 Case Report
Case Report
Extremely Rare Case Presentation of Lemierre Syndrome Caused by Klebsiella Pneumonia: Case Reports
Hanaa Al Senaidi1 and Anju Mathai2*
1Head of ENT Department, Sur hospital, Ministry of health, Sultanate of Oman
2ENT Specialist, Sur hospital, Ministry of health, Sultanate of Oman
Dr. Anju Mathai, ENT specialist, Ministry of health, Sur hospital, Oman.
Received Date: April 05, 2023; Published Date: April 14, 2023
Summary
Lemierre syndrome is a potentially fatal complication of oropharyngeal infections that is characterized by jugular vein thrombosis and septic emboli. Fusobacterium spp are the most causative organisms. Patients typically present with high grade fevers, neck pain, and pulmonary symptoms. Here we present 2 cases within a 12-month period with oropharyngeal infections who developed Lemierre syndrome due to Klebsiella pneumoniae. The incidence of Lemierre syndrome seems to be increasing and primary care physicians should be aware of this rare though serious condition. These 2 cases illustrated below shows that the presence of K. pneumoniae that can lead to Lemierre syndrome.
Keywords: Leimerre syndrome; Klebsiella pneumoniae; Oropharyngeal infections
Introduction
Lemierre syndrome, was first reported in 1890 by Courmont and Cade, although Lemierre, a French physician and professor of microbiology best described the syndrome in 1936 in a review of 20 cases. His cases were based on the following criteria:
1) Acute oropharyngeal infection or abscess,
2) Septicemia,
3) Thrombophlebitis of the internal jugular vein and
4) Secondary metastatic abscesses, most commonly to the lungs and joints.
It is seen mostly in previously well adolescents and young adults with slightly higher prevalence in males. Most cases of Lemierre syndrome present as sore throat, which is one of the most common presenting symptoms seen by primary care physicians, accounting for 1% to 10% of office visits. The current mortality rate of Lemierre syndrome is estimated to be between 5% and 10%, with significant morbidity. Before the advent of antibiotics, this syndrome was commonly encountered and often fatal. So physicians should be aware of a rare but potentially lethal complication of oropharyngeal infections: Lemierre syndrome, which is characterized by superinfection with Fusobacterium necrophorum, jugular vein thrombosis, and septic pulmonary emboli. Its incidence has been estimated at 1 per million per year.
In the last 10 years, already more than 80 cases have been published. This apparent increase may be related to the less frequent prescribing of penicillin for tonsillitis, its growing resistance to erythromycin, or other organisim like fusobacterium cant be isolated. Here are 2 cases of an oropharyngeal infection who developed Lemierre syndrome due to Klebsiella pneumonia.
Case 1
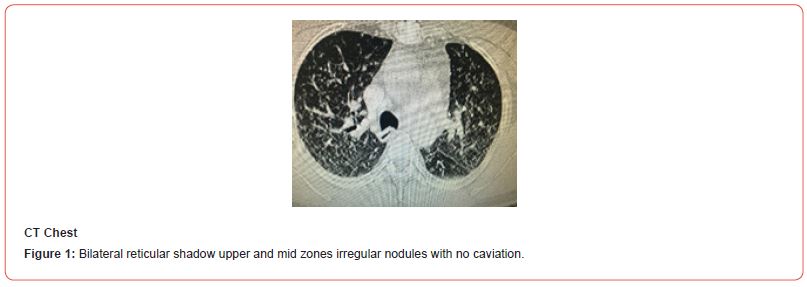
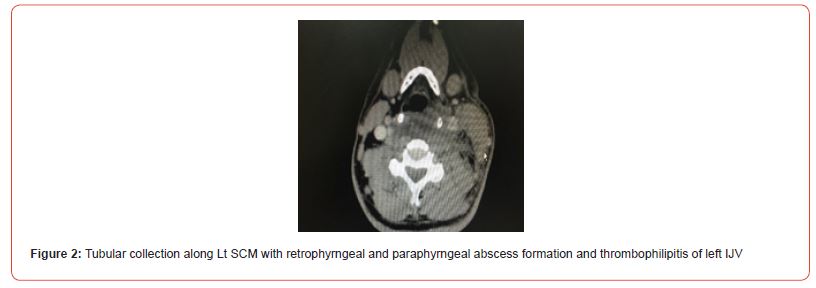
