 Research Article
Research Article
Measuring the Level of HbA1c (Glycated Hemoglobin) Among Patients with Diabetes: A Systematic Literature Review
Sarah Hussein Hamzah*
Bachelor’s degree in life sciences/microbiology department. Babylon/Iraq
Sarah Hussein Hamzah, Bachelor’s degree in life sciences/ microbiology department. Babylon/Iraq
Received Date: March 22, 2024; Published Date: April 04, 2024
Abstract
This systematic literature review aims to explore the measurement of HbA1c (Glycated Hemoglobin) levels among patients with diabetes. HbA1c is a crucial marker used to assess long-term glucose control in individuals with diabetes. The review will identify and analyze existing research on the measurement methods, interpretation of HbA1c levels, and their clinical implications for patients with diabetes. Additionally, the review will examine the relationship between HbA1c levels and diabetes management outcomes, such as glycemic control, complications, and overall health outcomes. The findings of this review will provide healthcare professionals with valuable insights into the interpretation and clinical implications of HbA1c levels, enabling them to optimize treatment plans and enhance the overall health and well-being of patients with diabetes.
Keywords: HbA1c; glycated hemoglobin; diabetes; measurement techniques; standardization; clinical implications
Introduction
Diabetes is a prevalent chronic condition that affects millions of individuals worldwide [1]. It is characterized by elevated blood glucose levels due to either insulin deficiency or insulin resistance [2]. Effective management of diabetes requires monitoring and maintaining optimal glucose control over the long term. HbA1c, also known as glycated hemoglobin, is a widely used marker for assessing average blood glucose levels over a period of 2-3 months [3]. HbA1c measurement plays a critical role in diabetes management as it provides valuable information about a patient’s glycemic control and helps healthcare professionals tailor treatment plans accordingly [4]. By assessing HbA1c levels, healthcare providers can evaluate the effectiveness of current treatment regimens, make necessary adjustments, and guide patients towards achieving optimal glucose control [5].
The measurement of HbA1c levels has evolved over the years, with various methods and techniques available for accurate assessment [6]. Laboratory-based assays and point-of-care testing are commonly used methods to measure HbA1c levels [7]. These measurements aid in understanding a patient’s average blood glucose levels, enabling healthcare professionals to make informed decisions regarding treatment strategies. Interpretation of HbA1c levels is crucial in clinical practice, as it helps establish target ranges for glycemic control in individuals with diabetes [8]. Different guidelines and recommendations exist regarding optimal HbA1c targets based on individual factors such as age, duration of diabetes, and presence of co-morbidities [9]. Understanding the interpretation of HbA1c levels can assist healthcare providers in setting realistic and achievable glycemic targets for their patients [10]. Furthermore, HbA1c levels have significant clinical implications for individuals with diabetes. Studies have shown that maintaining lower HbA1c levels is associated with reduced risks of diabetes-related complications, such as retinopathy, nephropathy, and cardiovascular diseases [11]. Monitoring HbA1c levels allows healthcare professionals to identify individuals at higher risk of complications and intervene accordingly to prevent or manage these adverse outcomes [3]. In light of the importance of HbA1c measurement in diabetes management, this systematic literature review aims to explore the various aspects related to the measurement of HbA1c levels among patients with diabetes. By analyzing existing research, this review will provide insights into the different measurement methods, interpretation of HbA1c levels, and the clinical implications of these levels for diabetes management outcomes. The findings of this review will contribute to enhancing the understanding and utilization of HbA1c measurement in clinical practice, ultimately improving the overall health and well-being of patients with diabetes.
