 Research Article
Research Article
Evaluation of the Level of Hetero Perception of the “T” Graft for the Management of Nasal Tip in A Group of Mexican Patients
Antonio de Jesús Adame Legorreta1*, Mónica Mariana Paz Alonso1 and Julio César López-Valdés2,3
1Centro de Especialidades Agua Dulce (CEA), Department of Otolaryngology and Facial Plastic Surgery, Tampico, Tamaulipas, Mexico
2Autonomous University of Tamaulipas, Tampico School of Medicine: “Dr Alberto Romo Caballero”, Tampico, Tamaulipas, Mexico
3Río Blanco Regional Hospital, White River, Veracruz, Mexico
Antonio de Jesús Adame Legorreta, Otorhinolaryngology and facial plastic surgery, National Autonomous University of Mexico, Tampico, Tamaulipas, Mexico.
Received Date: November 29, 2022; Published Date: December 20, 2022
Abstract
Material And Method: Retrospective descriptive study of the records of patients operated on for rhinoplasty with T-graft placement. Seven independent specialists of recognized prestige in Nasal Surgery were asked to analyze the pre-surgical and post-surgical photographs at 20 weeks, and to carry out the evaluation. From each case, granting a score, the one that evaluated with the highest qualification and the one that evaluated with the lowest qualifications were eliminated.
Objective: To determine the efficacy of the “T” graft for the management of the nasal tip in mestizo patients.
Results: 22 cases were included in the analysis, 19 women and 3 men aged between 16 and 64 years. Only one case involved secondary surgery. Improvement was observed in the projection, rotation and definition of the tip in all cases, also observing improvement in the following: the wingcolumnella ratio in 86.4%, symmetry in 92.7%, obtaining a natural appearance in 92.7%, the double columnar break in 86.3% and the obtaining of luminous points in 99%. No patient had significant tip asymmetry after the surgical procedure; No patient had postoperative complications or postoperative aesthetic or functional discomfort.
Conclusion: The “T” graft can be used successfully in cases where it is necessary to increase the projection, definition and rotation of the nasal tip that cannot be achieved only by sutures or other types of grafts, it is especially useful in cases of skin thick, and being above the domes, favors a natural aesthetic result. In addition, it is a useful graft in cases of asymmetry of alar cartilages and for correction in some cases of the wingcolumnella relationship.
Keywords: Rhinoplasty; T-graft
Introduction
The nose, being the center of the face, becomes very important in aesthetic symmetry and balance. Rhinoplasty is a surgical procedure in which there are a number of techniques to achieve an ideal result in each nose; These techniques are aimed at reinforcing the structure, preserving anatomy and harmonizing the supports of the nose.
Nowadays, there is a great variety of grafts that are excellently useful in rhinoseptoplasty; They are indicated in situations in which the desired objective has not been achieved through other types of techniques. They can be used regardless of whether it is a primary or secondary procedure; this is due to the fact that they occupy, reconstruct, or allow to camouflage a loss of tissues or some anatomical defect. Likewise, they provide support to the various osteocartilaginous structures that lead to the aesthetic and functional harmonization of the nose [1, 2].
The mestizo nose commonly implies a series of challenges when it comes to obtaining a satisfactory result in rhinoplasty. The weakness of the alar cartilages and the high thickness of the skin make repositioning surgery alone insufficient to adequately define and project the tip. It is this type of nose that the banner technique was designed for [3, 4].
The changes in patients with thin, too thin skin, has the consequence that the grafts in the nasal tip are associated with presenting their visibility on the skin, so they must be used in a bevelled way and preferably camouflage them and on some occasions its use is discouraged or advised with caution [5]. The “T” graft described here, named after its design, has been widely used by the author, throughout the period from 2010 to date, in cases in which adequate projection and definition of the tip nasal, as well as the creation of new domes, cannot be achieved by using only sutures or conservative resection of cephalic strips of the alar cartilages and use of the grafts described above, in patients with thick skin; however, there is no evaluation in the literature of the aesthetic results with the use of this type of graft for the management of the nasal tip. For this reason, this paper aimed to determine the efficacy of the “T” graft to obtain an adequate projection, definition and rotation of the nasal tip, regardless of the use or not of other techniques for the management of the back or the nasal pyramid.
Patients and Methods
A descriptive retrospective study was carried out where the files of patients operated on for rhinoplasty were reviewed at the “Agua Dulce Specialties Clinic” between May 2017 and May 2018, in whose surgical technique the placement of a “T” type graft is mentioned.”.