A healthy 65 years old man presented with history of sore throat, runny nose, high grade fever with chills and rigors and left neck pain and swelling which was progressively increasing in size in last 4 days. Examination in the emergency room was notable for marked left sided neck tenderness and swelling in posterior triangle lateral to sternocleidomastoid muscle, trismuss present; oral examination was normal. Chest: normal. Chest x-ray (CXR) (Figure 1) showed bilateral diffuse reticular shadows. Computed tomography (CT) scan of neck and chest (Figure 2) showed tubular collection along left sternocleidomastoid with retropharyngeal and parapharyngeal abscess formation and thrombophelibitis of the left internal jugular vein and Chest X ray showed bilateral mainly upper and mid zones irregular nodules with no cavitation and no calcification and no fibrotic changes Blood investigations at that time showed a raised white blood cell (WBC) count, marked platelets reduction, serum creatinine raised, high creactive protein of 225, Tuberculosis culture and Zeil Neilsen stain were negative. He received intravenous tazocin and underwent incision and drainage of retropharyngeal abscess transorally and transcervical approach.
Pus culture and sensitivity came as growth of klebsiella pneumonia sensitive to tazocin and ciprofloxacin. His Platelet and inflammatory marker and renal function return to normal gradually after surgery.
He was admitted with us for total 14 days in which he received 12 days Iv tazocin and 2 days of Iv ciprofloxacin and was discharged on oral ciprofloxacin for 2 weeks. Follow up period in Out patient clinic after 2 weeks, revealed normal examination of neck, no recollection and patient has clinically improved.
Case 2
62 years old man known case of Diabetes mellitus and hypertensive on medications. Presented to our setting with history of sore throat, dysphagia, odynophagia and muffled voice with submental swelling. The swelling started in left submandibular and parotid area for which he visited dentist who prescribed oral amoxyclav and offered him extraction of offending teeth after 5 days from using of oral antibiotic. With oral Amoxyclav, swelling has resolved in submandibular area with remnant in left submental and left parotid region at time of admission. Examination on emergency room revealed low blood pressure 78/41mm Hg, tachycardia, afebrile. Neck examination showed mild soft tender submental swelling with induration, Oral examination was normal apart from congested tonsils. Fibreoptic laryngoscopy was done and it was normal
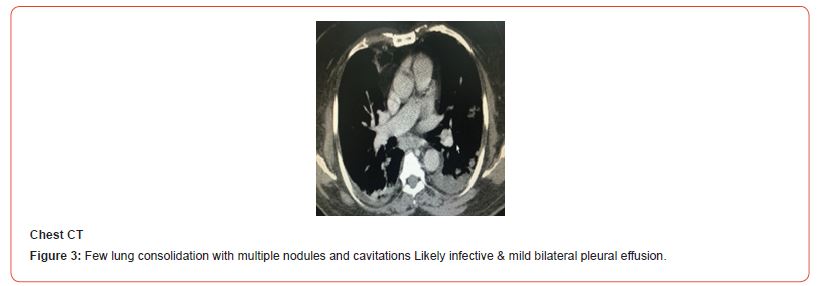
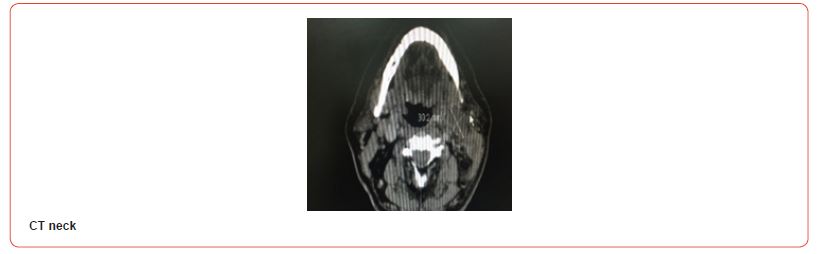
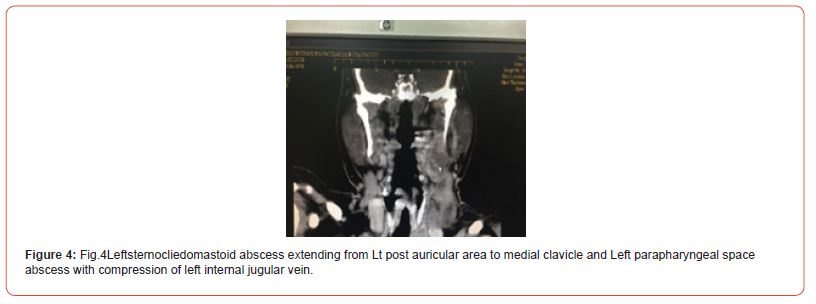
He was admitted with impression of resolving Ludwing angina. Computed tomography (CT Neck and Chest showed (Figure 3 and Figure 4): Left sternocleidomastoid abscess extending from Lt postauricular area to medial clavicle and Left parapharyngeal space abscess with compression of left internal jugular vein. Dental periapical cyst or granuloma at right upper premolar seen in CT Neck. Chest CT showed: few lung consildation with multiple nodules and cavitations likely infective and mild bilateral pleural effusion. Labs at that time showed raised white blood cell count and marked reduced in Platelet count. ESR of 118 and CRP of 378, drainage Liver enzyme with normal hepatitis and HIV screen and raised fibrinogen to 9. Then the impression was changed to left parpharyngeal abscess secondary to odontogenic infection related to remaining root tooth number 36 and grossly carious tooth number 37. He received intravenous (IV ) tazocin and underwent incision and drainage of left parpharyngeal abscess with dental extractions.
