 Research Article
Research Article
Mucociliary Clearance and its Relationship to Chest CT Scores in Covid 19 Patients
Onur Buyukkoc1, Burak Celik1*, Gokhan Yalcıner1, Elif Uzun Ata1 and Mehmet Ali Babademez2
1Ankara City Hospital, Department of Otorhinolaryngology, Ankara, Turkey
2Ankara Yıldırım Beyazıt University, Department of Otorhinolaryngology, Ankara, Turkey
Burak Celik, Ankara City Hospital, Department of Otorhinolaryngology, Ankara, Turkey.
Received Date: May 01, 2023; Published Date: May 12, 2023
Summary
Introduction: In this research, we compared nasal mucosal clearance (NMC) time in COVID-19 patients and control subjects. We also investigated the correlation between NMC and chest CT disease severity scores.
Objective: We thought that patients had more frequent pulmonary involvement in cases where mucociliary clearance is reduced, that is, the duration of mucociliary clearance is prolonged.
Material And methods: The NMC results of 40 patients hospitalised for COVID-19 were compared with 40 control patients. In addition, patients’ chest CTs were scored in terms of disease severity (0-20 points). The correlation between NMC and chest CT scores were investigated.
Results: The mean NMC time was found longer in the patient group. A moderate positive correlation was found between NMC times and chest CT disease severity scores in the patient group.
Conclusion: The prolongotion of NMC in COVID- 19 patients may be due to infection and inflammation involving the nasal mucosa. Moreover, the positive correlation between NMC and chest CT scores may indicate a relationship between the severity of lung disease and tracheobronchial and nasal clearence.
Keywords: Mucociliary clearence; Chest CT disease severity score; Covid 19
Abbreviations: Severe Acute Respiratory Syndrome-Coronavirus-2: SARS-Cov-2; Nasal Mucociliary Clearance: NMC; Saccharin Transit Time: STT; Computed Tomography: CT; Ear Nose Throat
Introduction
The Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS -Cov-2) is a novel RNA beta-coronavirus of probable zoonotic origin that is currently causing an unprecedented pandemic [1]. The nose is not only the mere entry site but also the main target of SARS-Cov-2 1. The Covid 19 virus has so far been detected in the nasopharynx, oropharynx, blood, sputum and stool [2]. Classical symptoms of the infection are fever, dry cough and shortness of breath [3]. Recent reports from around the world have shown that anosmia and dygeusia are significant symptoms associated with the COVID-19 pandemic [3].
The nasal mucociliary clearance (NMC), a vital key defense mechanism, is especially important in the upper airways and sinuses, as it protects the body against noxious inhaled materials [4]. Prolonged clearance time has been observed in subjects with rhinosinusitis, deviated nasal septum, nasal poliposis, inferior turbinate hypertrophy, chronic obstructive pulmonary disease, cystic fibrosis or defects in ciliary function [5, 6]. The saccharin transit time (STT) test is a useful method for scientific research, widely used in NMC studies, as it is a reproductible, simple to perform and noninvasive technique [7].
During this COVID-19 pandemics, a research has been published reporting that NMC time is prolonged in COVID-19 patients [8]. In addition, correlation between chest computed tomography (CT) disease severity scores and laboratory parameters (neutrophil count, white blood cell count, C-reactive protein, procalcitonin and lactose dehydrogenase) in COVID-19 patients was reported in a recently published study [9].
In this study, our primary aim was to investigate the relationship between the NMC time and chest CT disease severity scores in COVID 19 patients. In addition we aimed to compare the NMC times of the COVID 19 patients and the control group.
Material and Methods
This study was carried out between September and November 2020 in the Ankara City Hospital. Covid-19 patients who were hospitalized for pneumonia or accompanying comorbid diseases were included in the study. The control group was selected from those who applied to the Ear Nose Throat (ENT) outpatient clinic due to non-covid diseases. The control group was selected from individuals of similar age and gender to the patient group. The patients requiring intensive care treatment or high flow oxygen therapy were not included in the study. Also, participants with watery rhinorrhea, sinusitis, taste, and smell disturbances that could impair mucociliary clearance were excluded from the study.
