further impact airway muscle contractility, potentially exacerbating bronchoconstriction and worsening respiratory symptoms [19].
The findings showed that serum IgE (μg/L) in asthmatic individual were significantly elevated in asthmatic individuals compared to the control. Rage also reported that asthma is characterized by an elevation of serum levels of IgE, which also leads allergic reaction initiated by immunologic mechanisms mediated by IgE antibodies [20]. Buhl supported the findings that IgE plays an important role in triggering and sustaining the inflammatory cascade that drives allergic response. IgE activation leads to mast cell degranulation, releasing histamine and other inflammatory mediators, which contribute to hypersensitivity reactions [21]. The inflammatory action of asthma causes an elevation in airway hyper-sensitivity to various stimuli that can result in elevated levels of C reactive protein (CRP). CRP is a key biomarker of systemic inflammation that plays a crucial role in the body’s response to infection, tissue injury, and chronic inflammatory conditions [22]. This study reported an increased level of serum hs-CRP between asthmatic and non-asthmatic individual. This is in line with Kony who reported a positive relationship between elevated CRP levels and asthma, respiratory impairment and bronchial hyperresponsiveness [23].
Other research has shown that elevated levels of hs-CRP is linked with respiratory symptoms in adults with asthma, and the serum level of hs-CRP during exacerbation is significantly increased than the serum level during remission [24]. This study showed a direct correlation between the hs-CRP serum levels and asthma severity, although, with no significant differences observed between male and female asthmatic participants. Additionally, serum IL-4 levels were significantly elevated in asthmatic individuals when compared with controls. Lemanske and Busse reported elevated levels of Th2 cells in the airways, leading to the release of interleukin (IL)-4, and other cytokines that promote eosinophilic inflammation and IgE production by mast cells in asthma, contributing to asthma pathophysiology [25]. Studies have shown that asthma patients have elevated IL-4 protein levels in serum, increased IL-4 mRNA and protein in bronchial biopsies, and increased numbers of (T-) cells expressing IL-4 mRNA in bronchoalveolar lavage fluid (BALF) and bronchial biopsies [26]. This study reported positive correlation between IgE and IL-4. Buhl showed that TH2 type T cells induction releases IL-4, the cytokines released in turn promotes the production of IgE by B cells, growth of mast cells (IL- 4) and activation of eosinophils [27]. Positive association was also observed between IL-4 and hs-CRP.
Conclusion
The integration of precision medicine into asthma management in clinical practice proves the importance of identifying specific biomarkers. Various biomarkers have been clinically utilized to predict responses to steroid therapy, and within clinical trial settings to determine patients that are likely to benefit from biologic therapies, however, the number of available biomarkers remains limited and their predictive accuracy continues to pose challenges. Currently, patients with severe allergic asthma identified by elevated serum IgE levels, anti-cytokine therapies hold significant potential for the future of allergy and asthma treatment. Despite initial setbacks, there are several emerging anti-IL-4 therapies that appear promising, their clinical efficacy is closely linked to advancements in defining an individual’s asthma endotype, enabling a more precise understanding of specific asthma pathogenesis and tailored treatment approaches. This study demonstrated increase in serum IgE, hs CRP and IL-4 which provides recent diagnosis as well as modern treatment of asthma. In conclusion assay of the studied biomarkers routinely can help to deliver personalized therapy for the management of asthma by utilizing monoclonal antibodies of the studied immunobiomakers that can target these makers or their receptors may be made available for personalized therapeutic use.
Acknowledgment
All Authors have read and approved the final manuscript.
References
- Alsharairi NA (2023) Antioxidant Intake and Biomarkers of Asthma in Relation to Smoking Status-A Review. Curr Issues Mol Biol 45(6): 5099–5117.
- Peden DB (2010) Genetic and Environmental Factors in Asthma. In: Harver A, Kotses H (eds) Asthma, Health and Society, Boston, MA, Springer pp. 43-57.
- Tesfaye ZT, Gebreselase NT, Horsa BA (2018) Appropriateness of chronic asthma management and medication adherence in patients visiting ambulatory clinic of Gondar University Hospital: a cross-sectional study. World Allergy Organ J 11(1): 18-28.
- Wenzel SE (2012) Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med 18(5): 716-725.
- Miranda C, Busacker A, Balzar S, Trudeau J, Wenzel SE (2004) Distinguishing severe asthma phenotypes: role of age at onset and eosinophilic inflammation. J Allergy Clin Immunol 113(1): 101–108.
- GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258): 1204-1222.
