 Research Article
Research Article
Interpretation of Computed Tomography of the Temporal Bone on Inverted Imaging by Otologists and Neurotologists
Mounika Naidu Boya1*, Nilesh Mahajan2, Vijayendra Honnurappa2, Vinay Kumar Vijayendra2, Miriam I Redleaf1 and Burce Ozgen3
1Department of Otolaryngology/Head and Neck Surgery, University of Illinois-Chicago, USA
2Vijaya ENT Care Centre, Superspeciality Otology Centre, Bangalore, India
3Department of Radiology, University of Illinois at Chicago, USA
Mounika Naidu Boya, Department of Otolaryngology/ Head and Neck Surgery, University of Illinois-Chicago, 1855 W. Taylor St. Suite 2.42, Chicago, IL 60612, USA.
Received Date: November 06, 2024; Published Date: November 20, 2024
Abstract
Objective: Radiologists use inverted image high resolution computed tomography (HRCT). Do inverted images help otologists and neurotologists identify temporal bone structures?
Methods: Two surveys compared identifying otosclerosis and the neural canals in regular versus inverted images. Survey 1 selected 7 regular/ inverted pairs of HRCT axial images from patients with successful stapedectomies. Seven regular/inverted pairs from non-pathologic HRCT temporal bones were normal counterparts to the otosclerosis bones. Thirty-five respondents reviewed these 28 images. Survey 2 selected 9 regular/ inverted pairs of non-pathological HRCT sections. Fourteen respondents identified the neural canals from the total of 18 images. Criterion-based scoring focused on those respondents with accuracy more than 72%.
Results: Twenty percent of respondents could diagnose otosclerosis, and 21% could identify the neural canals, with no significant difference between regular and inverted images.
Conclusion: Image orientation did not affect interpretation accuracy in those with the knowledge base to identify temporal bone structures.
Keywords: Temporal bon; Radiology; Computed tomography; Otosclerosis; Stapedectomy
Introduction
In recent years the inverted images of plain chest films and high resolution computed tomographic scans (HRCT) have been endorsed for better visualization of some pathologies [1-6].
Controlled studies of radiologists’ readings of series of lung lesions have been documented these as easier to identify on the negative chest x-ray images [1, 2]. Some temporal bone pathology is also easier to identify on HRCT [3-6]. Specifically, Gadre and Wackym feel that cochlear-facial nerve dehiscence [3], persistent stapedial artery [4], membranous stapes footplate [5], stapedial and cochlear otosclerosis 6 and superior canal dehiscence [5] are easier to see on HRCT inverted images. Wackym’s study of cochlearfacial nerve dehiscence presented 8 patients whose pathology was confirmed at surgery [3]. And Gadre’s study of the membranous stapes footplate presented 33 ears (28 patients) confirmed at surgery [5]. It has also been reported that dark mode (light colors over dark background) on devices increases the visual acuity of users [7], which explains the increased popularity of inverted color schemes on screens.
To test our belief that the inverted CT images were easier to interpret, we developed web-based surveys to identify otosclerosis and neural canals in HRCT regular and inverted images. These two surveys were distributed among otologists and neurotologists in the United States and India. We anticipated that the temporal bone structures would be accurately identified by most respondents and that identification rates on the inverted presentation would be higher.
Materials and Methods
Ethics
After obtaining institutional review board (IRB) approval, HRCT images were obtained from a single tertiary care center in the Chicago metropolitan area.
CT Scanning parameters
The multidetector CT scanning of the temporal bones was performed in the axial pane with a 16-channel multidetector CT scanner (VCT LightSpeed 16, GE, Milwaukee, Wisconsin). The images were obtained with 0.625-mm collimation, 0.625-mm thickness, pitch of 0.531/1, 20cm FOV, 335 mAs (with automatic dose reduction software) and 120 kVp. The obtained data was reconstructed separately for each temporal bone in the axial plane by using a bone algorithm with 0.5-mm section thickness, 0.5- mm increments and a FOV of 100, with a matrix size of 512x 512. The axial data were then transferred to a separate workstation for post processing, with commercially available 3D reformatting software. Reformatted images were made in the axial (parallel to the lateral semicircular canal) with a section thickness of 0.625mm. Additional multiplanar reformatting images were not included in the evaluation.
