 Research Article
Research Article
Pressure-Less Acoustic Immittance Measurements of Patients with Persistent Ventilation Disorders
Moayad Anbari1, Shirin Zhumabaeva2, Munar Beishenova2, Dörte Fischer1,3, Shayirbek Sulaimanov2 and Tino Just1*
1Department of Otorhinolaryngology, Head and Neck Surgery, KMG Klinikum, Güstrow, Germany
2Department of Otorhinolaryngology, The National Center of Maternity and Childhood Care, Bishkek, Kyrgyzstan
3Department of Audiology, KMG Klinikum, Güstrow, Germany
Moayad Anbari (OCRID-ID: 0009-0003-5565-6437)
Dr. Shirin Zhumabaeva (OCRID-ID: 0000-0002-9073-1127)
Dr. Munar Beishenova (OCRID-ID: 0009-0000-8375-2563)
Dr. Dörte Fischer (OCRID-ID: 0000-0003-3736-4441)
Professor Shayirbek Sulaimanov (OCRID-ID: 0000-0002-0980-0501)
Professor Tino Just (OCRID-ID: 0000-0003-2036-8569)
Tino Just, M.D, Department of Otorhinolaryngology, Head and Neck Surgery Friedrich-Trendelenburg-Allee 1, D-18273 Güstrow, Germany
Received Date: January 02, 2025; Published Date: January 15, 2025
Abstract
This study presents pressure-less acoustic immittance (PLAI) measurements in patients with chronic ventilation disorders. An acoustic signal (100 - 3000 Hz) is introduced into the outer ear canal, allowing for determining the resonance frequency (RF) and the admittance peak.
This study aims to re-evaluate test results in patients with chronic tube ventilation disorders using PLAI in conjunction with tympanometry, pure tone audiometry, and otoscopy.
Material and Methods: PLAI measurements were conducted using a CE-certified system, MedWave® (Neuranix, Italy). In this prospective study, 135 subjects from two Departments of Otorhinolaryngology were included, with a mean age of 53.3 ± 17.6 years (79 men and 56 women). This group consisted of 99 patients (45 unilateral and 54 bilateral) with middle ear disorders and 36 healthy subjects with normal bilateral ears.
All participants, including patients with chronic ventilation disorders and 36 healthy subjects, underwent a comprehensive medical evaluation, which included ear, nose, and throat examinations, video otoscopy, pure tone audiometry, PLAI measurement using MedWave®, conventional single- frequency tympanometry, and video endoscopy with Valsalva maneuver (a forceful attempt of exhalation against a closed airway) for patients with tube ventilation issues.
Results: Among the 37 ears with tube ventilation disorders (mesotympanic and/or epitympanic retraction, adhesive process, hyperectasis) without middle ear effusion, an average resonance frequency of 440 Hz ± 180.1 Hz (ranging from 161.5 to 1109 Hz) and an average peak of 2.00*10-2 mmho ranging from .62 to 4.41*10-2 mmho was determined. It was shown that a slight retraction of the tympanic membrane could lead to the PLAI diagnosis of “normal” or “soft,” while cases with fixation of the ossicular chain, confirmed by middle ear surgery, were diagnosed as “rigid.”
Conclusion: This study demonstrates the implementation of PLAI and the interpretation of the PLAI measures in conjunction with otoscopy, audiometry, and single-frequency tympanometry in patients with chronic tube ventilation disorders. The incorporation of PLAI into the diagnostic battery appears to predict early-stage fixation of the ossicular chain, particularly in strong epitympanic retraction pockets.
Introduction
Tube ventilation problems may arise when the mucosa of the Eustachian tube is swollen or fails to open or close properly [1]. This dysfunction can occur during upper airway infections, nasal septal deviation [2], rhinosinusitis, allergic rhinitis [3], obstruction of the nasopharynx due to adenoids or tumor [1], cleft palate [4], trauma, cancer treatment, or sometimes without any identifiable cause. Patients with tube dysfunction often report symptoms such as difficulties in pressure equalization, ear pressure, aural fullness, pain, tinnitus, and mild hearing loss. Long-term ventilation issues can lead to damage of the middle ear mucosa and tympanic membrane, resulting in complications such as tympanic membrane retraction, atelectatic ear, adhesion of the atrophic tympanic membrane, otitis media with effusion, and chronic otitis media [5]. Currently, there are no comprehensive guidelines for diagnosing chronic tube ventilation disorders [6].
