 Clinical Case
Clinical Case
Glossoplasty Procedure in Treatment of Lingual Lymphatic Malformations
Smail Kharoubi*
*ENT Department, Universitary and Hospital Center CHU of ANNABA, Faculty of Medicine, University Badji Mokhtar-Annaba 23000 Algeria
Smail Kharoubi, ENT Department, Universitary and Hospital Center CHU of ANNABA, Faculty of medicine, University Badji Mokhtar- Annaba 23000 Algeria.
Received Date: June 07, 2023; Published Date: June 19, 2023
Summary
lymphatic lingual malformations (LMs) can causing many functional and cosmetic problems. Global screening is necessary (imaging RMN) before management. Many therapeutic options are possible: sclerotherapy, Laser, radiofrequency but surgical excision is the best solution specially in localized LMs or recurrent cases after non surgical therapy. We presented in this work one observation of LMs treated by surgical excision with good result.
Keywords: Lymphatic Malformations; macroglossia; Gossoplasty
Introduction
Lymphatic malformations (LMs) are developmental anomalies consisting of abnormally formed lymphatic channels and cystic spaces of varying size. Lymphatic malformations are present at birth but are not always obvious. Most become evident before 2 years of age. Lymphatic malformations of the tongue procure frequently pain, bleeding, difficulty eating, dyspnea, sleep apnea and speech difficulties. We can describe three types: micro cystic LMs, macro cystic LMs, mixed LMs. Clinical diagnosis is easy but a complete and screening is important and consists of the first stapes before treatment. Imaging (Doppler, RMN) show loco regional extension, identified pathologic presentation (macro cystic or micro cystic lymphatic malformation) and facilitate management protocol.
Clinical Case
A 4 year old boy presented to our ENT department with very important macroglossia. the beginning of disease was noted after birth with progressive macroglossia engendered sialorrhea, difficulty in speech and perturbance social relation (Figure1). Clinical exam show important macroglossia with impossibility of mouth closing.

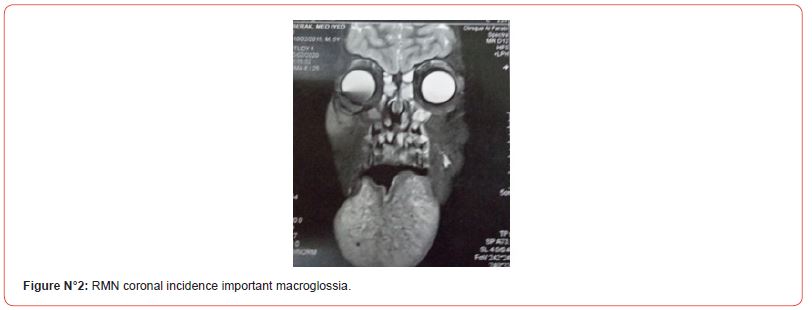
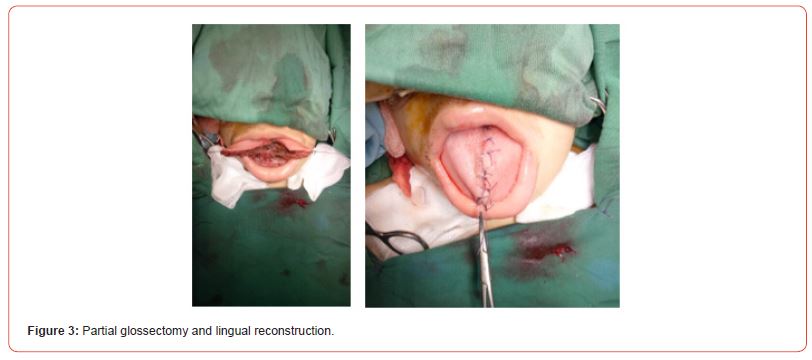
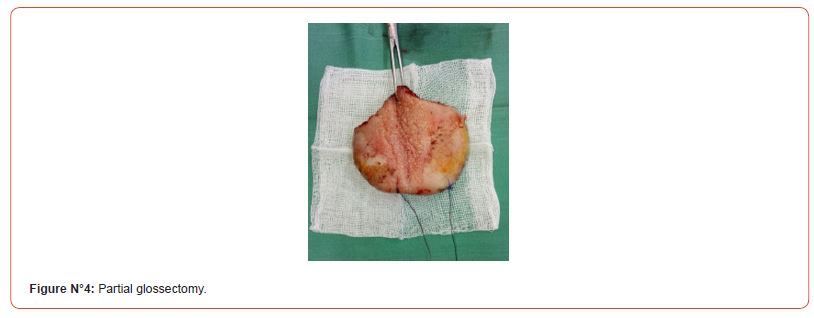
We have not find any other head and neck malformation. He had regularly corticosteroid therapy especially in acute growth. RMN note regular hypertrophy of tongue. After discussion and psychological evaluation we propose and realize a reduction glossoplasty with good final result (Figures 2,3,4).
