 Case Report
Case Report
Recalcitrant Neck Abscesses as a Late Complication of Neck Liposuction: Case Report
Eduardo Lopez Orozco*
Otolaryngology Head and Neck Surgery, Universidad de Guadalajara, Mexico
Eduardo Lopez Orozco, Private Practice, Niños Heroes 1921-1 Guadalajara, Jalisco, Mexico.
Received Date: June 24, 2024; Published Date: July 02, 2024
Abstract
An otherwise healthy 29-year-old female presented with a slowly growing neck abscesses 5 months after having a neck liposuction performed. In this case report we discuss the diagnostic and therapeutic approach underwent in order to elucidate this difficult diagnosis. After negative laboratory tests and inconclusive pathology reports, PCR for atypical mycobacteria was performed on a sample of the granulomatous tissue. This exam yielded a positive result for M. abscessus, which allowed us to instate a targeted antimicrobial therapy. Infections with M. abscessus are uncommon because this type of mycobacteria is an opportunistic pathogen that depends on direct inoculation to cause infection. Outbreaks have been identified in places performing procedures with improper equipment sterilization techniques. The conclusion is that adequate equipment sterilization should not be spared to avoid these infections. A high suspicion for atypical mycobacteria should be present in patients with this type of recalcitrant neck infections.
Keywords: Atypical mycobacteria; Neck abscess; Deep neck infection; Mycobacterium abscessus; Liposuction complication
Abbreviations: PCR-Polymerase Chain Reaction; RGM-Rapidly Growing Mycobacteria; SGM-Slowly Growing Mycobacteria
Introduction
The neck is a region full of delicate and vital structures; thus, a timely and correct diagnosis is needed in its diseases. Complications after neck surgery tend to be immediate, and include bleeding, hematomas, seromas, facial nerve paralysis, and hypertrophic scars [1]. However, subacute or even chronic complications can be found up to 6 months after the initial procedure. The present case was a diagnostic challenge since the patient did not present the expected response to the medical and surgical therapies offered for an apparent deep neck infection with multiple abscesses formation. This was specially challenging since the first neck liposuction procedure was performed by another surgeon, leaving us with no information regarding the procedure technique or the findings during said procedure. The purpose of presenting this case is to raise awareness of this rare-but difficult to diagnose-infections, and to recommend prevention of said infections with adequate instruments sterilization techniques.
Case Presentation
A 29-year-old woman came to our clinic with the chief complaint of a painful neck mass. The patient is otherwise healthy, and her only past medical history is a surgical procedure performed 5 months ago in an unknown location, where they performed rhinoplasty, removal of Bichat fat pads and neck liposuction.
The patient states that her problem began one month after her surgery with sudden apparition of painful nodules all around her neck, and feeling her face was “swollen”. She commented this with her previous surgeon, who told her that was ok and proceeded to apply subcutaneous steroids (dexamethasone) in the lesions. As time kept passing the nodules in the neck grew larger in size, more tender and more painful, up to the point of causing her shortness of breath when lying supine. She was approached by an internal medicine physician, who ordered an MRI and referred her to our clinic.
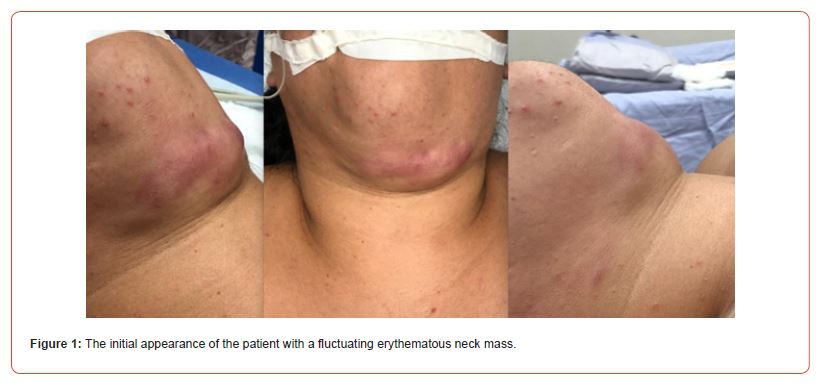
Upon inspection, the patient had a tender and fluctuating mass, an abscess, in the left submandibular area, expanding to the submental area. The skin was erythematous and in the surrounding region there were red nodules (Figure 1). Otherwise, the physical exam was unremarkable.