- Mortimer K, Lesosky M, García Marcos L, Asher MI, Pearce N, et al. (2022) The burden of asthma, hay fever and eczema in adults in 17 countries: GAN Phase I study. Eur Respir J 60(3): 2102865-2102869.
- Ozoh OB, Aderibigbe SA, Ayuk AC, Desalu OO, Oridota OE, et al. (2019) The prevalence of asthma and allergic rhinitis in Nigeria: A nationwide survey among children, adolescents and adults. PLoS ONE 14(9): e0222281-e0222288.
- Fajt ML, Wenzel SE (2009) Asthma phenotypes in adults and clinical implications. Expert Rev Respir Med 3(6): 607-625.
- Murdoch JR, Lloyd CM (2010) Chronic inflammation and asthma. Mutat Res 690(1-2): 24-39.
- Palacionyte J, Januskevicius A, Vasyle E, Rimkunas A, Bajoriuniene I, et al. (2024) Novel Serum Biomarkers for Patients with AllergicAsthma Phenotype. Biomedicines 12(1): 232-239.
- Narendra D, Blixt J, Hanania, NA (2019) Immunological biomarkers in severe asthma. Semin Immunol 46(6): 101332-101336.
- Piloni D, Tirelli C, Domenica RD, Conio V, Grosso A, et al. (2018) Asthma-like symptoms: is it always a pulmonary issue? Multidiscip Respir Med 13(3): 21-26.
- Leong Tung Ong (2021) High-Sensitivity Assays for C-Reactive Protein as a Systemic Inflammatory Marker in Assessing Asthma. EMJ Allergy and Immunology 6(1): 53-60.
- Rath N, Raje N, Rosenwasser L (2018) Immunoglobulin E as a Biomarker in Asthma. Immunol Allergy Clin N Am 38(4): 587– 597.
- Withers AL, Green R (2019) Transition for Adolescents and Young Adults With Asthma. Front Pediatr 7(4): 301-305.
- Akerman MJ, Calacanis CM, Madsen MK (2004) Relationship between asthma severity and obesity. J Asthma 41(5): 521-526.
- Baruwa Pranab, Sarmah Kripesh (2013) Obesity and asthma. Lung India 30(1): 38-46.
- Yim S, Fredberg J, Malhotra.H (2007) Continuous positive airway pressure for asthma: not a big stretch? Eur Respir J 29(2): 226–228.
- Oczypok EA, Milutinovic PS, Alcorn JF, Khare A, Crum LT, et al. (2015) Pulmonary receptor for advanced glycation end-products promotes asthma pathogenesis through IL-33 and accumulation of group 2 innate lymphoid cells. J Allergy Clin Immunol 136(3): 747-756.
- Buhl R (2005) Anti-IgE antibodies for the treatment of asthma. Curr Opin Pulm Med 11(1): 27-34.
- Fonseca FA, Izar MC (2016) High-Sensitivity C-Reactive Protein and Cardiovascular Disease Across Countries and Ethnicities. Clinics (Sao Paulo)71(4): 235-242.
- Leynaert B, Neukirch C, Kony S, Guénégou A, Bousquet J, et al. (2004) Association between asthma and rhinitis according to atopic sensitization in a population-based study. J Allergy Clin Immunol 113(1): 86-93.
- Sigari N, Ghasri H (2013) Correlation between hs-CRP and Asthma Control Indices. Tanaffos 12(3): 44-48.
- Busse WW, Lemanske RF Jr, Gern JE (2010) Role of viral respiratory infections in asthma and asthma exacerbations. Lancet 376(9743): 826-834.
- Batra PS, Kern RC, Tripathi A, Conley DB, Ditto AM, et al. (2003) Outcome analysis of endoscopic sinus surgery in patients with nasal polyps and asthma. Laryngoscope 113(10): 1703-1706.
- Bousquet J, Cabrera P, Berkman N, Buhl R, Holgate S, et al. (2005) The effect of treatment with omalizumab, an anti-IgE antibody, on asthma exacerbations and emergency medical visits in patients with severe persistent asthma. Allergy 60(3): 302-308.
-
Opeoluwa Yusuf, Daniel Ugbomoiko, Temitope Ogunleye, Olumide Festus Adegeye and Elizabeth Abodunrin*. Patterns of Serum Immuno-Biomarkers in Allergic Bronchial Asthma Patients. Sci J Biol & Life Sci. 4(2): 2025. SJBLS. MS.ID.000583.
-
Allergy; biomarkers; bronchial asthma; immunity; inflammation
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