The image evaluation and postprocessing to obtain “grayscale inverted images” were performed using a dedicated PACS (GE Centricity TM Universal Viewer v 6.0). Each “regular” axial dataset was inverted, using the PACS embedded image invert function.
Surveys’ structure
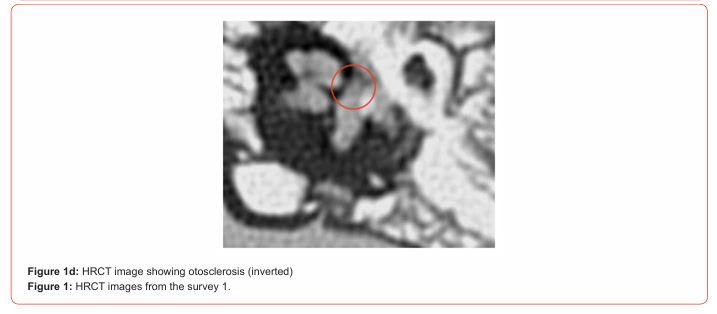
For the first survey, a pathological set of 7 regular/inverted pairs of HRCT axial images was obtained from 7 adult patients who had otosclerosis of the footplate confirmed surgically during stapedectomy. Seven control regular/inverted pairs of HRCT axial images were obtained from 7 patients who had undergone cochlear implantation with confirmation of ossicular mobility at implantation. This survey began with a short tutorial on the appearance of fissula ante fenestram otosclerosis on regular and inverted CT images. (Samples shown in Figure 