Methods
To conduct this systematic literature review, a comprehensive
search will be performed in electronic databases, including
PubMed, Scopus, and Web of Science. The search strategy will be
developed using a combination of relevant keywords and Medical
Subject Headings (MeSH) terms. The search will be limited to
articles published between 2010 and 2023 to ensure the inclusion
of recent research. The following keywords and MeSH terms will
be used in the search strategy: “HbA1c,” “glycated hemoglobin,”
“diabetes,” “measurement,” “assay,” “laboratory,” “point-ofcare,”
“interpretation,” “clinical implications,” “glycemic control,”
“complications,” and “health outcomes.” These terms will be
combined using Boolean operators (AND, OR) to refine the search
and retrieve relevant articles.
a) Inclusion criteria for article selection will include
a. Studies published in English.
b. Studies focused on human subjects diagnosed with
diabetes.
c. Studies that discuss the measurement of HbA1c levels.
d. Studies that provide information on the interpretation of
HbA1c levels.
e. Studies that investigate the clinical implications of HbA1c
levels, including glycemic control, complications, and overall
health outcomes.
b) Exclusion criteria will include
a. Studies not published in English.
b. Studies that do not focus on HbA1c measurement in
patients with diabetes.
c. Studies that primarily focus on animals or in vitro
experiments.
d. Studies that are duplicates or have insufficient data.
The screening process will involve two stages: title and abstract screening, followed by full-text review. Two independent reviewers will conduct the screening process, and any disagreements will be resolved through discussion or consultation with a third reviewer if necessary. Data extraction will be performed using a standardized form, including study characteristics (e.g., author, year, and study design), measurement methods, interpretation of HbA1c levels, and clinical implications. The extracted data will be synthesized and analyzed to identify common themes, trends, and gaps in the literature as shown in Table 1. The quality of the included studies will be assessed using appropriate tools, such as the Newcastle- Ottawa Scale for observational studies or the Cochrane Risk of Bias tool for randomized controlled trials. This quality assessment will provide insights into the strength of evidence presented in the selected studies. The findings of this systematic literature review will be synthesized and presented in a narrative format, highlighting key findings and implications for clinical practice. Limitations of the included studies and potential areas for future research will also be discussed.
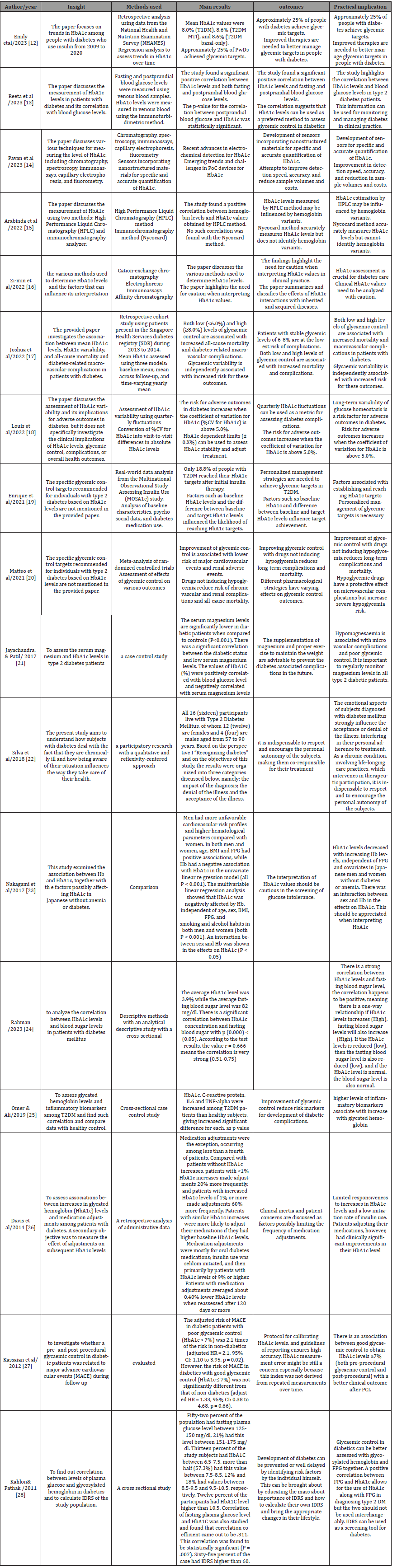
Table 1:Included Study Characteristics.