In clinical practice, medical history, nasal endoscopy, otoscopy, and audiological tests, such as pure tone audiometry and tympanometry, are employed to assess the status of the outer ear canal, tympanic membrane, and middle ear. Otoscopy also includes pneumatic otoscopy to evaluate the movement of the malleus, differentiate between retraction pockets and adhesive process, and confirm the presence of effusion. Relying on a single test often fails to yield a definitive diagnosis. For instance, while otoscopy may show a healthy-appearing tympanic membrane and tympanometry suggests a normal middle ear, pure tone audiometry may reveal a significant air-bone gap (ABG) [7, 8]. Various tympanogram types can be found even in subjects with a normal-appearing tympanic membrane and normal hearing [9]. Consequently, clinicians typically utilize a combination of tests to achieve an accurate diagnosis. Since the early 1980s, wideband ear canal recordings have been used. Wideband acoustic immittance (WAI) assesses middle ear sound conduction across a wide range of frequencies [10]. Clinicians can detect subtle changes in middle ear acoustics and mechanical properties that conventional tympanometry cannot be proved by conventional tympanometry [11]. Studies have shown that WAI has improved accuracy over single-frequency tympanometry and enhances differential diagnosis, particularly in older children and adults with conductive hearing loss [12], otosclerosis [13], and otitis media with effusion [14].
In 2013, participants in the Eriksholm Workshop on Wideband Absorbance Measures discussed terminology, research needs, and clinical applications of WAI. They advocated using the term WAI, encompassing power-based and impedance-based measures, to describe measures of impedance and admittance [15].
Since then, numerous studies have reported wideband energy reflectance (WBR) or IRI2 [7, 9, 16, 17], wideband absorbance (A) [12, 18] and transmittance [12] in patients with conductive hearing loss. The challenge in interpreting and comparing these studies lies in the different measures. WBR is the ratio of reflected energy to incident energy, representing the energy reflected from the outer/ middle ear. Wideband absorbance is the power absorbed by the outer/middle ear under ambient conditions, calculated as 1-IRI2 [16].
This study compares wideband reflectance measures of adult patients with isolated chronic tube ventilation problems to those obtained through conventional single-frequency (226 Hz) tympanometry. The measurement system used for measurements applies a 100 to 3000 Hz signal. Previous research indicated that the resonance frequency in patients with tympanic membrane retraction or hyperectasis and adhesive processes was lower than in normal ears [9]. However, resonance frequency and peak measures changed following the pressurization of the middle ear via the Valsalva maneuver
This study aims to re-evaluate the test results in patients with chronic tube ventilation disorders using pressure-less acoustic immittance (PLAI), considering tympanometry, pure tone audiometry, and otoscopy.
Material and Methods
Ethical Considerations
The study design was approved by the Ethics Committee of the General Medical Council of Mecklenburg-West Pomerania (A2024- 0183). This prospective study strictly adhered to the revised version of the Helsinki Declaration. The study is registered with the German Register of Clinical Studies (DRKS DRKS00035288).
Participants
Inclusion criteria for participation included patients aged 18-90 years with middle ear diseases affecting one or both ears. Exclusion criteria encompassed patients younger than 18, those with cochlea or middle ear implants, glomus tumors, and cognitive disorders.
A total of 135 subjects from two Departments of Otorhinolaryngology, with a mean age of 53.3 ± 17.6 years (79 men and 56 women), were included. This group included 99 patients (45 unilateral and 54 bilateral) with middle ear disorders and healthy subjects with normal bilateral ears (N=36).
Subjects with no history of inflammation or disease affecting the middle ear, recent hearing disabilities, aural symptoms, and normal tympanic membranes (without atrophy, scarring, retraction, or perforation) were defined as normal.
Of the 135 patients (270 ears), 36 subjects had bilateral normal ears (72 normal ears), while 99 patients had either unilateral (45 patients, 45 ears with pathologies and 45 normal ears) or bilateral pathologies (54 patients, 108 ears with disease). In total, 117 normal ears and 153 pathological ears were considered.
All 117 normal ears from 81 subjects/patients and 37 patients out of 153 with chronic tube ventilation disorders were considered for further analysis (20 patients with epitympanic retraction, 10 patients with mesotympanic retraction without adhesion, 5 patients with adhesive process, and 2 patients with hyperectasis).
All subjects were informed about the study’s aims and provided written consent.
Procedure
Participants, both patients and healthy subjects, underwent a comprehensive medical evaluation, including ear, nose, and throat examinations. Video otoscopy was performed on all participants, and images and videos were stored. Two ENT surgeons analyzed the data and categorized each ear based on the outer ear canal and tympanic membrane condition. In all healthy subjects, acute or chronic otitis and other pathologies were excluded.
All participants underwent pure tone audiometry, pressure-less measurements of acoustic immittance using MedWave® (Neuranix, Italy), conventional tympanometry, and video endoscopy with Valsalva maneuver for patients with tube ventilation problems or retraction pockets.
PLAI
The end of the MedWave® probe was inserted into the lateral portion of the external ear canal. The test system applies a 100 to 3000 Hz signal. Evaluation of the responses results in a calculation of the complex acoustic admittance. MedWave® provides objective numerical terms: Fr (Hz)—the frequency at which the maximum value of the admittance curve occurs, and P (Peak Admittance Value).