Local ethical commitee approval and written informed consents of the patients were obtained. The study approval was obtained from the ethics committee. (E2-20-98). The demographic characteristics of both the COVID 19 and the control group were recorded. NMC time was measured in both groups. Chest CT was taken for all of the COVID 19 group.
Nasal mucocilliary clearance was measured with saccharine method as described by Anderson et al. in 1974 and modified by Ruthland and Cole in 1980 [7-10]. A quarter of commercially available 60mg saccharin tablet particle, was gently placed on the medial surface of the inferior turbinate at least 7mm behind the turbinate’s anterior end to avoid the area of mucosa where cilia beat in an anterior direction. The time from particle placement until the subject reported the first sensation of a sweet taste were recorded.
Mucociliary transport times of patient and control groups were compared. Chest CT scores of all participants in the patient group were scored according to the severity scoring defined by Cheng, et al. [11] In line with this scoring system, findings of five lung lobes were assessed individually and degree of involvement was classified as none (0%), minimal (1%-25%), mild (26%-50%), moderate (51%-75%), or severe (76%-100%). Overall severity score was calculated by summation of the five lobe scores (ranging between 0-20) [11]. All chest CT scans were evaluated by the same radiologist, who is experienced in this regard. Correlation between NMC and chest CT scores were investigated.
Local ethical commitee approval and written informed consents of the patients were obtained.
Statistics
The data were analysed using the SPSS 23.0 package programme (SPSS Inc., Chicago, IL). The Shapiro- Wilk test was used to determine the normality of data distribution. Descriptive statistics are presented as mean±standard deviation for normally distributed data, and as numbers and percentages for categorical data. Student’s t-test for independent samples was used to compare the means of numeric variables. The χ2 test was used to compare the frequencies of categorical variables. Spearman’s correlation analysis was used to show the relationship between NMC time and other continuous variables. P<0.05 was considered statistically significant.
Results
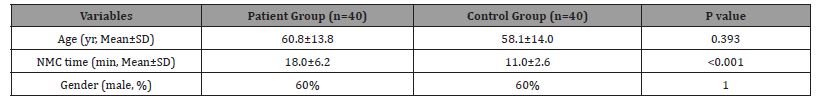
Study group consisted of 80 patients (40 COVID-19 and 40 control patients). The mean age of the patient and control groups were 60.8±13.8 and 58.1±14.0 years, respectively. Sixty percent of the participants in both groups were male. There was no statistically significant difference between the groups in terms of age and gender (p>0.05). The mean NMC time was significantly longer in the patient group (18.0±6.2 and 11.0±2.6 minutes, respectively, p<0.001) (Table 1).
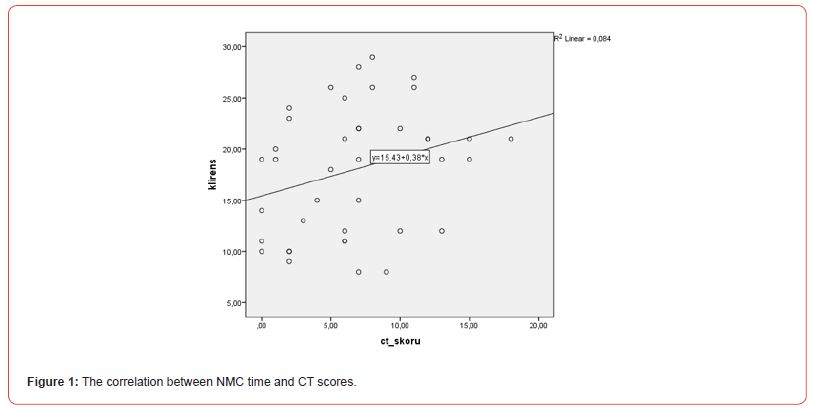
Chest tomography disease severity scores of the patients varied between 0 and 18 (mean 6.65±4.6). A moderate positive correlation was found between NMC times and chest CT scores in the patient group (r:0,314, p:0,049)(Figure 1). However, there was no significant correlation between age and NMT time in both groups (patient group: r=-0,023, p=0.889, control group: r=0,093, p=0.567).