Results and Discussion
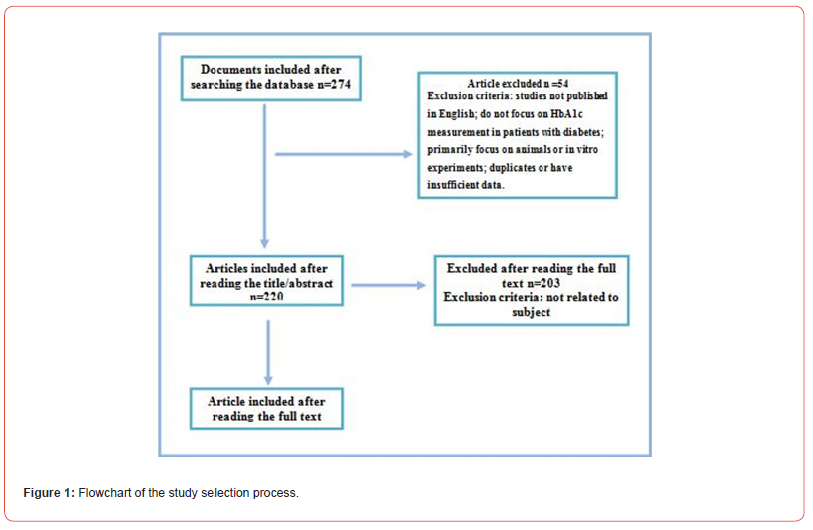
The systematic literature review revealed several key findings regarding the measurement of HbA1c levels among patients with diabetes as shown in Figure 1.
Measurement Methods
The review identified various measurement methods for HbA1c levels, including laboratory-based assays and point-of-care testing. Laboratory-based assays, such as high-performance liquid chromatography (HPLC), and immunoassays are commonly used in clinical settings for accurate and precise measurement of HbA1c levels. Point-of-care testing, on the other hand, offers the advantage of providing rapid results at the patient’s bedside or in community settings. Both methods have their advantages and limitations, and the choice of method depends on factors such as availability, cost, and convenience.
Interpretation of HbA1c Levels
The review found that interpretation of HbA1c levels is crucial for guiding diabetes management. Different guidelines and recommendations exist regarding target HbA1c ranges, depending on factors such as age, duration of diabetes, and presence of comorbidities. For most individuals with diabetes, the recommended target HbA1c level is below 7%. However, in certain populations, such as older adults or those with significant co-morbidities, a higher target range may be considered to avoid hypoglycemia and improve quality of life.
Clinical Implications
The review highlighted the clinical implications of HbA1c levels in diabetes management. Lower HbA1c levels have been associated with improved glycemic control and a reduced risk of diabetesrelated complications. Studies have shown that reducing HbA1c levels by 1% can lead to a significant decrease in the risk of micro vascular complications, such as retinopathy and nephropathy. Additionally, maintaining optimal HbA1c levels has been linked to a lower risk of cardiovascular diseases and mortality in individuals with diabetes. However, it is important to note that HbA1c levels alone do not provide a complete picture of diabetes management. Other factors, such as self-monitoring of blood glucose, patient adherence to treatment, and individualized care, also play crucial roles in achieving optimal glycemic control and preventing complications.
Limitations and Future Research
While the systematic literature review provided valuable insights, there were some limitations to consider. The included studies varied in design, sample size, and methodology, which may have influenced the overall findings. Additionally, most of the studies focused on Type 2 diabetes, and there were a limited number of studies specifically addressing HbA1c measurement in special populations, such as pregnant women or individuals with Type 1 diabetes. Future research should aim to address these gaps by conducting well-designed studies that explore the impact of HbA1c measurement on diabetes management outcomes in diverse populations. Additionally, the development of standardized protocols for HbA1c measurement and interpretation could further enhance the consistency and reliability of results.