Conventional tympanometry
Tympanometry was performed with Madsen® Zodiac (type 1096) (Otometrics) at 226 Hz from -400 to +200 daPa. The following results were used for calculation: Tympanometric peak pressure (TPP), equivalent ear canal pressure (ECP), equivalent ear canal volume (ECV), and static peak admittance (SA), along with the type of tympanogram (Jerger types: A (peak within normal limits for both pressure and height: a normal admittance/compliance reading of 0.3-1.6 mL, a normal middle ear pressure reading of +50 to -50 daPa, and a normal ear canal volume reading of 0.5 to 2.5 mL), Ad (peak between +100 and -100 daPa, A compliance reading under 0.3 mL, ECV of up to 1.6 mL), As (peak between +100 and -100 daPa, A compliance reading over 1.5 mL, ECV of up to 0.4 mL), B (flat with no significant peak), and C (the height of the peak is or is not within normal limits and is more negative than normal).
Statistical Analyses
To measure the stability and precision of PLAI and conventional measurements, Cronbach’s reliability statistic was performed. Statistical tests (Kolmogorov test and Shapiro-Wilks test) indicated non-normal distribution for all parameters, with all p values < .05. Nonparametric tests were conducted for group comparisons as appropriate. Pearson statistics were used for correlational analyses.
The alpha level was set to 0.05. SPSS version 30.0 (SPSS Inc., Chicago, IL, USA) was utilized for statistical analyses.
Results
Overall, 117 ears (36 healthy subjects with bilateral normal ears (N=72) and the contralateral ear of 45 patients with unilateral ear pathology) were classified as normal based on otoscopy and pure tone audiometry.
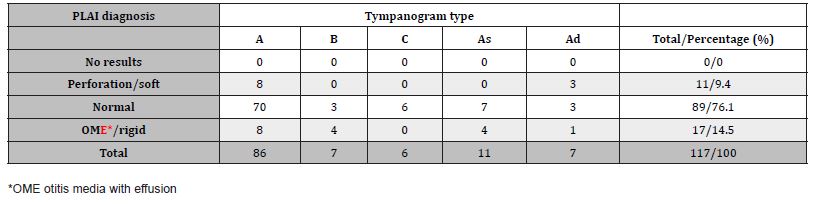
Of these, 86 out of 117 ears had a tympanogram type A (73.5%), 7 ears (6%) had a tympanogram type As, while 11 ears (9.4%) exhibited a tympanogram type Ad (Table 1). Tympanogram types B and C were found in approximately 5% of the normal-appearing ears assessed through otoscopy.
For all 117 normal-appearing ears assessed via otoscopy, an average resonance frequency of 408 Hz ± 60.97 Hz (ranging from 258.4 to 705.2 Hz) and an average peak of 1.68*10-2 mmho ranging from .52 to 2.52*10-2 mmho was determined. Table 1 presents PLAI measurements based on tympanogram type (see Figure 1 and 2).
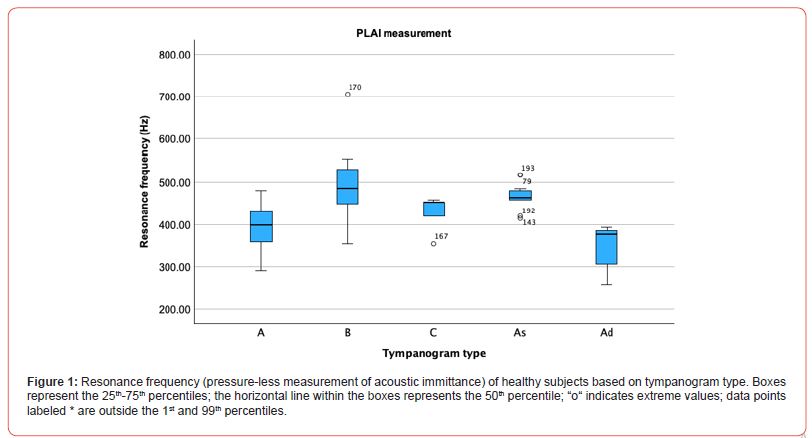
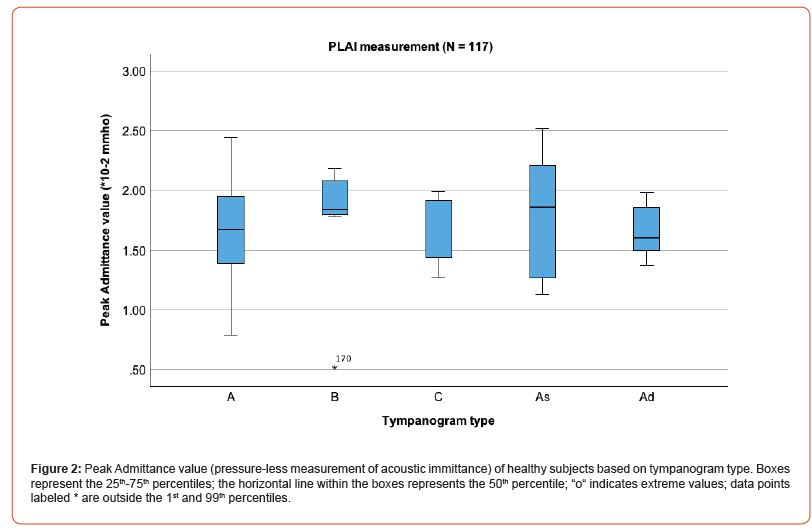
Table 1: Descriptive statistics of PLAI measurements for all 135 healthy subjects (117 ears) depending on the tympanogram type.