Figures N°2-4
Discussion
Lymphatic malformation or lymphangioma is a rare benign congenital lesion of unknown aetiology. Lymphangioma was first described by Virchow in 1854. More than 90% of all lymphatic malformations occur in the head and neck, including the cheek, tongue, and floor of mouth. Wiegend has presented a classification of this disease in four stages: stage I -micro cystic lymphatic malformations of tongue, stage II with muscle involvement, stage III - tongue and floor of mouth, stage IV- tongue, floor mouth and further cervical structures [1].
The management of lymphatic malformations (LMs) continues to improve with advancement in molecular genetics, imaging, and treatment options.
Etiologies of macroglossia are numerous and separated into congenital or acquired.
Macroglossia can resulting to [2]:
-Muscular hyperplasia: Beckwith-Wiedemann syndrome, myxoedema, acromegalia, chromosomic anomalies (17p11.2 deletion,9q34 deletion).
-Infiltrative tissular lesion: lymphatic and venous malformation, hemangiomas, amylosis, neurofibromatosis, mucopolysaccharidosis.
-Infectious and Inflammatory causes (syphilis’s, tuberculosis, sarcoidosis, actinomysosis).
Others: down syndrom, micrognathia, angio edema.
A good and fine evaluation of patient status is very important.
Initially we must exam the buccal cavity and tongue description: morphology, anteroposterior and lateral diameter macroscopic aspect (congestive, fissure, angioma, edematous mucosa) and make a photo’s of lesion also a graphic model with all menstruation (length, width, thickness). We appreciate also mobility of tongue, ,teeth evaluation and possibility of dyspnea.
Imaging (RMN) is important procedure. RMN appreciates tongue morphology, vascular participation, floor of tongue, floor of mouth, others lymphangiomas (parapharyngeal, salivary gland, neck). This exam facilitate the choice of therapeutic protocol and authorize follow up. Doppler give information about vascular velocity. Biologic screening can to help us in a few cases (metabolic disturbance, enzymatic and genetic anomalies). Lingual biopsy can recognize uncommon and difficult diagnosis(sarcoidosis, amyloidosis). Before treatment we must discussed with parents of child ,giving consentment and expose all possible solutions. We must also to explain the aim of our procedure and therapeutic program.
Various treatment modalities are tried and we can describe medical or surgical approaches.
1. Corticosteroid: oral or intravenous way in acute inflammation or associated with others therapeutic options. Usually we utilize 1mg/kg/day of prednisolone during 5 to 8 days.
2. Local injection sclerotherapy: sclerotherapy is a true solution with appreciable results in lymphatic malformations management. It induce retraction, tissue fibrosis and partial or total reduction of the lesion (macro cyst). A lot of sclerosing agent is used: bleomycin, OK- 432 (picibanil), doxycyclin, pingyangmycin [3, 4]. Sclerotherapy used primary in macroscopic lymphatic malformation or secondary to recurrent cysts following partial extirpation. May propose first line treatment the injection of pingyangmycin (1mg/ml, 3-4 weeks interval with over 1 to 8 injections) in micro cystic lingual lymphatic malformation and 62,5% of total response [5].
3. Lasers: diode, carbone dioxide, yttrium-aluminum-garnet, potassium-titanyl-phosphate [6]. All variety of Lasers have been used with similar results. Laser treatment induces tissue fibrosis. Laser therapy reduced intraoperative time ,minimal bleeding and without suturing. the complications after this therapy are minor pain, edema, surinfection.
4. Electrocautery can to be help us and associated excision function and hemostasis.
5. Radiofrequency ablation [7]. Grimmer about eleven patients treated with radiofrequency related diminished bleeding, pain, infection or vesicle formation, one patient with complete resolution and 6 patients with significant improvement [6, 8].
6. Radiotherapy: The most common indication for first radiotherapy was progression despite standard therapy and/ or urgent palliation for symptoms [9]. This option is difficult and must to be last choose. Protocol used 2 Gray per week 35 to 45G. Morbidity is frequent and consist in pain, xerostomia, dysgeusia, oedema, pain swallowing.