1.) Thereafter, the first survey presented 28 images and 28 datapoints-asking the presence or absence of otosclerosis on each image. The regular and inverted images were presented in both surveys in random sequence.

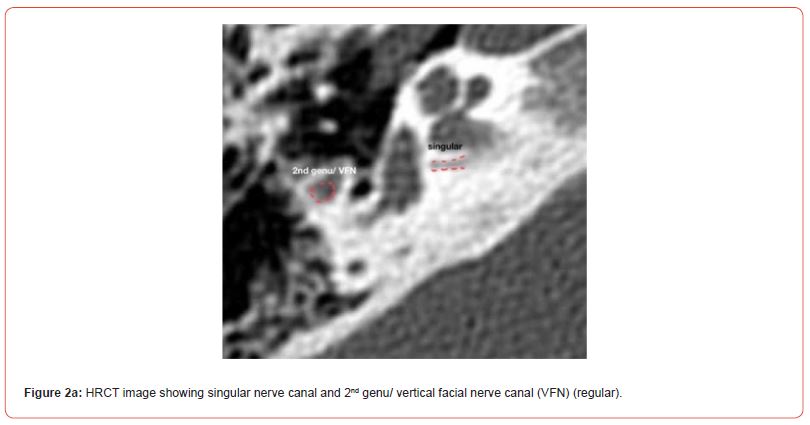
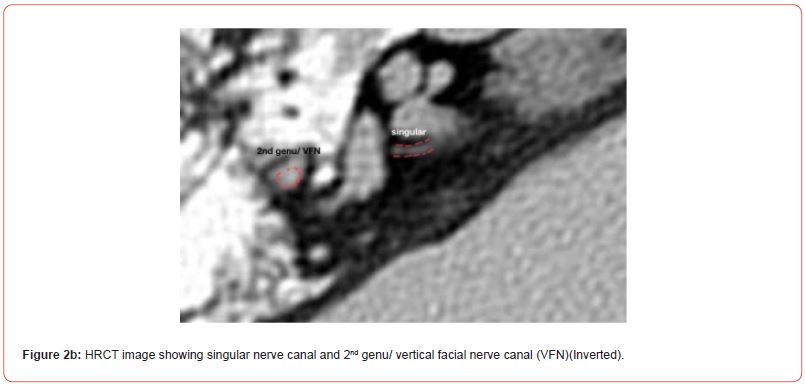
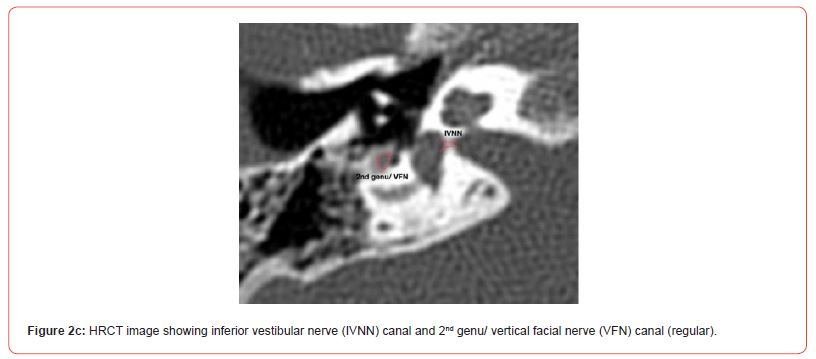
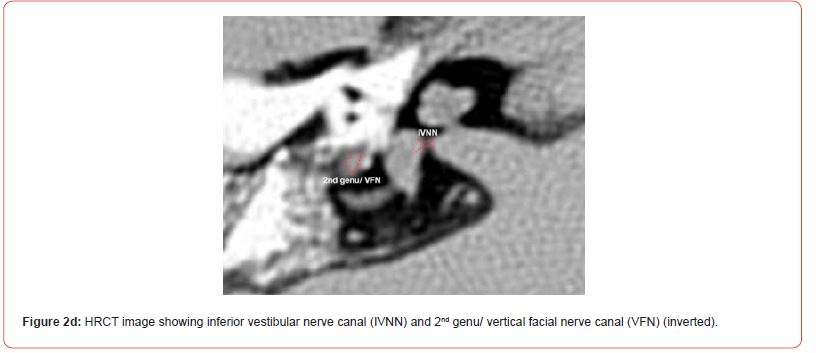
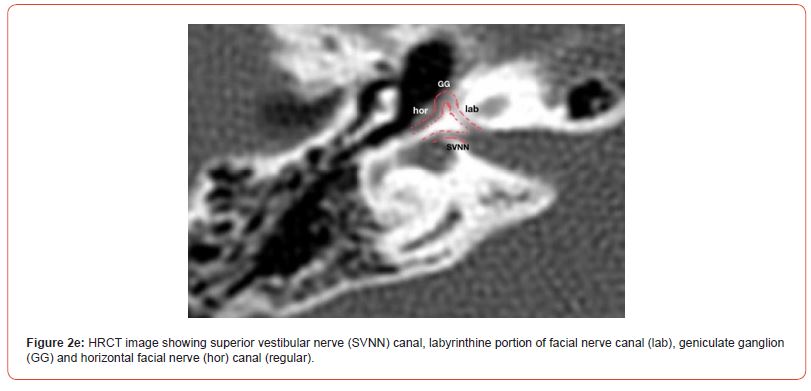
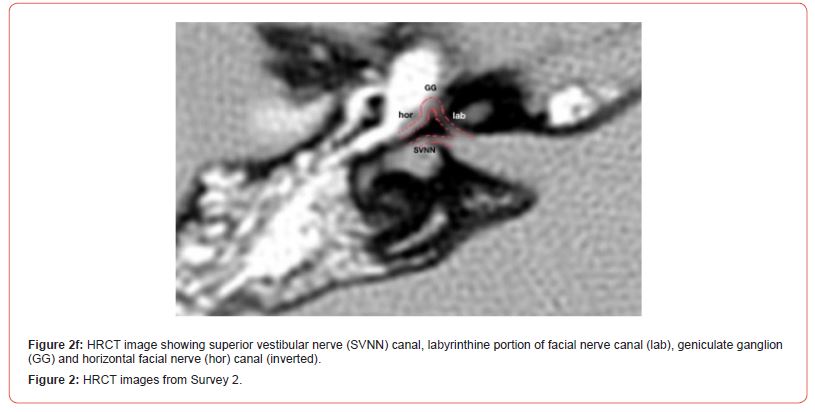
For the second survey, 9 normal regular/inverted pairs of HRCT axial images from non-pathological ears of patients were chosen which clearly showed the temporal bone neural canals with minimal ambiguity. (Samples shown in Figure 2). The second survey presented 18 images and 52 datapoints. The total number of neural canals displayed in all the images combined were 26 inverted images and 26 regular images.