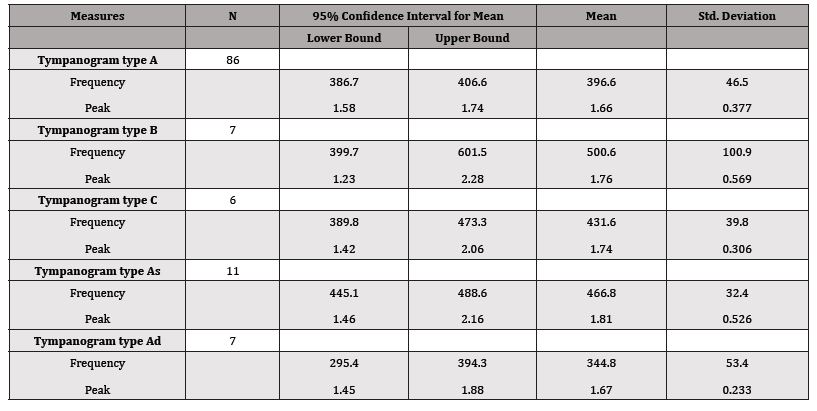
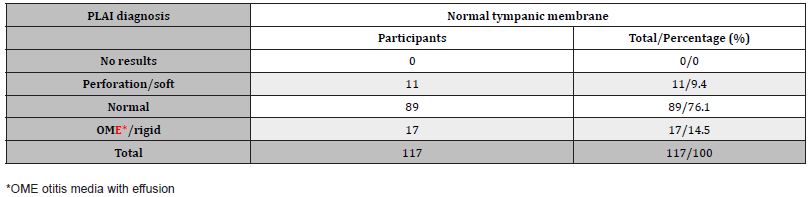
Overall, 76% of all normal-appearing ears exhibited a PLAI diagnosis of “normal” (Table 2), and less than 15% were diagnosed as “soft/perforation” or “rigid, OME”.
Table 2: PLAI diagnosis in participants with a normal tympanic membrane with otoscopy and normal pure tone audiometry (N = 117).
Considering tympanometry, 70 out of 117 subjects with a normal-appearing tympanic membrane had a tympanogram type A and a PLAI diagnosis of “normal” (60%) (Table 3).
Table 3: PLAI diagnosis in participants with a normal tympanic membrane with otoscopy and normal pure tone audiometry (N = 117), depending on the tympanogram type.
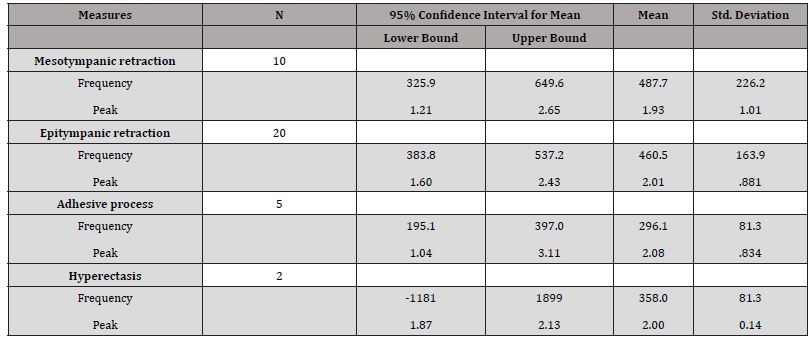
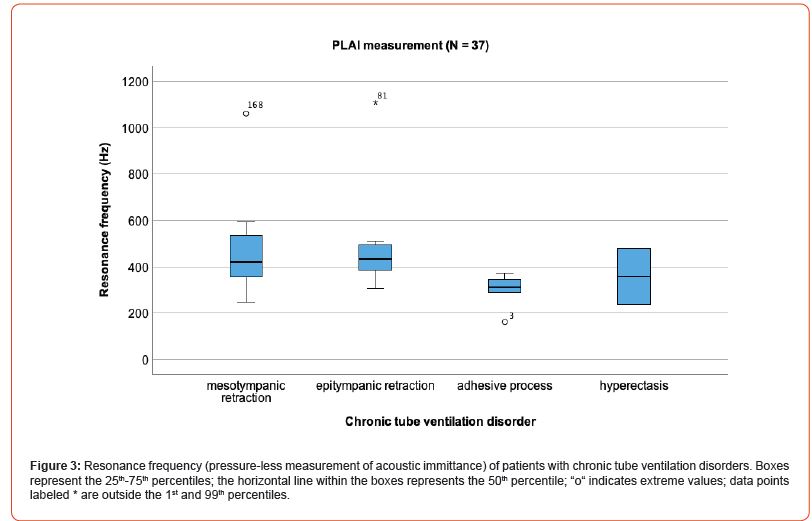
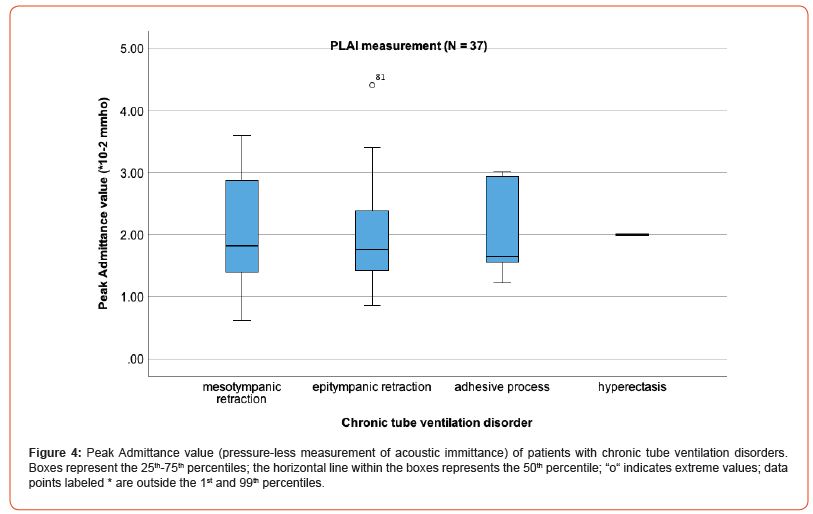
For all 37 ears with tube ventilation disorders (mesotympanic and/or epitympanic retraction, adhesive process, hyperectasis) without middle ear effusion, an average resonance frequency of 440 Hz ± 180.1 Hz ranging from 161.5-1109 Hz and an average peak of 2.00*10-2 mmho ranging from .62 to 4.41*10-2 mmho was determined. Table 4 presents PLAI measurements based on pathology (see also Figures 3 and 4).
Table 4: Descriptive statistics of PLAI measurements of 37 ears with chronic tube ventilation disorder.
Overall, approximately 50% of patients with chronic tube ventilation disorders received a PLAI diagnosis “normal” (Table 5) and 20% diagnoses “soft/perforation” and about 30% “rigid, OME”. Of those patients with an epitympanic retraction, 30% were