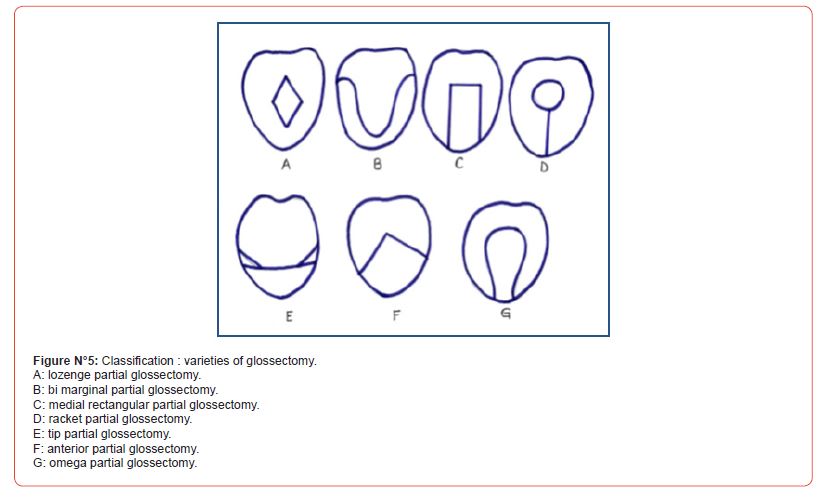
7. Surgical excision is the best solution (Glossoplasty). We realize a partial glossectomy (monopolar, radiofrequency, Laser) of the tip, marginal, anterior ou medial tongue (Figure N°5). residual tongue after resection must to be contening in month cavity with normal and functional protraction. Post operative orthophonic reeducation is necessary from good results. Glossoplasty is indicate also after failure of another treatments [3, 4].
Figure N°5
Complications and post therapeutic difficulties include infection, hematoma, seroma, neural damage and difficulty in speech. Follow up is very important time. patient is controlled 1,3,6 and 9 mouth after therapy. We evaluate results and functional disturbance by clinical and imaging evaluation. A complement of treatment can be necessary by surgery, sclerotherapy or Laser application. Lymphatic malformations lesion can regressed with time.
Conclusion
lingual lymphatic malformations is difficult situation with functional and cosmetic disturbance. Surgical approach (glossoplasty) is a very good option with favorable results in majority of cases. We waiting new development and update in biology, genetic and technological tools for future management in lymphatic malformations.
Acknowledgement
None.
Conflicts of Interest
No conflicts of interest regarding the publication of this article.
References
- Wiegand S, Eivazi B, Zimmermann AP, Neff A, Barth PJ, et al. (2009) Microcystic lymphatic malformations of the tongue: diagnosis, classification, and treatment. Arch Otolaryngol Head Neck Surg 135(10): 976-983.
- Goswami M, Singh S, Gokkulakrishnan S, Singh A (2011) Lymphangioma of the tongue. Natl J Maxillofac Surg 2(1): 86-88.
- Parashar G, Shanka Gr, Sahadev R, Santhana krishnan R (2020) Intralesional Sclerotherapy with Bleomycin in Lymphatic Malformation of Tongue an Institutional Experience and Outcomes. J Indian Assoc Pediatr Surg 25(2): 80-84.
- Yoo JC, Ahn Y, Lim YS, Hah JH, Kwon TK, et al. (2009) OK-432 sclerotherapy in head and neck lymphangiomas: long-term follow-up result. Otolaryngol Head Neck Surg 140: 120-123.
- Mai HM, Zheng JW, Zhou Q, Yang XJ, Wang YA, et al. (2013) Intralesional injection of pingyangmycin is a safe and effective treatment for microcystic lymphatic malformations in the tongue. Phlebology 28(3): 147-152.
- Berwald C, Salazard B, Casanova D, Bardot J, Magalon G (2006) Indications of lasers treatment for lymphatic malformations. Ann Chir Plast Esthet 51: 429-432.
- Bozkaya S, Uğar D, Karaca I, Ceylan A, Uslu S, et al. (2006) The treatment of lymphangioma in the buccal mucosa by radiofrequency ablation: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102(5): e28-e31.
- Grimmer JF, Mulliken JB, Burrows PE, Rahbar R (2006) Radiofrequency ablation of microcystic lymphatic malformation in the oral cavity. Arch Otolaryngol Head Neck Surg 132(11): 1251-1256.
- Liu KX, Lamba N, Marcus KJ, Sandler ES, Gold SH, et al. (2021) Long-term outcomes of pediatric and young adult patients receiving radiotherapy for nonmalignant vascular anomalies. Pediatr Blood Cancer 68(6): e28955.
-
Smail Kharoubi*. Glossoplasty Procedure in Treatment of Lingual Lymphatic Malformations. On J Otolaryngol & Rhinol. 6(3): 2023. OJOR.MS.ID.000638.
-
Glossoplasty procedure, Difficulty eating, Dyspnea, Sleep Apnea, Speech difficulties, ENT, Head and neck, Tongue, Salivary gland, Parapharyngeal
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