Cases that did not have a pre- and post-surgical photographic record, did not attend their check-up appointments or did not take post-surgical photographs at 20 weeks, including frontal, basal, lateral and oblique views, as well as those associated with severe malformations were excluded., or a history of recent facial trauma. Seven independent observers with extensive and recognized experience in rhinology were asked to review the pre- and postsurgical photographs, taken 20 weeks after the procedure, and were asked to rate the following variables:
1) Obtaining the double luminous point
2) Tip projection
3) Rotation of the tip
4) Definition of the tip
5) Symmetry of the tip
6) Obtaining the double columnar break
7) Correction (or preservation, if applicable) of the wingcolumnella relationship
8) Natural appearance of the tip
Each variable was assigned a value, according to the scale shown in Table 1.
Table 1:Scale of values.
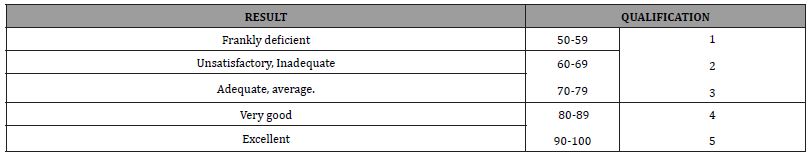
The average of the values assigned to each variable was calculated, as well as the total score obtained in each case. The improvement obtained with the placement of the graft in “T” was determined for each variable evaluated, as well as in the overall aesthetic result, likewise the observer who qualified the highest and the one who qualified the lowest was eliminated, obtaining the result of only 5 observers.
Informed consents and acceptance to participate in the study were signed.
Surgical technique
An endonasal approach is used somewhat similar to the classic “delivery”:
Marginal incisions following the caudal edge of the lateral cross of the alar cartilage, bilateral columellar incision 2mm behind the free edge of the median cruras, intercartilaginous incisions, and complete transfixion incision.
The marginal incisions are joined with the columnellars and the intercartilaginous ones with the complete transfixion, it is completely dissected to freely and easily expose all the alar cartilages, from the feet of the crura to the lateral withers.
Septoplasty is performed and the need to trim the anterocaudal edge in various ways is assessed, either triangular with an upper base if rotation is sought, or triangular with a lower base if derotation is sought, or uniform rectangular if one wishes to shorten the nose or treat the columella. protrusive (illustration), the strut graft is taken by resection of a lower strip and the “T” graft with a forceps that takes the graft from the highest and posterior part of the quadrangular cartilage just before the perpendicular plate of the ethmoid, leaving a broad framework of intact cartilage and closed with mucosa-septum-mucosa transfiction sutures with simple 4-0 catgut.
The alar cartilages are reviewed, assessing the need to remove cephalic strips in the paradomal region, always respecting at least 5mm in width, subdomal reins are placed to fully expose the alar cartilages independent of the pyramid and nasal septum on the left side (Photography).
The space between the medial cruras is dissected up to the maxilla and a strong strut 20 to 25mm long by 3mm wide (photograph) is placed. Subsequently, the placement of interdomal and transdomal stitches is assessed unilaterally or bilaterally.
A 5-0 nylon suture is placed over median cruras.

The graft is modeled in a “T” It is important to ensure that the quality of the cartilage graft is very good, with adequate thickness and strength, as well as to avoid injuring it during manipulation. Partial thickness cuts are then made on the lateral face, leaving a 5-6mm wide crosspiece and a 15mm central post, giving a total height of 20mm, the crosspiece is fixed with 5-0 nylon to the domes from the left side from caudal to cephalad and the graft is traversed in a “T” at the level of the “neck” (attachment point of the crosspiece to the central post) (photograph).
Return to the right side from cephalic to caudal, embracing the neck of the graft and leaving the crosspiece fully flown over the domes, gaining an additional 5-6mm of projection to what has already been gained with the strut graft and the facing of the domes, it is fixed to the middle cruras with a point that crosses them (without skin) and embraces the post in its lower part, thus fixing the graft in a way that it is difficult for it to move or lateralize, but leveling points are given if necessary on the sides of the transom towards the domes.
Management of the rest of the nose (lateral nose, hump, lower back, etc.) is independent of the use of the T-graft. Other pertinent observations are that it must always be accompanied by the use of a support strut, and in cases of nasal hump the Handling of the back should be done at the end of the lobe work, since the reduction required in the hump after the projection gained by this technique will be remarkably less, and in the cases of small humps it often only requires regularization with a rasp.
Results
Thirty records of patients in whom a “T” graft was placed were collected. Six did not have photographic control at 20 weeks and two cases were excluded due to a history of previous injuries such as deforming fractures.