diagnosed with “rigid/OME,” 10% with “soft/perforation,” and 55% as “normal.” All patients with epitympanic retraction, adhesive process, and eight out of ten patients with mesotympanic retraction underwent middle ear surgery. In one patient, a cholesteatoma was detected (Figure 7). This case was, therefore, excluded from statistical analysis.
Table 5: PLAI diagnosis in tube ventilation disorders (N = 37).
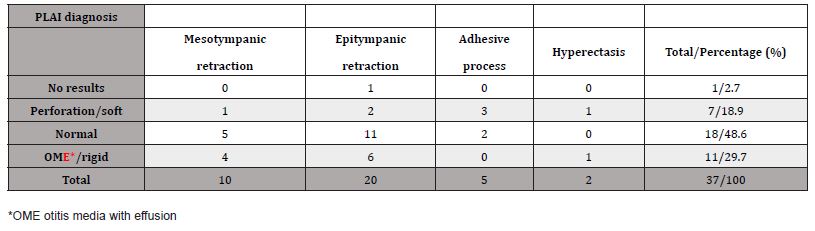
Table 6 presents PLAI diagnoses considering tympanogram type for 20 patients with isolated epitympanic retraction. The mean ABG was 15.4 ± 8.44, ranging from 3.75 to 35.0. Correlational analyses revealed no significant correlations between PLAI measures, tympanometric measures, and ABG (all p’s >.05). All six patients with epitympanic retraction diagnosed as “OME/rigid” demonstrated varying degrees of fixation of the malleus during middle ear surgery, a finding also confirmed by pneumatic otoscopy in three patients.
Table 6: PLAI diagnosis in patients with epitympanic retraction (N = 20) depending on the tympanogram type.
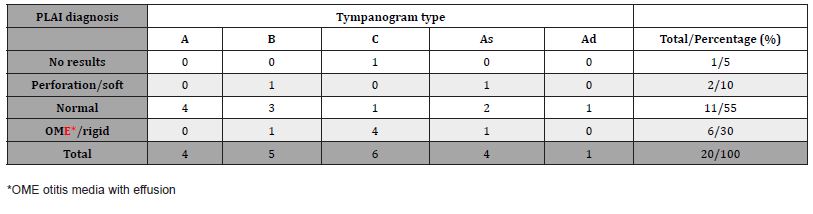
Figure 5 illustrates the findings of a patient with both epitympanic and mesotympanic retraction accompanied by mild conductive hearing loss. Tympanometric evaluation revealed an underpressure of
-261 daPa, and the tympanometer provided a tympanogram type As. PLAI demonstrated normal findings. An effusion was excluded through paracentesis. During tympanoplasty, fixation and disconnection of the ossicular chain were ruled out, and cholesteatoma was excluded.

