 Research Article
Research Article
Management of Facial Palsy Secondary to Temporal Bone Fracture
Najib Zouhair*, Anass Chaouki, Youssef Oukessou, Sami Rouadi, Redalah Elarabi Abada, Mohamed Roubal and Mohamed Mahtar
Department of Otorhinolaryngology, Hospital of 20 august, Casablanca, Morocco
Najib Zouhair, Department of Otorhinolaryngology, Hospital of 20 august, Casablanca, Morocco
Received Date: February 07, 2020; Published Date: February 24, 2020
Abstract
Aim: The aim of this study was the analysis of clinical and paraclinical facial palsies occurring after fracture of the temporal bone so as therapeutic indications and outcomes.
Methods: We conducted a prospective and Evaluative study during three years in the department of ENT of the hospital of 20 august. Including all patients presented to the emergency unit with temporal bone Trauma with facial paralysis.
Results: 24 patients including 21% grade III, 21% grade IV, 14% grade V, 34% grade VI, most often secondary to fracture of the right temporal bone with 56% and in 7% of cases it is bilateral. The electromyogram showed 7% of cases it is a moderate axonotmesis, 25% of cases moderate to severe axonotmesis, 34% neurotmesis. The Schirmer test noted hyposecretion in 53%. We performed 13 cases of surgical decompression of the three portions of the facial by the retro-auricular trans-mastoidal approach and one case of hypoglossal-facial anastomosis. The follow-up was monthly. The evolution was favorable in 80% with almost normal facial and auditory functions and an average decline of 2.7 years.
Conclusion: FP grade and it’s time to installation are two crucial clinical elements in the treatment decision. Most authors agree to favor medical treatment for incomplete PF and secondary onset. Total and immediate FP, with a spontaneously adverse prognosis, classically call for surgical treatment.
Keywords: Facial palsy; Temporal bone fracture; Decompression
Introduction
FP secondary to temporal bone trauma is a complication related to a fracture through the intra-petrous facial canal that can sit in one or more of facial canal segments. It may result to a compression, stretching, inflammation or even nerve transection. It may cause a partial or total loss of facial muscles motor function which generally results in generalized hemifacial weakness and it causes major aesthetic and functional damage [1].
Materials and Methods
We conducted a prospective and Evaluative study during three years in the department of ENT of the hospital of 20 august. Including all patients presented to the emergency unit with temporal bone Trauma with facial paralysis (grades between III and VI of house and Brackmann grading system), Data collection was made through emergency registers, medical records, operative reports and follow-up in ENT consultation, variables studied was the clinical examination (Side, date of occurrence and circumstances of the PF, Degree of paralysis according to House-Brackmann’s Classification), and the paraclinical assessment( Audiometry and Impedance Audiometry, acoustic reflex, Temporal bone CT scan, Schirmer’s test, Electromyography (EMG), Electrogustometry were not performed) [2]. Medical treatment was based on prednisolone 1 to 1.5 mg/kg/15 days and progressive degression, active and passive physiotherapy without electrical stimulation, eye Care. Patients were reassessed monthly through one year and each year through 3 years.
Results
We collected 24 patients with facial palsy among the 347 patients presented for temporal bone fracture during the 3 years of study, only 14 of them were operated. The mean age of patients was 23 years, with extremes between 8 and 35 years, all patients were men. Sixty-five percent of patients had polytrauma, 28% had an isolated temporal bone trauma. Thirty-four percent of patients had grade VI, 14% had grade V and the grade IV and III was in 21 % each [3]. Facial palsy was noticed in the Right side in 56% of cases, and bilateral in 7% of cases. otologic examination found hemotympanum in 42% of patients, post traumatic perforation in 36%, cerebrospinal fluide otorrhea in 15 %. Temporal bone CT scan showed transverse extra labyrinthine fracture in 60% and mixed extra-labyrinthine fracture in 20% of all cases (Figure 1).