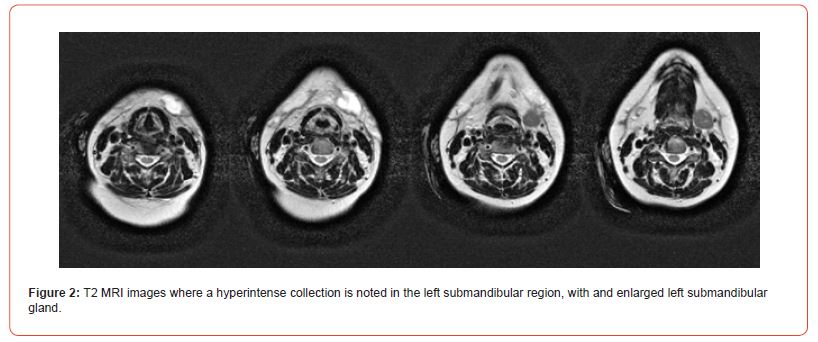
T2 sequence in the MRI showed a localized round hyperintense area in the left submandibular area extending from the glottic region to the submandibular gland; the left submandibular gland also looks enlarged (Figure 2).
The patient underwent incision and drainage of the abscess. About 15ml of yellow cloudy apparently purulent material was obtained upon incision of the skin (Figure 3). The platysma was erythematous and swollen, and a vast amount of fibrotic and inflammatory material was found, samples were taken for pathology. The patient was treated with broad spectrum antibiotics postoperatively (ceftriaxone and clindamycin).

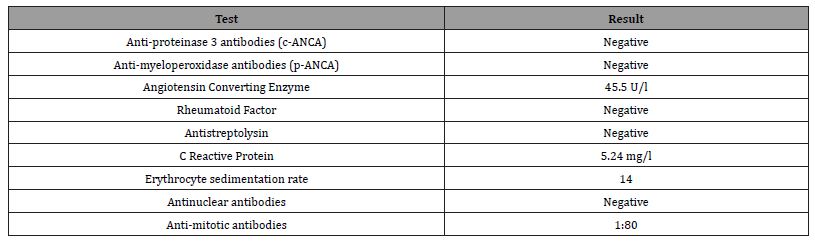
Even though the surgical procedure appeared to be successful, two weeks after the incision and drainage the patient developed new small abscesses in the neck region. These lesions were very painful, kept growing and occasionally drained a fluid (Figure 4). Lab tests were performed suspecting an autoimmune disease, but every reactive was negative (Table 1).
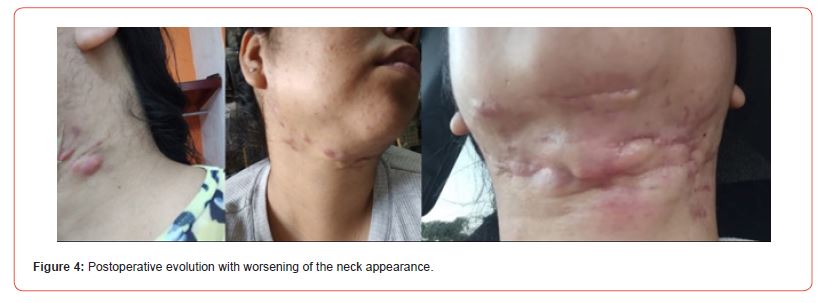
Table 1:Laboratory results.
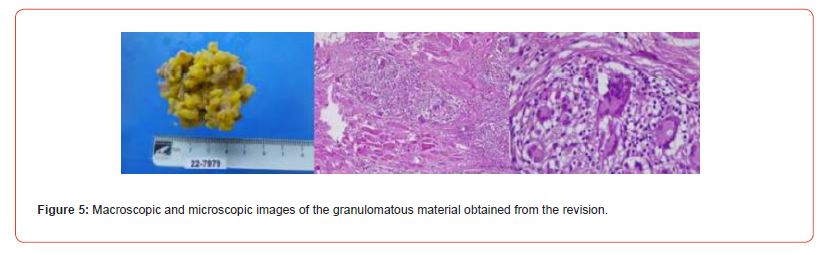
The patient was taken again to the Operating Room for a revision. During the surgery we found fibrosis, some sutures and granulomatous tissue. Again, samples were sent to pathology.
Pathology reported chronic granulomatous foreign body inflammatory reaction. It was negative to Ziehl-Neelsen and Periodic- Acid Schiff stains (Figure 5).