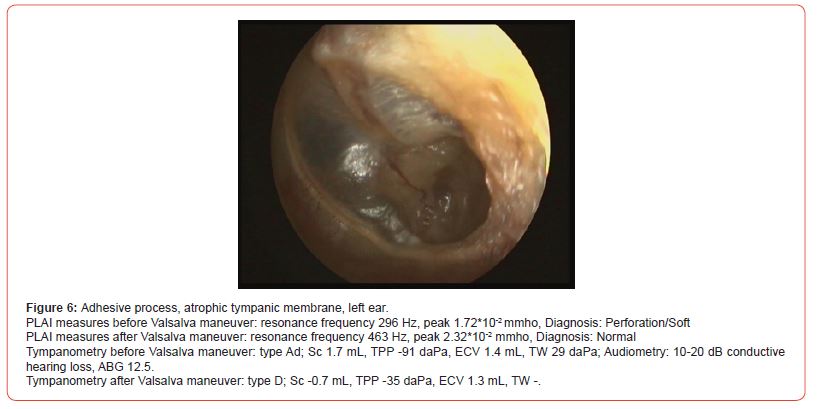
The findings of a 56-year-old man with a left-sided adhesive process are demonstrated (Figure 6). While the upper anterior and posterior portions of the tympanic membrane showed slight bulging after the Valsalva maneuver, the inferior portion of the atrophic adhesive tympanic membrane remained retracted. Both PLAI measures and tympanometric findings changed in this patient after the Valsalva maneuver. The PLAI diagnosis shifted from “perforation/soft” to “normal.” The audiometric results remained unchanged after the Valsalva maneuver.
In a 66-year-old woman with a left-sided, non-translucent, thickened tympanic membrane and a retraction pocket, mild conductive hearing loss was measured via pure tone audiometry (Figure 7). PLAI measures indicated findings resembling a fixation of the ossicular chain with increased stiffness.
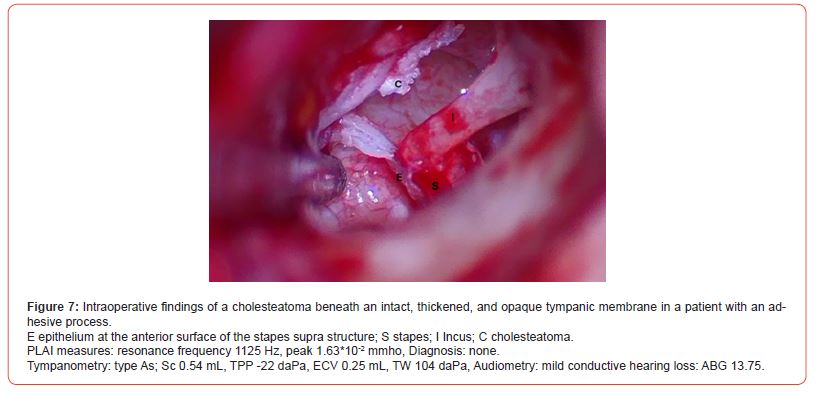
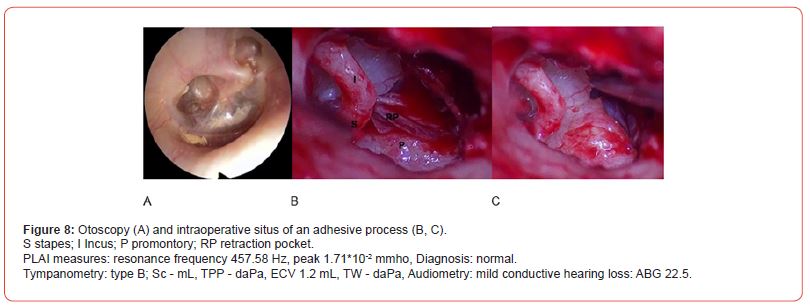
Figure 8A shows the otoscopic finding of an adhesive process. Pneumatic otoscopy revealed an attachment of the eardrum to the promontory. During surgery, adhesion of the tympanic membrane to the long process of the incus and the anterior surface of the stapes supra structure was found. The adhesive tympanic membrane was easily detached (Figure B, C). The ossicular chain was intact without fixation.
Discussion
During otological consultations, patients present with various ear conditions, including tympanic membrane perforation, otitis media with effusion, cholesteatoma, myringosclerosis, tympanosclerosis, and otosclerosis, among others. To achieve accurate diagnoses and provide treatment recommendations, a set of diagnostic tools are employed, including otoscopy and nasal endoscopy, tuning fork tests (Weber and Rinne), tympanometry, pure tone audiometry, and speech audiometry. A single method is often insufficient for a definitive diagnosis. This paper illustrates that even in patients without complaints and with normal hearing, a healthy-appearing tympanic membrane can yield diverse tympanometric findings in 26.5% of cases, with a normal tympanogram type A observed in only 73.5%.