Conclusion
In conclusion, this systematic literature review has provided valuable insights into the measurement of HbA1c levels among patients with diabetes. The review identified various measurement methods, including laboratory-based assays and point-of-care testing, and highlighted the importance of accurate and precise measurement for effective diabetes management. Interpretation of HbA1c levels is crucial in setting glycemic targets and guiding treatment plans, considering factors such as age, duration of diabetes, and co-morbidities. The clinical implications of HbA1c levels were also explored, revealing the association between lower HbA1c levels and improved glycemic control, reduced risk of complications, and better overall health outcomes. However, it is important to consider HbA1c levels in conjunction with other factors, such as self-monitoring of blood glucose and patient adherence to treatment, for comprehensive diabetes management. While the review provided valuable insights, it is important to acknowledge the limitations, such as variations in study design and the focus on specific populations. Future research should aim to address these limitations and further explore the impact of HbA1c measurement on diabetes management outcomes in diverse populations. Overall, this systematic literature review contributes to enhancing the understanding of HbA1c measurement in diabetes management. The findings can guide healthcare professionals in optimizing treatment plans, improving glycemic control, and ultimately enhancing the overall health and well-being of patients with diabetes.
Competing Interests
None to declare.
References
- Arokiasamy P, Salvi S, Selvamani Y (2021) Global burden of diabetes mellitus. In Handbook of Global Health. Cham: Springer International Publishing pp. 1-44.
- Lebovitz HE (2001) Insulin resistance: definition and consequences. Experimental and clinical endocrinology & diabetes 109(Suppl 2): S135-S148.
- Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK (2016) Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomarker insights 11(1): 95-104.
- Schnell O, Crocker JB, Weng J (2017) Impact of HbA1c testing at point of care on diabetes management. Journal of diabetes science and technology 11(3): 611-617.
- Sugandh FNU, Chandio M, Raveena FNU, Kumar L, Karishma FNU, et al. (2023) Advances in the management of diabetes mellitus: a focus on personalized medicine. Cureus 15(8): e43697-e43699.
- Karami A, Baradaran A (2014) Comparative evaluation of three different methods for HbA1c measurement with High-performance liquid chromatography in diabetic patients. Advanced biomedical research 3(1): 94-97.
- Jalali MT, Bavarsad SS, Hesam S, Afsharmanesh MR, Mohammadtaghvaei N (2020) Assessing agreement between the three common clinical measurement methods of HbA1c. Journal of Diabetes & Metabolic Disorders 19(1): 273-279.
- Haghighatpanah M, Nejad ASM, Haghighatpanah M, Thunga G, Mallayasamy S (2018) Factors that correlate with poor glycemic control in type 2 diabetes mellitus patients with complications. Osong public health and research perspectives 9(4): 167-174.
- Milosevic D, Panin VL (2019) Relationship between hematological parameters and glycemic control in type 2 diabetes mellitus patients. Journal of Medical Biochemistry 38(2): 164-171.
- Simmons D, Simmons D, Hlaing T (2014) Interpretation of HbA1c: association with mean cell volume and haemoglobin concentration. Diabetic Medicine 31(11): 1387-1392.
- Boye KS, Thieu VT, Lage MJ, Miller H, Paczkowski R (2022) The association between sustained HbA1c control and long-term complications among individuals with type 2 diabetes: a retrospective study. Advances in Therapy 39(5): 2208-2221.
- Emily R Hankosky, Karli B Gunn, Elizabeth Lubelczyk, Jessica Mitroi, David R Nelson, et al. (2023) Gaps Remain for Achieving HbA1c Targets for People with Type 1 or Type 2 Diabetes Using Insulin: Results from NHANES 2009–2020. Diabetes Therapy 14(6): 967-975.
- Reeta Baishya, Madhurima Bora, Arijit Mazumdar (2023) A cross sectional study to determine the correlation of blood glucose and HbA1C in type 2 diabetes mellitus patients. International Journal of Research in Medical Sciences 11(3): 874-879.
- Pavan Kumar Mandali, A Prabakaran, Kasthuri Annadurai, Uma Maheswari Krishnan (2023) Trends in Quantification of HbA1c Using Electrochemical and Point-of-Care Analyzers. Sensors 23(4): 1901-1905.