Respondents
All responses were anonymous. The pool of test-takers was 35 for the first survey and 14 for the second survey. These were experienced otologists, neuroradiologists, and otolaryngologists with various years of experience of dedicated head and neck imaging in both the United States and India.
Data management and analysis
To generate the survey and collect responses, the online survey software Qualtrics XM, version “December 2023” was utilized. The survey was free, web-based, easily accessible by computer or mobile device and therefore all HIPAA information was removed and Qualtrics bot detection was enabled.
We used a criterion-based scoring system, instead of a percentile-based test. This system of scoring has been used by the American Board of Radiology for board certifying examinations [8]. In a criterion-based scoring system, all respondents who show enough knowledge can pass the test; and passing is determined by whether their score meets or exceeds the set criterion [8]. This is similar to a driving-knowledge-based test where all takers who demonstrate the required knowledge level are passed, independent of percentile position.
Studies have indicated that CT scan error rates in readings by professional radiologists range from 9.8% to 45% [9]. In the context of head CT scans, there have been reports of a 16.2% discrepancy rate in readings by radiologists versus neurosurgeons [10]. The results from both surveys were tallied separately using the American Board of Radiology’s criterion-based system with a 72% correct, or a 28% error rate.
The unpaired t-test was used to evaluate the difference in identifying the target finding (otosclerosis or the neural canals) on regular versus inverted images.
Results
Three hundred thirty-four emails were sent with the otosclerosis survey link, and 56 participants started the survey while only 35 completed it. Three hundred twenty-four emails were sent with the neural canal survey link and 25 participants started the survey while only 14 completed it.
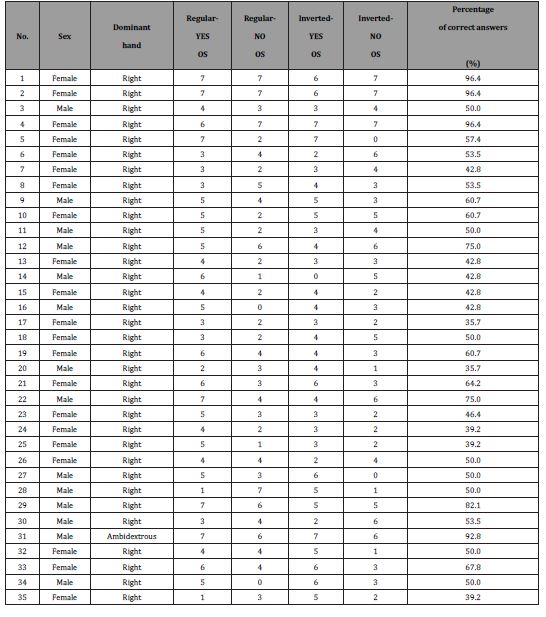
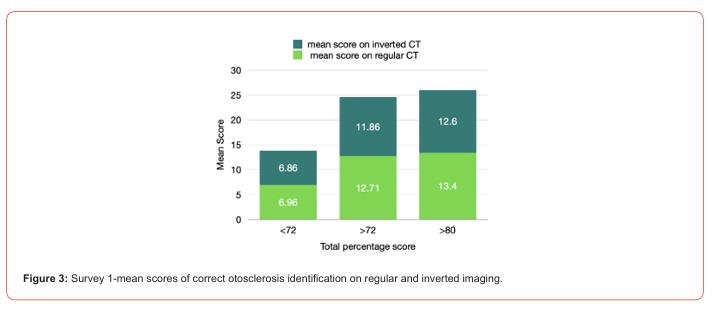
The results from Survey 1 are shown in Table 1 and Figure 3. Our study found that 7 of 35 respondents (20%) were able to accurately identify otosclerosis in more than 72% of the HCRT images. Five of 35 (14.28%) were able to identify the presence of otosclerosis in greater than 80% of the images. Among those respondents who could read otosclerosis on HRCT scans accurately, there was no significant difference in their performance when comparing inverted to regular imaging (P= 0.317). There was no genderbased differences in performance. This result suggests that among individuals who can identify otosclerosis, the orientation of the images does not influence their ability to interpret HRCT images.
Table 1:Results of otosclerosis survey.