Pus, tissue and blood culture and sensitivity ( c/s ) showed growth of klebsiella pneumonia sensitive to tazocin and ciprofloxacin. His platelet and inflammatory marker and renal function return to normal gradually after drainage of abscess.
He was admitted with us for total 16 days in which he received 14 days Iv tazocin and 2days of Iv ciprofloxacin and was discharged on oral ciprofloxacin for 2 weeks. Follow up period in OPD after 2 weeks revealed normal examination of neck, no recollection and patient were clinically improve and no complain.
Discussion
F. necrophorum, the most common pathogen, has an ability to invade as a primary pathogen. This feature is related to the bacteria’s ability to produce lipopolysaccharide endotoxin, leukocidin, and haemolysin. Other organisms isolated from patients with this syndrome include Bacteroides, Streptococcus, Pepto streptococcus with more than one pathogen being reported in a few cases is the most commonly reported causative pathogen. Only four cases of Lemierre’s syndrome in patients with diabetes due to K. pneumoniae have been reported previously. A review of the literature suggested that an association exists between deep neck infections due to K. pneumonia and diabetes mellitus. The reasons for this association are still not clear.
In the current case K pneumonia was identified also in healthy patient non diabetic in both blood culture and pus culture, adding to the diversity of causative agents of Leimerre syndrome in non diabetic patients.
In the current case, the disease progressed rapidly from the first stage of primary infection. The time of onset from the initial oropharyngitis to the development of complication is usually less than 7 days which is happened in our cases. The primary source of infection in our cases was palatine tonsils and odontogenic infection which present as unspecific symptoms included fever, rigor, dyspnea , sore throat, swollen neck with pain, trismus and dysphagia, and local invasion of the lateral pharyngeal space and internal jugular vein septic thrombophlebitis via direct extension through the fascia plane between the tonsils and the parpharyngeal space by hematogenous or lymphatic space spread from peritonsillar vessels. Metastasis is the final stage of this disease
The most common site of metastatic infection is the lungs. In the current cases, pleural effusion and multiple cavitation lung lesions are present in CT chest with no symptoms. Moreover, the spleen, skin, kidneys, brain and soft tissues may be involved. In our case 2 , jaundice present, along with abdominal pain associated with mildto- moderate hyperbilirubinemia with elevated liver enzyme.