This paper focuses on diagnosing patients with chronic tube ventilation disorders, including mesotympanic and/or epitympanic retraction, adhesive processes, or hyperectasis, using a limited set of diagnostic tests: otoscopy, tympanometry, pure tone audiometry, and WAI measurements. This project aims to assess whether PLAI offers advantages over single-frequency tympanometry in predicting ossicular fixation or disconnection of the ossicular chain. Previous studies have shown that WAI improves accuracy over singlefrequency tympanometry, enhancing differential diagnosis [12-14, 19]. WAI is a cost-effective and non-invasive technology suitable for routine evaluation in otologic settings [11]. Due to the different frequencies applied for WAI without pressurization in the literature, the term PLAI was used in this paper. The test system applies a 100 to 3000 Hz signal. Normative data presented in a previous paper indicated a resonance frequency in healthy ears of approximately 400 Hz and a peak admittance value of 1.65*10-2 mmho [9]. The results of this study demonstrate that 76% of subjects with a normal-appearing tympanic membrane provide the diagnosis “normal” with PLAI. In subjects with a normal-appearing tympanic membrane and tympanogram type A, the percentage of diagnoses “normal” increases to 81%.
Compared to healthy subjects, patients with tube ventilation disorders without middle ear effusion exhibited a higher resonance frequency and a higher admittance peak. Tympanometric measurements revealed that over 50% of patients, and even 80% in cases of epitympanic retractions, had abnormal tympanogram, primarily types As, B, and C, were found. This finding suggests a pathology that increases stiffness; however, it is not possible to specify the exact pathology. Similar findings were reported by Sanford, et al. in a case series [11]. They found that single-frequency tympanometry did not completely explain the severity of the conductive hearing loss in a patient with otosclerosis and a patient with negative middle ear pressure. With wideband admittance measurements, a narrow absorbance peak was found at 4000 Hz with significantly reduced values at frequencies lower than 3000 Hz in a child with excess middle ear pressure and OME. These findings were suggestive of abnormal increases in middle ear stiffness.
Using PLAI, diagnoses were established in patients with chronic tube ventilation disorders, ranging from “normal” to “soft/ perforation” or “rigid, OME.”
It was anticipated that an atrophic tympanic membrane with slight retraction would yield a lower admittance peak value, leading to a diagnosis of “soft/perforation” and that a severe adhesion with fixation of the ossicular chain may lead to the diagnosis of “OME/rigid.” It was demonstrated that slight retraction could lead to the PLAI diagnosis “normal” or “soft.” In cases with ossicular chain fixation in patients with epitympanic retraction, confirmed only by middle ear surgery, the diagnosis “rigid” was provided. However, slight adhesion of the tympanic membrane to the stapes supra structure and the long process of the incus did not result in increased stiffness, leading to the expected diagnosis of “rigid.” The attachment of the tympanic membrane appears to play a secondary role in explaining the ABG. Hyperectasis (bulging outward and atrophic tympanic membrane) and even 1 out of 10 slightly retracted eardrums resulted in decreased middle ear stiffness and corresponding impedance decreases. This decrease in stiffness also affects the resonance of the outer and middle ear, shifting the main absorbance peak to a lower frequency. Similar findings were presented in 2023 by AlMakadma et al. [20].
The interpretation of PLAI measures in chronic ventilation disorders is based on several test modalities, primarily otoscopy, audiometry, tympanometry, and intraoperative findings. Interpreting PLAI results without considering all the aforementioned tests may lead to misinterpretation. Despite the absence of significant correlations between PLAI measures and hearing results in all patients, in cases of epitympanic retractions, the PLAI diagnosis “rigid” seems to predict ossicular fixation. According to our results, when the PLAI diagnosis “soft” is provided, a fixation of the ossicular chain can be excluded. Preliminary results from a pilot study [9] and one case in this study (Figure 8) demonstrated that the Valsalva maneuver and pneumatic otoscopy led to transient changes in stiffness and corresponding resonance frequency. The position of the tympanic membrane (retracted, normal, or bulged) and the appearance of the outer ear canal, such as exostosis, debris, or post-inflammatory fibrosis, need also be considered when interpreting PLAI results. The small number of cases limits the significance of the results. Therefore, the results need to be proven in a more extensive study.
Conclusion
This article demonstrates the implementation of PLAI and the interpretation of PLAI measures considering otoscopy, audiometry, and singe-frequency tympanometry in patients with chronic tube ventilation disorders. The authors found that incorporating PLAI into the diagnostic battery appears to predict early-stage fixation of the ossicular chain, especially in cases with significant epitympanic retraction pockets.
Acknowledgement
None.
Conflict of Interest
No conflict of interest to disclose.