Twenty-two cases were included for analysis, with an age of 28.09±13.66 (SD) years, with a range between 16 and 64 years; nineteen (86.36%) cases corresponded to female patients. In 21 cases the “T” graft was placed as part of a primary rhinoplasty and in one case the graft was placed in a revision rhinoplasty.
A score of 4.60±0.21 SD (range 3.905-4.875) points was obtained; according to the observers, improvement was reported for all cases in all parameters Table 2. The results are shown below: improvement in projection 97.2% and definition of the tip 97.2%, better rotation 90%, wing-columnella ratio (86.4%); improvement in double columnar break 86.4%, bright spots present in 99% of patients, improvement in symmetry 92.7% and natural appearance 95.4%.
Table 2:Evaluations obtained for each of the cases presented according to the experts consulted.
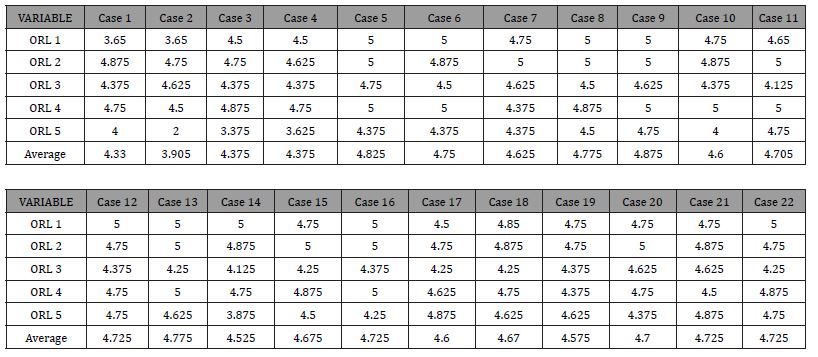
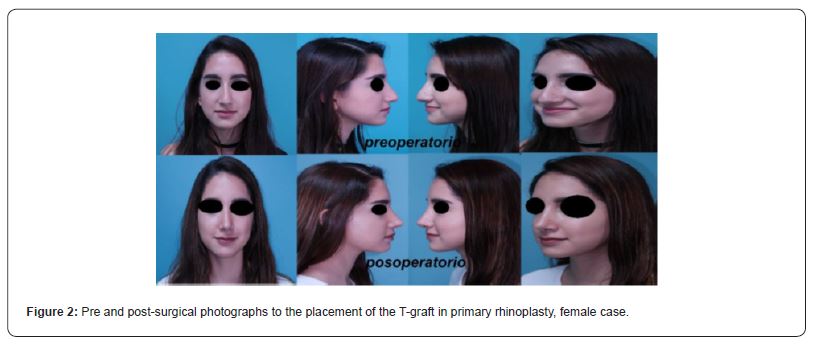
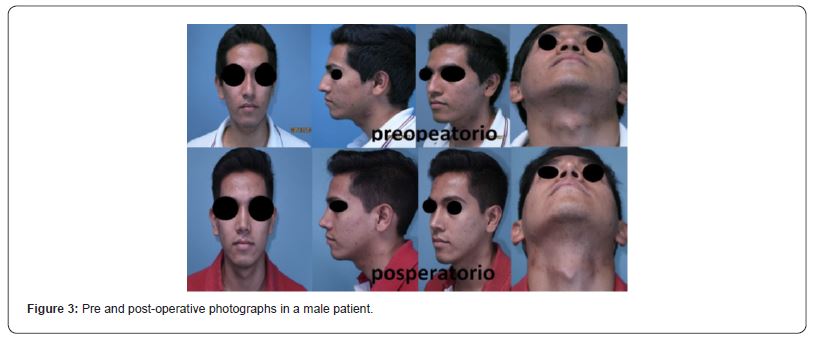
In none of the cases was asymmetry of the tip shown after the surgical procedure. In addition, there was no noticeable visibility of the graft reported in any patient. There were no postoperative complications or postoperative aesthetic or functional discomfort (Figures 2, 3).
Discussion
The handling of the nasal tip is and will always be a challenge for the facial surgeon, especially in the case of the mixed nose, due to the multiple erratic characteristics that they usually have; in most cases they are hypoprojected and/or hyporotated together with other anatomical variations that are difficult to manage; such is the case of the weakness of the minor alar cartilages and the high thickness of the skin that make only skeletal repositioning surgery insufficient to adequately define and project the tip [6].
From these principles, there are a wide variety of grafts for rhinoplasty; however, the search for a prosthetic material with the ideal shape and characteristics continues.
Generally speaking, the ideal graft must meet certain characteristics such as easy obtaining, low cost, it must not cause morbidity, easy remodeling, as well as effective biological integration in the recipient area. It must maintain its shape over time, not be an infectious vector and be resistant [5-11].