There are also hematologic complications of Lemierre syndrome, such as thrombocytopenia and disseminated intravascular coagulation. In current cases The platelet count was only 17,000IU/mL at admission in case 1 and only 50,000IU/ml at admission in case 2. Transient renal insufficiency presented in both current cases due to kidney involvement as reported in literature.
A high degree of suspicion is needed and usually the syndrome is not diagnosed until microbiology results are available. But with suspected clinical picture imaging modalities which confirm the diagnosis, microbiology result may be an additional information only. Contrast-enhanced CT provides exceptional accuracy in the diagnosis of Lemierre syndrome because of its ability to show distended veins with enhancement of the walls, intramural filling defects and swelling of adjacent soft tissues, which allows the delineation of additional pathology (e.g. abscess extension) which has been demonstrated in our cases with left side parapharyngeal abscess and compression of internal jugular vein.
Conclusion
Leimerre syndrome may be caused by organisms other than those originally described by Andre Lemierre. Our case highlights the need for clinicians to look out for organisms other than F. necrophorum in cases where index of clinical suspicion is high and also widen the antimicrobial cover. In all cases reported so far due to K. pneumoniae, the patients happen to be diabetic and it is the first time to report LS case in non diabetic with K. pneumoniae. Early recognition of the syndrome is crucial to allow the initiation of immediate appropriate therapy because microbiologic confirmation may take several days. Hence, we stress the importance of taking early blood cultures and carrying out a careful examination of the neck in suspicious patients presenting with a severe oropharyngitis. Also, contrast-enhanced CT should be performed as early as possible because physical examination of the neck and ultrasonography may be negative for thrombosis of the IJV in some cases. Accurate and prompt diagnosis followed by appropriate treatment can make the critical difference in preventing consequent morbidity and mortality [1-8].
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Kuppalli K, Livorsi D, Talati NJ, Osborn M (2012) Lemierre's syndrome due to Fusobacterium necrophorum. Lancet Infect Dis 12: 808.
- Riordan T (2007) Human infection with Fusobacterium necrophorum (Necrobacillosis), with a focus on Lemierre's syndrome. Clin Microbiol Rev 20: 622.
- Hagelskjaer Kristensen L, Prag J (2008) Lemierre's syndrome and other disseminated Fusobacterium necrophorum infections in Denmark: a prospective epidemiological and clinical survey. Eur J Clin Microbiol Infect Dis 27: 779.
- Armstrong AW, Spooner K, Sanders JW (2000) Lemierre's Syndrome. Curr Infect Dis Rep 2: 168.
- Baker CC, Petersen SR, Sheldon GF (1979) Septic phlebitis: a neglected disease. Am J Surg 138: 97.
- Brazier JS, Hall V, Yusuf E, Duerden BI (2002) Fusobacterium necrophorum infections in England and Wales 1990-2000. J Med Microbiol 51: 269.
- Hagelskjaer LH, Prag J, Malczynski J, Kristensen JH (1998) Incidence and clinical epidemiology of necrobacillosis, including Lemierre's syndrome, in Denmark 1990-1995. Eur J Clin Microbiol Infect Dis 17: 561.
- Gomide LMES, Zarate Nissel MA, Weihermann V (2022) Septic Thrombophlebitis of the Internal Jugular Vein in an Immunocompromised Patient with Lemierre Syndrome: A Case Report. Transplant Proc 54: 1388.
-
Hanaa Al Senaidi and Anju Mathai*. Extremely Rare Case Presentation of Lemierre Syndrome Caused by Klebsiella Pneumonia: Case Reports. On J Otolaryngol & Rhinol. 6(3): 2023. OJOR.MS.ID.000636.
-
Neck pain, Oropharyngeal infections, Sore throat, Tonsillitis, Runny nose, Oral ciprofloxacin, Dysphagia, Laryngoscopy, CT Neck, Left parpharyngeal.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