- Arabinda Mohan Bhattarai, Sulochana Parajuli, Salina Pradhananga (2022) Variation of HbA1c with Hemoglobin level: A comparative study between High Performance Liquid Chromatography and Immunochromatography Analyzer. Medical Journal of Shree Birendra Hospital 21(2): 46-48.
- Zi min Chen, Limei Shao, Mingfeng Jiang, Xue Ying Ba, Bingjie Ma, et al. (2022) Interpretation of HbA1c lies at the intersection of analytical methodology, clinical biochemistry and hematology (Review). Experimental and Therapeutic Medicine 24(6): 707-710.
- Joshua Kuan Tan, Gek Hsiang Lim, Nur Nasyitah Mohamed Salim, S Chia, Julian Thumboo, et al. (2022) Associations Between Mean HbA1c, HbA1c Variability, and Both Mortality and Macrovascular Complications in Patients with Diabetes Mellitus: A Registry-Based Cohort Study. Clinical Epidemiology 15(1): 137-149.
- Louis Monnier, Claude Colette, Fabrice Bonnet, Eric Renard, David Owens (2022) HbA1c variability and diabetes complications: assessment and implications. Diabetes & Metabolism 49(1): 101399-101405.
- A Enrique Caballero, Beth L, Nordstrom, Birong Liao, Ludi Fan, Nan Zhang, et al. (2021) Individualized HbA1c target selection and achievement in the Multinational Observational Study Assessing Insulin Use (MOSA1c) type 2 diabetes study. Journal of Diabetes and Its Complications 35(11): 108011-108015.
- Matteo Monami, Riccardo Candido, Basilio Pintaudi, Giovanni Targher, Edoardo Mannucci, et al. (2021) Improvement of glycemic control in type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Nutrition Metabolism and Cardiovascular Diseases 31(9): 2539-2546.
- Jayachandra S, Patil S (2017) A Case Control Study of Levels of Serum Magnesium and HbA1c among Patients with Type 2 Diabetes. International Journal of Physiology 5(1): 180-183.
- Silva JR, Souza EC, Echazú Böschemeier AG, Costa C, Bezerra HD, Feitosa EE (2018) Diagnosis of diabetes mellitus and living with a chronic condition: participatory study. BMC Public Health 18(1): 699-704.
- Nakagami T, Oya J, Kasahara T, Uchigata Y (2017) Effect of Hemoglobin Levels and Sex on HbA1c Levels among Japanese Population. Diabetes and Endocrinology 1(1): 3-8.
- Rahman R, Amalia FN, Sakdiah S, SAJ (2023) Correlation Between Glycated Hemoglobin (Hba1c) Levels and Fasting Blood Glucose Levels in Patients with Diabetes Mellitus in Jambi City. Proceeding International Conference Health Polytechnic of Jambi 2(1): 108-111.
- Omer MA, Ali AE (2019) Relationship between hba1c levels and inflammatory biomarkers (c - reactive protein, il6 and tnf-alpha) among type 2 diabetes mellitus-khartoum- sudan. International Journal of Medical and Biomedical Studies 3(3): 195-201.
- Davis JW, Chavez B, Juárez DT (2014) Adjustments to Diabetes Medications in Response to Increases in Hemoglobin A1c. Annals of Pharmacotherapy 48(1): 41-47.
- Kassaian SE, Goodarzynejad H, Boroumand MA, Salarifar M, Masoudkabir F, et al. (2012) Glycosylated hemoglobin (HbA1c) levels and clinical outcomes in diabetic patients following coronary artery stenting. Cardiovascular diabetology 11(1): 82-92.
- Kahlon AS, Pathak R (2011) Patterns of glycemic control using glycosylated hemoglobin in diabetics. Journal of Pharmacy and Bioallied Sciences 3(3): 324-328.
-
Sarah Hussein Hamzah*. Measuring the Level of HbA1c (Glycated Hemoglobin) Among Patients with Diabetes: A Systematic Literature Review. Sci J Biol & Life Sci. 3(4): 2024. SJBLS.MS.ID.000568.
-
HbA1c; glycated hemoglobin; diabetes; measurement techniques; standardization; clinical implications
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