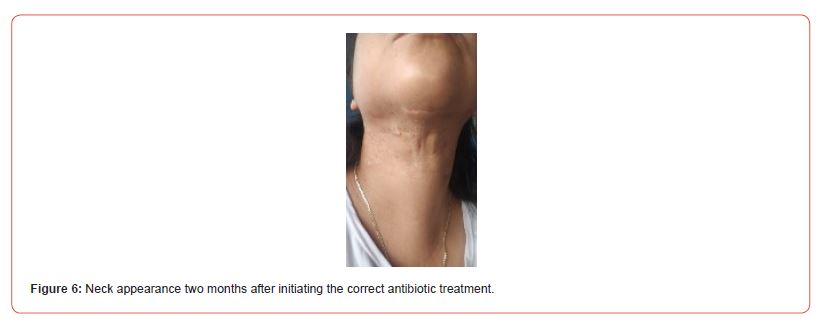
Atypical mycobacteria Polymerase Chain Reaction was performed on the obtained tissue, which yielded a positive result for Mycobacterium abscessus. The patient was started on a long-term antibiotic treatment consisting of moxifloxacin, doxycycline and clarithromycin, and the appearance of the skin in her neck improved considerably (Figure 6).
Discussion
Mycobacterium abscessus belongs to the family of the mycobacteria, which belong to the phylum of the Actinobacteria. These microorganisms are characterized by their branching filaments and for being microaerophilic [2]. Up to 95% of these organisms are found living freely in the environment: in the soil, air and water [3]. Atypical or non-tuberculous mycobacteria are strict opportunistic pathogens causing mainly infections in the skin and mucous membranes. They are classified according to their growth rate into rapidly growing (which form colonies in less than 7 days), and slowly growing mycobacteria. Rapidly growing mycobacteria (RGM) include M. abscessus, M. chelonae, M. bolletti and M. masiliense. Slowly growing mycobacteria include M. marinum, M. ulcerans, M. avium complex, M. kansaii, amongst others [2].
M. abscesus previously comprised three subspecies which are currently understood as different organisms: M. abscessus subesp. abscessus, M. abscessus subesp. massiliense, and M. abscessus subesp. Bolletii [4]; nevertheless, the proportion amongst M. abscessus and M. massiliense is almost the same [5], M. bolletii is rarely identified [4]. These bacteria are difficult to diagnose, so DNA tests with DNA sequencing, polymerase chain reaction or restriction endonuclease assay are recommended for a species-specific diagnosis [6].
Clinical manifestations of RGM include localized abscess formation and ulcers. The spectrum of diseases generated by these organisms greatly varies depending on the state of the host: they can cause respiratory tract infections in people with structural lung disease, central nervous infections in HIV-infected patients, or more commonly skin and soft tissue infection [4]. The presentation of the skin and soft tissue infection also varies, with a range of presentations going from cutaneous tender nodules to abscesses, passing through erythematous papules of pustules [7].
In healthy individuals the main risk factor for infection is direct insemination of the organism via trauma and surgical or cosmetic procedures [8]. Procedures that have been associated with RGM infection are liposuction, acupuncture, pedicures, subcutaneous injection, amongst others [8]. Outbreaks have been identified in Brazil where 311 patients were infected with the same strain of mycobacteria, apparently due to inconsistent cleaning and disinfection procedures performed in the surgical instruments [9]. In Spain another outbreak of M. abscessus was identified in 17 patients who underwent mesotherapy treatment in an aesthetic clinic that apparently employed contaminated products [10]. Other reports include tender lumps 6 weeks after performing dermabrasion at home, the patient was diagnosed with M. abscessus and treated with IV antibiotics [11].
This was a difficult case to diagnose that provoked a lot of discussion and pathophysiologic theories. Upon finding a patient that underwent a neck liposuction and that developed an enlarging fluid collection in the neck we had some differential diagnoses. One possibility we considered was a sialocele: we hypothesized that the platysma was violated during the liposuction, the submandibular gland injured, and the collection was purely fluid. Another hypothesis was foreign body reaction to sutures or any of the materials used in the previous surgery. Rheumatologic and infectious conditions were also considered and assessed.
Conclusion
The first point to take away is that this type of infections can be prevented if adequate disinfection is performed in the surgical instruments. Although mycobacteria are generally resistant, it has been shown that ethyl alcohol 50% and 70%, benzyl-4-chlorophenol/ phenylphenol 1%, and sodium chlorite (1:5:1) are effective against mycobacteria in less than 1 minute contact time. Sodium hypochlorite (50,000 mg/l) requires 10 minutes contact time to reduce bacterial counts. However, N-alkyl dimethyl benzyl ammonium chloride (1:256), and potassium peroxymonosulfate-sodium chloride (1%) did not reduce bacterial counts after 60 minutes [12]. Other problems relating to the disinfection process include lack of cleaning of the lumen of cannulas which can harbor biofilms, low concentrations of the sterilizing substance or a lack of contact time [9, 13]. Thus, although preparation of the equipment is a step often overlooked by the surgeon, in situations such as this one, it is extremely important to ensure the sterility of the equipment.