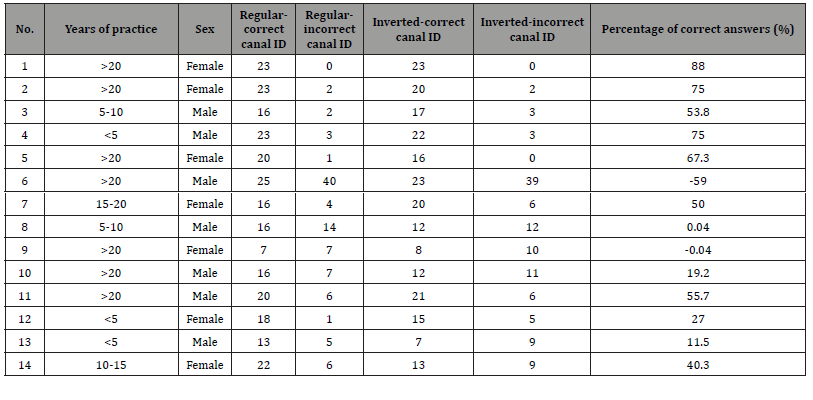
The findings of survey 2 have been presented in Table 2 and Figure 4. Our study found that only three of 14 respondents (21%) were able to accurately identify neural canals on HRCT with a score of over 72%. One of the 14 only one of the respondents (7%) was able to score >80%. Among those respondents who were able to identify the neural canals, there was no significant difference in identification when using regular or inverted images (P= 0.205). There was no gender-based differences in performance.
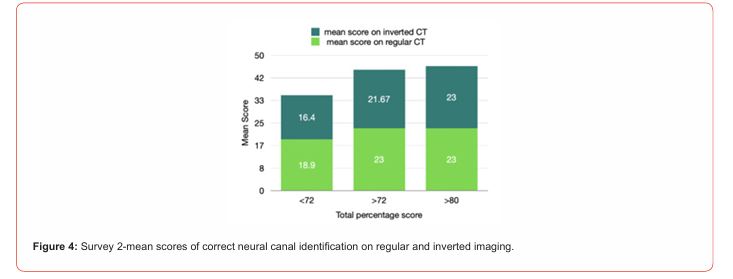
Table 2:Results of nerve canal survey. (Negative percentages indicate respondents who named more canals which were not pictured at all than canals which were pictured.)
Discussion
The present study aimed to investigate the effectiveness of inverted images in the interpretation of high resolution computed tomographic scans for the identification of otosclerosis and neural canals. The tallies from these surveys conducted among otologists and neurotologists in the United States and India revealed that approximately 20% of respondents accurately interpreted HRCT in more than 72% of images for both otosclerosis and neural canals. Only 14% were able to accurately interpret more than 80% of the otosclerosis images; and only 7% could identify more than 80% of the neural canals.
Previous studies have attributed the greater ease at appreciating HRCT structures on inverted images to visual physiology [2, 11]. The physiologic lower threshold for detecting a difference appears to be possible with the negative images [11]. Somehow the contrasts show better, as measured by 16 readers of 30 chest x-rays [2]. Otolaryngologic literature has two series of 8 and 33 patients whose surgical findings were predicted by inverted images [3, 5]. Our otologic literature mostly contains favorable impressions of the inverted images’ usefulness [4, 6]. Contrary to our own clinical impression, our study found no significant difference in the performance of respondents when comparing regular and inverted imaging for otosclerosis or neural canal identification.
Strengths of our study were the quality of our HRCT images which were selected to be clear and unambiguous. The Qualtrics system also presented the images in a randomized order and easily allowed data analysis into correct and incorrect judgments on regular and inverted images. The limitations of the study were that the actual task of interpretation proved too difficult for our respondents-of the 334 who received the first survey, only 56 responded. And of the 324 who received the second survey only 25 responded. Of the 56 who began the first survey, only 35 could complete it, while only 14 out of the 25 completed the second survey. After all that, the survey tasks were too difficult for 80% of the respondents. This meant that only 20% of respondents answered correctly on at least 72% of the images presented, which corresponds to the American Board of Radiology’s criterion-threshold for competence. Among this select group, either modality of image presentation was sufficient to identify structures. A future study might have to use tasks of less difficulty to answer this research question.