Smoking rates were similar in both groups and it was not statistically significant between the two groups (p>0.05).
Table 1:comparison of patient and control groups.
Discussion
NMC is an important defence mechanism of the upper and lower airways, helps the expulsion of harmful substances from the respiratory tract [12]. Since NMC is fundamental in lung defense, several methods have been described to evaluate it. STT is one of the most commonly used methods due to its price, easy applicability, non-invasiveness and reproducibility. The factors that can interfere with the results obtained by the STT test are worth highlighting: age, temperature, circadian cycle, infections, drugs, caffeine, alcohol, smoking and physical activity. A normal NMC time is defined as less than 20 minutes. Thirty minutes is considered as the cut-off point that discriminates normal subjects from subjects with impaired NMC [3, 4]. Although these cut-off points are widely accepted, values between 4 and 54min are also reported. Because of these variable values, each study uses its own control group. Although the classical symptoms of infection are fever, dry cough, and the shortness of breath, rhinnorhea, nasal congestion, anosmia and dysguesia are among the significant symptoms that can be observed [3]. Moreover, according to Zou, et al. [13] higher viral loads are detected in the nasal cavity than in the oral cavity. Prolongation of NMC in COVID-19 patients may be related to infection and inflammation involving the nasal mucosa.
In addition, Millar AB [14] reported that there is a close correlation between tracheobronchial and nasal clerance in normal subjects, indicating that factors influencing tracheobronchial clerance seem to exert the same influence on nasal clerance.
As is known, mucociliary clearance may be impaired in diseases affecting the respiratory system. A recent study has shown that the NMC time due to COVID 19 disease can be extended. In our study based on this literature information and investigating the relationship between the prolongation in NMC time and CT scores, we found a moderate positive correlation between the two parameters. When we look at the literature, there is no other study examining the relationship between NMC time and CT score. However, Zhang, et al. [9] conducted a study investigating the relationship between the laboratory findings and CT scores of COVID 19 patients and found that the CT score correlated with some laboratory findings.
Koparal, et al. [8] found that NMC time was longer in covid 19 patients than in control patients. Similarly, in our study, we found the NMC time longer in the patient group. In the same study, it was observed that age and NMC time were correlated. We did not find any correlation in our study.
Our study has some limitations. The most important limitation is the limited number of people included in the study. Still, our sample size was sufficient to show the correlation between NMC time and CT scores and the difference in NMC time between the patient and control groups. Studies with more participants may show a stronger correlation between NMC time and CT scores, or the relationship between age and NMC time. In our cross-sectional study, the CT findings at the time of admission and NMC time were evaluated. In future studies, the relationship between the change in CT score and the change in NMC time can be investigated.
The strength of our study is that it is the first study in the literature that investigates the relationship between NMC time and CT score and shows this relationship. In the light of this information, we suggest that there is a correlation between the severity of the CT findings and tracheobroncial clearence; which is also correlated with NMC. This study will form the basis for many future studies. According to the results of new studies to be conducted, NMC time can give an idea about the severity of lung involvement in patients in whom CT cannot be taken.
Conclusion
In conclusion, we found that the severity of chest CT findings was correlated with the prolongation of NMC time. Moreover, the NMC time is longer in COVID 19 patients.
Limitations of the study
Prolongation of the clearance time depending on age and protection of the upper respiratory tract is a situation that can always be seen.
Acknowledgement
The research team would like to thank the other colleagues in the department. Also, deep thanks to the participants in the research and our colleagues.
