Case Report
Case Report
Congenital Epidermoid Cyst in the Uvula of a Child: Case Report and Literature Review
Natalia Gabriela Sanchez1, Hiram Alvarez Neri2 and Alvaro Lezid Padilla Rodriguez3*
1Digital Pathology Laboratory, Instituto Tecnológico y de Estudios Superiores De Monterrey Campus Mexico, Mexico
2Private Children’s Hospital, Dalinde Medical Center, Mexico
3Digital Pathology Laboratory, School of Medicine Universidad Panamericana Campus Mexico City, School of Medicine Instituto Tecnológico y de Estudios Superiores De Monterrey Campus Mexico City, Mexico
Alvaro Lezid Padilla Rodríguez, Digital Pathology Laboratory, School of Medicine Universidad Panamericana Campus Mexico City, School of Medicine Instituto Tecnológico y de Estudios Superiores De Monterrey Campus Mexico City, Mexico.
Received Date:March 17, 2023; Published Date:April 11, 2023
Abstract
Epidermoid cysts are benign stratified-squamous epithelium-lined lesions that may be congenital or acquired (trauma or surgery). They are rare in the oral cavity, being more frequent on the mouth’s floor, and extremely rare in the uvula. To the best of our knowledge, only 14 cases of epidermoid cysts in the uvula have been reported to date. We present a case of a 3-year-old boy with an incidental finding of a uvular epidermoid cyst. The pathogenesis, diagnosis, and treatment of this rare entity are discussed.
Keywords:Epidermoid cyst; Uvula; Congenital; Oral
Introduction
Epidermoid cysts are benign lesions with stratifiedsquamous epithelial lining containing fluid or semisolid material. Approximately 7% occur in the head and neck, and only 1.6% occur in the oral cavity, mainly on the mouth’s anterior floor [1,2]. A comprehensive review of English and Spanish literature by searching the databases using the terms “epithelial cyst uvula” and “epidermoid cyst uvula”, without date restrictions, disclosed only 14 confirmed cases [3-13]. We report a case of a 3-year-old male with a mass at the uvular tip. We provide a comprehensive review of existing cases.
Case Report
A 3-year-old male with a history of isolated episodes of regurgitation came for consultation for a slowly-growing small white mass in the uvula that had been noticed by his mother for the past three months. The patient was in good health, and his medical history was uneventful. Physical examination revealed a wellcircumscribed, smooth, yellow-white, oval lesion that measured approximately 1 cm located on the tip of the uvula (Figure 1).
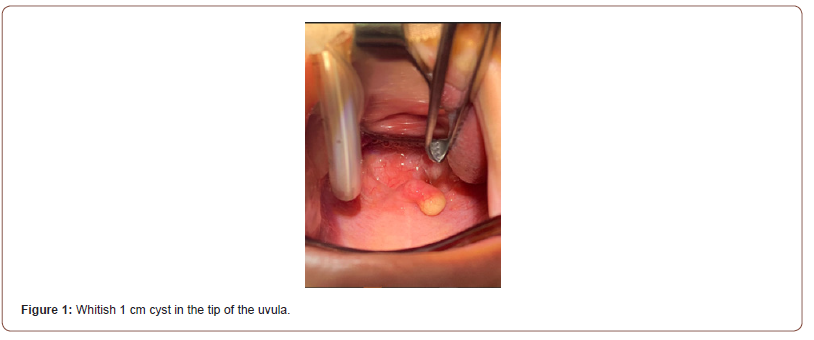
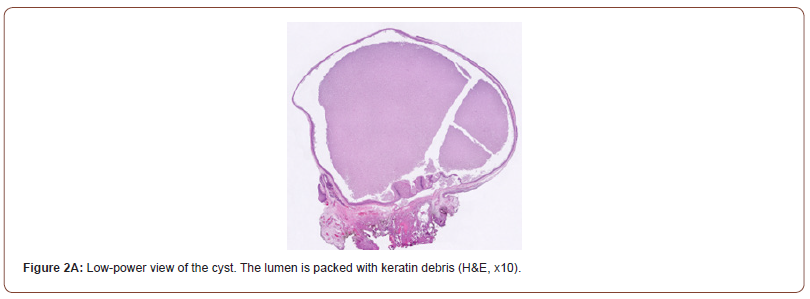
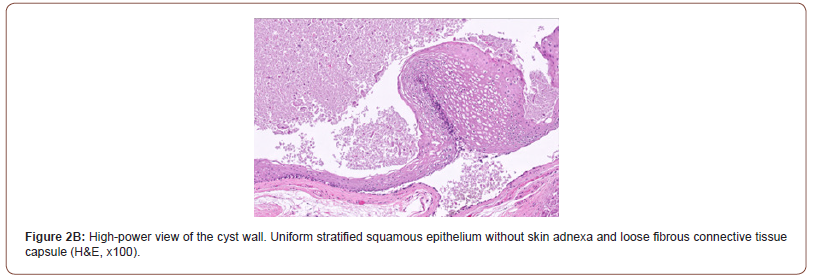
The rest of the physical examination was unremarkable. A clinical diagnosis of uvular cyst was made, and the lesion was completely excised under general anesthesia without surgical or postoperative complications. Grossly, the surgical specimen consisted of a smooth-surfaced, oval, soft, yellowish-white nodule that measured 7 x 6 x 5 mm. A thin fibrous tissue capsule formed the cyst’s wall, and the cut surface showed a central cavity filled with yellowish-white, pasty material. Microscopically, sections of the specimen showed a cyst with luminal keratin debris (Figure 2A), lined by stratified squamous epithelium without skin appendages and an underlying loose fibrous connective tissue (Figure 1A, 2B).