Despite our own findings here, we still endorse the adjuvant use of inverted HRCT images. It has long been clear that the anatomy and pathology of the temporal bone is best appreciated with many modalities, rather than just one. For example, HRCT alone seems to be the best modality for viewing the singular nerve [12]. For assessing the entire route and pathology of the facial nerve, however, HRCT should be combined with magnetic resonance imaging (MRI) [13-15]. Even for viewing the facial nerve intratemporal route, the HRCT must be viewed in multiple reconstructed planes to best assess each segment [14-16]. And so, just as there is no imaging modality or plane which can accommodate all situations, so the inverted images should be added to the otologists’ repertoire [3-6].
Acknowledgement
None.
Conflict of Interest
The authors have no funding and no conflicts of interest to disclose.
References
- Lungren MP, Samei E, Barnhart H, McAdams HP, Leder RA, et al. (2012) Gray-scale inversion radiographic display for the detection of pulmonary nodules on chest radiographs. Clin Imaging 36: 515-521.
- Robinson JW, Ryan JT, McEntee MF, Lewis SJ, Evanoff MG, et al. (2013) Grey-scale inversion improves detection of lung nodules. Br J Radiol 86: 27961545.
- Wackym PA, Balaban CD, Zhang P, Siker DA, Hundal JS (2019) Third window syndrome: surgical management of cochlea-facial nerve dehiscence. Front Neurol 10: 1281.
- Lindemann TL, Austin KL, Gadre AK (2020) Successful cochlear implantation in the face of persistent stapedial artery: surgical technique and imaging features. J Int Adv Otol 16: 463-466.
- Gadre AK, Edwards IR, Baker VM, Roof CR (2020) Membranous or hypermobile stapes footplate: a new anatomic site resulting in third window syndrome. Front Neurol 11: 871.
- Schwartz TR, Lindemann TL, Mongelluzzo G, Wackym PA, Gadre AK (2021) Gray-scale inversion on high resolution computed tomography of the temporal bone: an observational study. Ann Otol Rhinol Laryngol 130: 1125-1131.
- Kim K, Erickson A, Lambert A, Bruder G, Welch G (2019) Effects of Dark Mode on Visual Fatigue and Acuity in Optical See-Through Head-Mounted Displays. In: Symposium on Spatial User Interaction (SUI '19). New York, NY, USA: Association for Computing Machinery 2019: 1-9.
- Exam scoring model. American Board of Radiology. Accessed April 12, 2024.
- Terreblanche O, Andronikou S, Hlabangana L, Brown T, Boshoff P (2012) Should registrars be reporting after-hours CT scans? a calculation of error rate and the influencing factors in south africa. Acta Radiologica 53: 61-68.
- Parag P, Hardcastle TC (2022) Interpretation of emergency CT scans of the head in trauma: neurosurgeon vs radiologist. World J Surg 46: 1389-1395.
- Blackwell HR (1946) Contrast thresholds of the human eye. J Opt Soc Am 36: 624-643.
- Muren C, Wadin K, Dimopoulos P (1991) Radioanatomy of the singular nerve canal. Eur Rad 1: 65-69.
- Gupta A, Mends F, Hagiwara M, Fatterpekar G, Roehm PC (2013) Imaging the facial nerve. Rad Res Prac 1-14.
- Veillon F, Ramos Taboada L, Abu Eid M, Charpiot A, Riehm S (2010) Imaging of the facial nerve. Eur J Rad 74: 341-348.
- Jäger L, Reiser M (2001) CT and MRI imaging of the normal and pathologic conditions of the facial nerve. Eur J Rad 40: 133-146.
- Tüccar E, Tekdemir I, Aslan A, Elhan A, Deda H (2000) Radiological anatomy of the intratemporal course of the facial nerve. Clin Anat 13: 83-87.
-
Mounika Naidu Boya*, Nilesh Mahajan, Vijayendra Honnurappa, Vinay Kumar Vijayendra, Miriam I Redleaf and Burce Ozgen. Interpretation of Computed Tomography of the Temporal Bone on Inverted Imaging by Otologists and Neurotologists. On J Otolaryngol & Rhinol. 7(2): 2024. OJOR.MS.ID.000657.
-
Otologists, Cochlear facial nerve, Otosclerosis, Neural canals, Head and neck, Neurotologists, Temporal bone, Stapedectomies, X-ray images
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