Atypical mycobacteria infection is a diagnosis that should be considered in patients with abscesses that keep proliferating despite treatment with broad spectrum antibiotics and adequate incision and drainage. It is important to have in mind that the main risk factor in healthy patients is a previous surgical or cosmetic procedure with contaminated instruments or devices. Therefore, while obtaining the history, emphasis must be made to investigate whether the patient has had surgeries, acupuncture, dermabrasion, tattoos, microblading, etc. Even when pathology reports are negative, and all other diagnostic options have been exhausted, molecular studies such as PCR should be performed if the clinical suspicion exists. This type of studies also provide the advantage that they can assess antibiotic susceptibility to instate the best antibiotic treatment, since most of this bacteria present multiple antibiotic resistances.
Acknowledgment
None.
Conflict of Interest
The author reports no conflict of interest.
References
- Diniz DA, Gonçalves KKN, Silva CCG, de Araújo ESM, Carneiro SC de AS, et al. (2022) Complications associated with submental liposuction: a scoping review. Med Oral Patol Oral Cir Bucal [Internet]. 27(3): e257.
- Johansen MD, Herrmann JL, Kremer L (2020) Non-tuberculous mycobacteria and the rise of Mycobacterium abscessus. Nat Rev Microbiol 18(7): 392-407.
- Angenent LT, Kelley ST, St. Amand A, Pace NR, Hernandez MT (2005) Molecular identification of potential pathogens in water and air of a hospital therapy pool. Proc Natl Acad Sci U S A 102(13): 4860-4865.
- Lee MR, Sheng WH, Hung CC, Yu CJ, Lee LN, et al. (2015) Mycobacterium abscessus complex infections in humans. Emerg Infect Dis 21(9): 1638-1646.
- Teng SH, Chen CM, Lee MR, Lee TF, Chien KY, et al. (2013) Matrix-Assisted Laser Desorption Ionization-Time of Flight Mass Spectrometry Can Accurately Differentiate between Mycobacterium masilliense ( abscessus subspecies bolletti) and M. abscessus (Sensu Stricto). J Clin Microbiol 51(9): 3113.
- Griffith DE, Aksamit T, Brown Elliott BA, Catanzaro A, Daley C, et al. (2007) An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med (4): 367-416.
- Kothavade RJ, Dhurat RS, Mishra SN, Kothavade UR (2013) Clinical and laboratory aspects of the diagnosis and management of cutaneous and subcutaneous infections caused by rapidly growing mycobacteria. Eur J Clin Microbiol Infect Dis 32(2): 161-188.
- Uslan DZ, Kowalski TJ, Wengenack NL, Virk A, Wilson JW (2006) Skin and soft tissue infections due to rapidly growing mycobacteria: comparison of clinical features, treatment, and susceptibility. Arch Dermatol 142(10): 1287-1292.
- Viana Niero C, Lima KVB, Lopes ML, Rabello MCDS, Marsola LR, et al. (2008) Molecular Characterization of Mycobacterium massiliense and Mycobacterium bolletii in Isolates Collected from Outbreaks of Infections after Laparoscopic Surgeries and Cosmetic Procedures. J Clin Microbiol 46(3): 850.
- Galmés Truyols A, Giménez Duran J, Bosch Isabel C, Nicolau Riutort A, Vanrell Berga J, et al. (2011) An outbreak of cutaneous infection due to Mycobacterium abscessus associated to mesotherapy. Enferm Infecc Microbiol Clin 29(7): 510-514.
- Grubbs J, Bowen C (2019) Mycobacterium abscessus infection following home dermabrasion. Cutis 104(1): 79-80.
- Mainous ME, Smith SA (2011) Efficacy of Common Disinfectants against Mycobacterium marinum. J Aquat Anim Health 17(3): 284-288.
- Sattar SA, Best M, Springthorpe VS, Sanani G (1995) Mycobactericidal testing of disinfectants: an update. J Hosp Infect 30(SUPPL.): 372-382.
-
Eduardo Lopez Orozco*. Recalcitrant Neck Abscesses as a Late Complication of Neck Liposuction: Case Report. On J Otolaryngol & Rhinol. 7(1): 2024. OJOR.MS.ID.000653.
-
Neck abscesses; Neck liposuction; Granulomatous tissue; Neck infections Submandibular area; Autoimmune disease; Granulomatous tissue; Soft tissue; Facial nerve paralysis; Neck grew
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