Based on these findings, the case was diagnosed as a completely excised epidermoid cyst of the uvula. The patient had no recurrence at a one-month follow-up.
Discussion
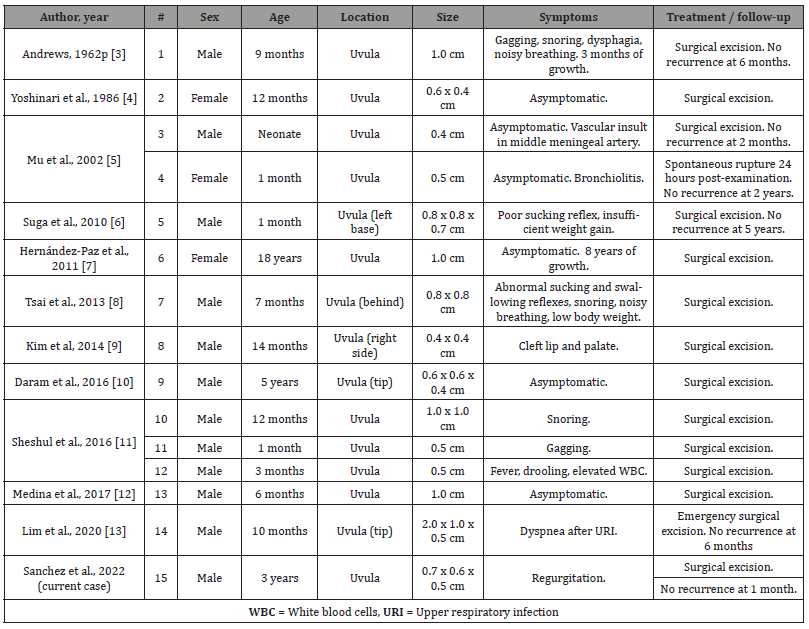
Epidermoid cysts are benign, slowly-enlarging lesions, either congenital or acquired, due to trauma or surgery. These cysts can arise anywhere in the body, with an incidence of 7% in the headand- neck region and 1.6% in the oral cavity [2]. Only 14 cases have been described in the uvula (Table 1) [3-13].
In this rare location, they are predominant in males with a male: female ratio of 4:1, all in the pediatric population, with a median age of 9 months. Most epidermoid cysts are acquired lesions, most likely due to trauma or iatrogenic introduction of epithelial cells into deep tissue during surgery [10]. However, in the uvula, the pathogenesis seems to be congenital, as all cases have occurred in pediatric patients with no history of trauma or prior intubation. The origin is, therefore, likely due to a developmental defect where remnants of ectodermal debris are trapped during the fusion of the maxillary process to form the palate between the 6th and 12th week of embryological development [4,8,10,11].
In this zone, they are generally asymptomatic, slowly enlarging lesions [4,5,7,10,12] that can eventually grow, causing obstructive symptoms such as snoring [3,8,11], gagging [3,11], dysphagia [3,11], mouth breathing [3,8], poor sucking reflex [6,8], and insufficient weight gain [6,8]. Some cases presented with simultaneous upper respiratory infections, which caused airway obstruction [11,13] and even required emergency surgery in one case [13]. Our patient´s new onset regurgitation was likely caused as a result of this entity. Imaging is not required for diagnosis as a cyst in the uvula is easily identified on physical examination and accessible for surgical resection. They are usually located at the tip [10,13]; however, they may be present laterally [6,9], or behind the uvula [8]. MRI may be necessary if malignancy is suspected; however, no cases of malignant transformation have been described in the uvula [7,12].
Table 1:Epidermoid Cysts in The Uvula.
Macroscopically, epidermoid cysts in the uvula range from 0.4- 2 cm (average 0.78 cm). They are well-circumscribed, spherical to oval, yellowish-whitish in appearance with a thin capsule. On the cut surface, they contain fluid or semisolid material. A histologic examination is required for a definitive diagnosis. Epidermoid cysts are characterized by a fibrous connective tissue wall lined by a layer of stratified-squamous epithelium without skin adnexa. The lumen is filled with variable amounts of keratin debris. Mass lesions in the uvula can be caused by dermoid cysts, teratoid cysts, mucoceles, and branchial cleft cysts. In 1955, Meyer established a morphologic classification for cysts on the floor of the mouth as either dermoid, epidermoid, or teratoid. Epidermoid cysts are lined only by stratified-squamous epithelium; Dermoid cysts also include skin adnexa; and Teratoid cysts include mature tissue representing at least two embryonic layers (endoderm, mesoderm, or ectoderm) [14]. Mucoceles are not lined by any kind of epithelium. Branchial cleft cysts are lined by stratified-squamous or ciliated columnar epithelium and have a fibrous wall with lymphoid follicles.