Authors’ Contributions
BC, supervision, established the concept of the research, designed the work, validation, and visualization of the results. OB, GY and EUA role in supervision, role in revising the results, writing the original draft, reviewing, and editing. OK and MAB role in collecting data, applying the intervention, and analyzing the data. The authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not‑for‑profit sectors.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Local ethical commitee approval and written informed consents of the patients were obtained. The study approval was obtained from the ethics committee. (Ethics Committee of the Ankara Bilektn City Hospital, E2-20-98)
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- Gallo O, Locatello LG, Mazzoni A, Novelli L, Annunziato F (2021) The central role of the nasal microenvironment in the transmission, modulation, and clinical progression of SARS-CoV-2 infection. Mucosal Immunol 14(2): 305-316.
- Islamoglu Y, Bercin S, Aydogan S, Sener A, Tanriverdi F (2021) Assessment of SARS-CoV-2 in the Cerumen of COVID-19-Positive Patients. Ear Nose Throat J 100(2_suppl): 155S-157S.
- Grag K, Kumar Shubhanshu (2022) Effect of Covid-19 in Otorhinolaryngology Practice: A Review. Indian J Otolaryngol Head Neck Surg 74(Suppl 2), 2699-2702.
- Deborah S, Prathibha KM (2014) Measurement of Nasal Mucociliary Clearance. Clin Res Pulmonol 2(2): 1019.
- Baby MK, Muthu PK, Johnson P, Kannan S (2014) Effect of cigarette smoking on nasal mucociliary clearance: A comparative analysis using saccharin test. Lung India 31(1): 39-42.
- Aroor R, Sunu Ali Z, Gangadhara Somayaji KS (2017) Do Nasal Surgeries Affect Mucociliary Clearance?. Indian J Otolaryngol Head Neck Surg 69(1): 24-28.
- Rodrigues F, Freire AP, Uzeloto J, Xavier R, Ito J, et al. (2019) Particularities and Clinical Applicability of Saccharin Transit Time Test. Int Arch Otorhinolaryngol 23(2): 229-240.
- Koparal M, Kurt E, Altuntas EE, Dogan F (2021) Assessment of mucociliary clearance as an indicator of nasal function in patients with COVID-19: a cross-sectional study. Eur Arch Otorhinolaryngol 278(6): 1863-1868.
- Zhang B, Zhang J, Chen H, Chen L, Chen Q, et al. (2020) Novel coronavirus disease 2019 (COVID-19): relationship between chest CT scores and laboratory parameters. Eur J Nucl Med Mol Imaging 47(9): 2083-2089.
- Rutland J, Cole PJ (1981) Nasal mucociliary clearance and ciliary beat frequency in cystic fibrosis compared with sinusitis and bronchiectasis. Thorax 36(9): 654-658.
- Chung M, Bernheim A, Mei X, Zhang N, Huang M, et al. (2020) CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology 295(1): 202-207.
- Dülger S, Akdeniz Ö, Solmaz F, Şengören Dikiş Ö, Yildiz T (2018) Evaluation of nasal mucociliary clearance using saccharin test in smokers: A prospective study. Clin Respir J 12(4): 1706-1710.
- Zou L, Ruan F, Huang M, Liang L, Huang H, et al. (2020) SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. N Engl J Med 382(12): 1177-1179.
- Millar AB, Agnew JE, Newman SP, Lopez Vidriero MT, Pavia D, et al. (1986) Comparison of nasal and tracheobronchial clearance by similar techniques in normal subjects. Thorax 41(10): 783-786.
-
Onur Buyukkoc, Burak Celik*, Gokhan Yalcıner, Elif Uzun Ata and Mehmet Ali Babademez. Mucociliary Clearance and its Relationship to Chest CT Scores in Covid 19 Patients. On J Otolaryngol & Rhinol. 6(3): 2023. OJOR.MS.ID.000637.
-
Nasal mucosal clearance, Pulmonary involvement, Ear Nose Throat, Breath, Dry cough, Nasal septum, Rhinosinusitis, Sinusitis, Taste, Smell.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