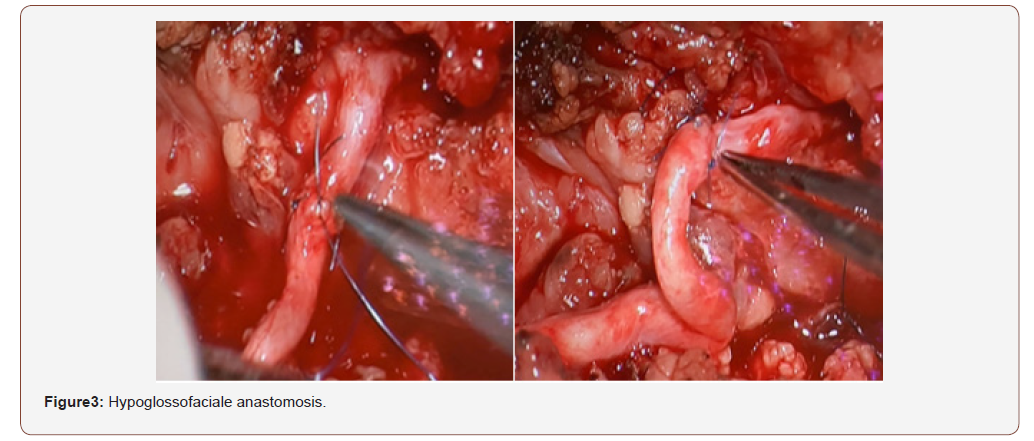
Electromyogramme found an axonotmesis in 66% and neurotmesis in 34% of cases. Schirmer test showed an altered secretion in 53% of cases. The acoustic reflex was absent in 91% of cases. The geniculate ganglion was affected in 36% of cases, the tympanal segment in 20%, the mastoidal segment in 14%, the association of first and second segment was seen in 14% of cases. Ten patients received medical treatment associated with physiotherapy and eyes care [4]. Fourteen patients were operated, we proceeded to trans-mastoid approach: after mastoidectomy with posterior and superior tympanotomy. Facial decompression was performed in 13 cases (Figure 2). Just one patient with irreparable damages who wasn’t decompressed so we proposed a hypoglosso-facial anastomosis (Figure 3). on the other hand, we found discontinuous ossicular chain in 52% and we performed a disarticulation in 36% with ossiculoplasty type 2 by incus or cartilage transposition [5]. The evolution after 3 years of surgical and medical treatment found a remarkable improvement from grades 3 and 4 to grades 1 and 2 in 70% of cases and from grades 5 and 6 to grades 3 and 4 in 15%.
Discussion
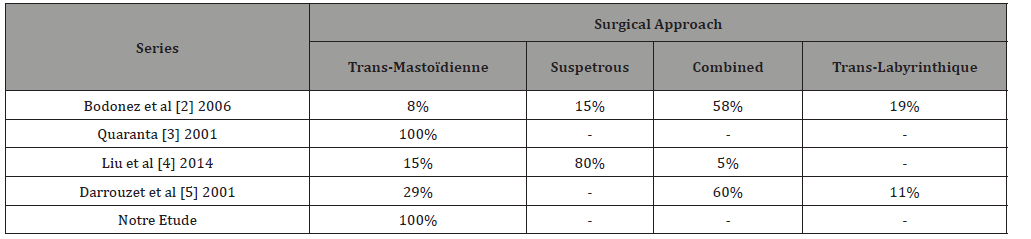
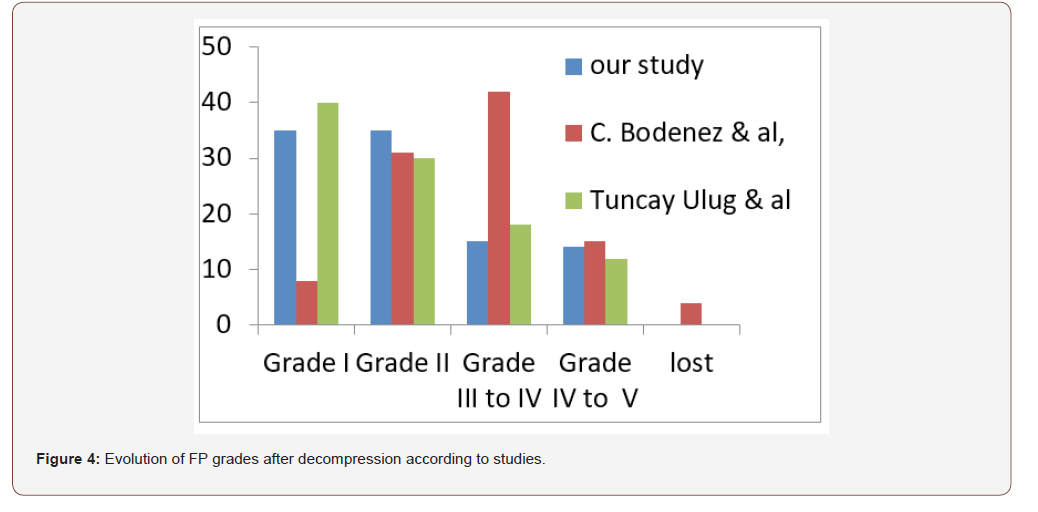
The choice of the approach is controversed, although the transmastoidal combined or not to the sus petrous approach seems to be the most used by authors (Table 1). After decompression the majority of patients facial palysis turned to grades 1 or 2 except for Badenez & al where the majority of facial palysis turned to grades 2 and 3 mostly [6-7] (Figure 4).
Table 1: Decompression approach according to authors.
Conclusion
There is no therapeutic consensus. authors decide according to, clinical presentation and electromyography results time for surgical management is also controversial. It is recommended to operate in cases of: Immediate facial paralysis Grade VI, or Grade III and above resistant to oral corticosteroids.