Complete transoral surgical excision is the treatment of choice, even in neonates [3-13]. Early excision can prevent clinical complications such as airway obstruction [13]. The well-defined borders of the cysts facilitate surgical resection, and no recurrence has been described. Fine needle aspiration and fenestration are not recommended due to the risk of infection, which can cause pain and worsen clinical symptoms [6]. On rare occasions, the cyst can spontaneously rupture without further recurrence [5].
Conclusion
Epidermoid cysts in the uvula are rare benign tumors formed by ectodermal entrapment during the fusion of maxillary processes to form the palate. It presents more commonly in males, and all cases have presented in pediatric patients. Clinical presentation is usually asymptomatic but may cause obstructive symptoms when size is considerable. In the evaluation of cystic lesions of the uvula, the differential diagnosis should include epidermoid cyst, dermoid cyst, teratoid cyst, mucocele, and branchial cleft cyst. Complete surgical excision provides both the definitive diagnosis and curative treatment, and the procedure is usually well tolerated. Pediatricians, otolaryngologists, and pathologists should be aware of the occurrence of epidermoid cysts in the uvula, as early detection and management prevent complications.
Conflict of Interest
No conflict of interest.
Acknowledgment
None.
References
- New GB, Erich JB (1937) Dermoid Cyst of the Head and Neck. Surgery, Gynecology Obstetrics 65: 48-56.
- Turetschek K, Hospodka H, Steiner E (1995) Case report: epidermoid cyst of the floor of the mouth: diagnostic imaging by sonography, computed tomography and magnetic resonance imaging. Br J Radiol 68(806): 205-207.
- Andrews BF (1962) Epidermal Inclusion Cyst of the Uvula in Infancy. American Journal of Diseases of Children 103: 174-176.
- Yoshinari M, Nagayama M (1986) Epidermoid cyst of the uvula: report of a case. J Oral Maxillofac Surg 44(10): 828-829.
- Mu SC, Sung TC, Yeh ML, Hsu S te, Lin MI, et al. (2002) Solitary epithelial cyst of the uvula in the neonate: case reports and review of the literature. Pediatr Emerg Care 18(2): 93-94.
- Suga K, Muramatsu K, Uchiyama T, Takano N, Shibahara T (2010) Congenital Epidermoid Cyst Arising in Soft Palate Near Uvula: A Case Report. Bull Tokyo Dent Coll: 207-11.
- Hernandez-Paz SH, Garcia-Guzman CM, Morales-Ayala LL (2011) Epidermoid cyst in the uvula. Revista de Especialidades Medico-Quirurgicas 16: 182-187.
- Tsai WC, Kuo CY, Wang CH (2013) Epidermal inclusion cyst of the soft palate and uvula in an infant. Eur J Pediatr 172(11): 1563-1564.
- Kim Y-B, Yang J-Y, Leem D-H, Baek J-A, Ko S-O, et al. (2014) Epithelial Cyst of the Uvula with Unilateral Complete Cleft Lip and Palate. Maxillofac Plast Reconstr Surg 36: 13-15.
- Daram S, Ulualp SO, Uddin N (2016) Epidermoid cyst of the uvula in a child. SAGE Open Med Case Rep 4: 2050313X1668362.
- Seshul M, Wiatrak BJ, Tseng E, Kelly DR (1998) Isolated Epithelial Cysts of the Uvula in Children: A Report of Three Cases. Annals of Otology, Rhinology & Laryngology 107: 717-719.
- Medina B, Ruiz-Diaz O, Gomez O, Franco L, Rodriguez I, et al. (2017) Epidermoid Cyst of Uvula: Presentation of Case. Review of the Literature. International Journal of Medical and Surgical Sciences 4: 1101-1107.
- Lim HR, Cho HH, Yang HC, Kim HC (2020) An epidermoid cyst of the uvula causing dyspnea in an infant: A case report. Medicine 99(46): e22573.
- Meyer I (1995) Dermoid cysts (dermoids) of the floor of the mouth. Oral Surg Oral Med Oral Pathol 8(11): 1149-1164.
-
Natalia Gabriela Sanchez, Hiram Alvarez Neri and Alvaro Lezid Padilla Rodriguez*. Congenital Epidermoid Cyst in the Uvula of a Child: Case Report and Literature Review. Open J Pathol Toxicol Res. 1(3): 2023. OJPTR.MS.ID.000515.
-
Congenital, Epidermoid, Child, Pathology, Epidermoid cyst; Uvula; Congenital; Oral, cavity, surgery, trauma male: female.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.