References
- Monsell EM, Harley RE (1996) Eustachian tube dysfunction. Otolaryngol Clin North Am 29(3): 437-444.
- McNicoll WD (1982) Uncomplicated eustachian tube dysfunction: the site of the nasal septal deformity. J R Nav Med Serv 68(1): 23-29.
- Yeo SG, Park DC, Eun YG, Cha CI (2007) The role of allergic rhinitis in the development of otitis media with effusion: effect on eustachian tube function. Am J Otolaryngol 28(3): 148-152.
- Goldman JL, Martinez SA, Ganzel TM (1993) Eustachian tube dysfunction and its sequelae in patients with cleft palate. South Med J 86(11): 1236-1237.
- Bluestone CD, Hebda PA, Alper CM, Sando I, Buchman CA, et al. (2005) Recent advances in otitis media. 2. Eustachian tube, middle ear, and mastoid anatomy; physiology, pathophysiology, and pathogenesis. Ann Otol Rhinol Laryngol Suppl 194: 16-30.
- Llewellyn A, Norman G, Harden M, Coatesworth A, Kimberling D, et al. (2014) Interventions for adults Eustachian tybe dysfunction: a systematic review. Health Technol Assess 18(46).
- Nakajima HH, Pisano DV, Roosli C, Hamade MA, Merchant GR, et al. (2012) Comparison of ear-canal reflectance and umbo velocity in patients with conductive hearing loss: a preliminary study. Ear Hear 33(1): 35-43.
- Sanford CA, Brockett JE (2014) Characteristics of wideband acoustic immittance in patients with middle-ear dysfunction. J Am Acad Audiol 25(5): 425-440.
- Anbari M, Zhumabaeva S, Beishenova M, Fischer D, Sulaimanov S, Just T (2024) Comparison of conventional single-frequency tympanometry with pressure-free acoustic immittance measurements of pathological and normal middle ears. On J Otolaryngol & Rhinol 7(2): 1-11.
- Stinson MR, Shaw EA, Lawton BW (1982) Estimation of acoustical energy reflectance at the eardrum from measurements of pressure distribution in the human ear canal. J Acoust Soc Am 72(3): 766-773.
- Sanford CA, Brockett JE, Aithal V, AlMakadma H (2023) Implementation of Wideband Acoustic Immittance in Clinical Practice: Relationships among Audiologic and Otologic Findings. Semin Hear 44(1): 65-83.
- Keefe DH, Simmons JL (2003) Energy transmittance predicts conductive hearing loss in older children and adults. J Acoust Soc Am 114(6 Pt1): 3217-3238.
- Feeney MP, Keefe DH, Hunter LL, Fitzpatrick DF, Putterman DB, et al. (2021) Effects of Otosclerosis on Middle Ear Function Assessed with Wideband Absorbance and Absorbed Power. Ear Hear 42(3): 547-557.
- Merchant GR, Al-Salim S, Tempero RM, Fitzpatrick D, Neely ST (2021) Improving the Differential Diagnosis of Otitis Media with Effusion Using Wideband Acoustic Immittance. Ear Hear 42(5): 1183-1194.
- Feeney MP, Hunter LL, Kei J, Lilly DJ, Margolis RH, et al. (2013) Consensus statement: Eriksholm workshop on wideband absorbance measures of the middle ear. Ear Hear 34 Suppl 1: 78S-79S.
- Prieve BA, Feeney MP, Stenfelt S, Shahnaz N (2013) Prediction of conductive hearing loss using wideband acoustic immittance. Ear Hear 34 Suppl 1: 54S-59S.
- Beers AN, Shahnaz N, Westerberg BD, Kozak FK (2010) Wideband reflectance in normal Caucasian and Chinese school-aged children and in children with otitis media with effusion. Ear Hear 31(2): 221-233.
- Keefe DH, Sanford CA, Ellison JC, Fitzpatrick DF, Gorga MP (2012) Wideband aural acoustic absorbance predicts conductive hearing loss in children. Int J Audiol 51(12): 880-891.
- Nakajima HH, Rosowski JJ, Shahnaz N, Voss SE (2013) Assessment of ear disorders using power reflectance. Ear Hear 34 Suppl 1(7 0 1): 48S-53S.
- AlMakadma H, Kei J, Yeager D, Feeney MP (2023) Fundamental Concepts for Assessment and Interpretation of Wideband Acoustic Immittance Measurements. Semin Hear 44(1): 17-28.
-
Moayad Anbari, Shirin Zhumabaeva, Munar Beishenova, Dörte Fischer, Shayirbek Sulaimanov and Tino Just*. Pressure- Less Acoustic Immittance Measurements of Patients with Persistent Ventilation Disorders. On J Otolaryngol & Rhinol. 7(3): 2025. OJOR.MS.ID.000663.
-
Audiometry, Otoscopy, Otorhinolaryngology, Ear, Nose, Ventilation issues, Nasal septal deviation, Upper airway infections, Allergic rhinitis, Cleft palate
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