Its satisfying to obtain a grade I to III after decompression, and a grade III to IV after nerve repair.
Acknowledgement
None
Conflict of Interest
No conflict of interest.
References
- Labbé D, Bardot J, Bénateau H (2007) Peripheral facial paralysis surgery and sequelae EMC Tech Chir Chir. Plast Reconstr Esthét 2(4): 1-18.
- Bodenez C, Darrouzet V, Rouanet Larriviere M, Barreau X, Liguoro D, et al. (2006) Facial paralysis after fracture of the temporal bone. Ann Otolaryngol Chir Cervico-Faciale 123(1): 9-16.
- Quaranta A, Campobasso G, Piazza F, Quaranta N, Salonna I (2001) Facial nerve paralysis in temporal bone fractures: outcomes after late decompression surgery. Acta Otolaryngol (Stockh)121(5): 652-625.
- Liu Y, Han J, Zhou X, Gao K, Luan D, et al. (2014) Surgical management of facial paralysis resulting from temporal bone fractures. Acta Otolaryngol (Stockh) 134(6): 656-660.
- Darrouzet V (2001) Management of facial paralysis resulting from temporal bone fractures: Our experience in 115 cases. Otolaryngol Head Neck Surg 125(1): 77-84.
- C Bodenez, V Darrouzet, M Rouanet Larriviere, X Barreau, D Liguoro, et al. (2006) Ann Otolaryngol Chir Cervicofac 123(1): 9-16.
- Ulug T, Arif Ulubil S (2005) Management of facial paralysis in temporal bone fractures a prospective study analyzing 11 operated fractures. Am J Otolaryngol 26: 230-238.
-
Najib Z, Anass C, Youssef O, Sami R, Redalah E A. Management of Facial Palsy Secondary to Temporal Bone Fracture. On J Otolaryngol & Rhinol. 2(2): 2020. OJOR.MS.ID.000534.
-
Facial palsies, Axonotmesis, Neurotmesis, Canal segments, Bone Trauma, Mastoidal segment, Corticosteroids, Labyrinthine, Acoustic reflex, Hemotympanum.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