The anchor graft described by Gunter receives its name from the shape of its design; it is sutured to the caudal edge of the medial cruras and the transverse component can replace the lateral crura or be placed over its remnants. It is used to improve support, projection or both, as well as collapse or deformation of the lateral crura [12].
The biggest drawback of this type of graft is that it is often noticeable through the skin, even thick skin, so it is recommended to leave the edges beveled to avoid this complication.
The shield graft, also called Sheen, is a graft that increases the definition of the nasal tip, versatile with a trapezoidal shape (although its shape may vary) and is positioned superficial to the median cruras in the midline; can be used as camouflage for asymmetrical domes and forked nasal tip; It can also be used to give more or less projection to the tip [13-15].
Mostly used in patients with thick skin to increase the definition of the tip, its main complication is its protrusion through the skin (especially thin skin) and deformity of the nasal tip, which is avoided by carefully carving and using morcelized cartilage to avoid its visualization, however, due to its shape, this graft only protrudes 2 millimeters above the domes, and is often insufficient, compared to the “T” graft, which due to its shape can protrude at least 5mm above the domes. , likewise achieve camouflage of asymmetries in the nasal tip.
The “T” graft has been used by the authors successfully for several years in cases in which it is necessary to increase the projection or definition of the nasal tip that cannot be reached by sutures or other previously described grafts [16-19].
Although the history of the graft described here does not exist as such, Juri [20] described a procedure in which prosthetic material called “champagne glass” is used, which is placed through the Rethi incision. Said graft presents similar characteristics to the one proposed here, in the same way it has a similar design; and obtained results similar to ours; however it is little known and therefore has fallen into disuse. It is possible that these coincidences in terms of design have been fostered due to the characteristics of Latin American societies.
By protruding from the domes it achieves a similar projection when placing 3-4 pecks, favors projection, rotation and definition of the tip in an important way, helps to manage thick skin and bumpy tips. Among the variables analyzed, the greatest gain was observed in the rotation, projection, and definition of the nasal tip. For the evaluation of the variables of symmetry and double columnar break, it is important to consider that, only in the case of pre-surgical asymmetry or a rectified columnella, post-surgical improvement can be achieved; in cases in which there was no prior asymmetry or if the patient naturally had a pre-surgical double columnar break, there is no gain in this aspect. A longitudinal study with control photographs with a longer post-surgical time is required to determine the percentage of resorption that the cartilage graft may have and the long-term result of the placement of this type of graft. Another pertinent observation in the cases of nasal hump is that the handling should be done at the end of the work of the lobe, since the necessary reduction in the hump after the projection gained by means of this technique will be remarkably less, and in the cases of small humps No modification of the back is required anymore, or only regularization with a rasp [21].
Conclusion
The “T” graft described here is innovative as it results in projection rotation and definition of new domes which can currently be obtained through other techniques, but not with other point grafts, the gain achieved on the domes is between 5 to 7mm. It can be used successfully in cases where it is necessary to increase the projection, definition and rotation of the nasal tip that cannot only be achieved by means of sutures or other types of grafts. It is especially useful in cases of thick skin, and when remaining above the domes, favors a natural aesthetic result. In addition, it is a useful graft in cases of asymmetry of alar cartilages and for correction in some cases of the wing-columnella relationship.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Giacomotti JD, Bertone VH, Ottone NE, Medan CD, Tejedor M et al. (2013) Anatomy of the Nasal Tip. Rev Arg Anat Onl 4(1): 6-13.
- Gálvez Chávez JC, Yvan Millian J (2007) Anthropometric changes in the mixed-race nose after open rhinoplasty. Rev Cubana Cir [Internet magazine] 46(4): 14.
- Canto Vidal B, Canto Vigil T (2010) Rhinoplasty in Mestizo and Black Noses. Electronic Journal of Medical Sciences in Cienfuegos ISSN:1727-897X Medisur 8(1).
- Byrd HS, Hobar PC (1993) Rhinoplasty: A practical guide for surgical planning. Plast Reconstr Surg 91: 642-656.
- Gunter JP, Landecker A, Cochran CS (2006) Frequently used grafts in rhinoplasty: nomenclature and analysis. Plast Reconstr Surg 118: 14e-29e.
- Morera SE, Escobar FC, Pedroza CF, Frontera GJ (2008) Long-term Changes on Nasal Tip in Rhinoplasty Patients Operated With the New Domes Technique and the Banner Technique. Acta Otorrinolaringol Esp 8: 390-398.
- Toriumi DM (2006) New concepts in nasal tip contouring. Arch Facial Plast Surg 8(3): 156-185.
- Ansari Κ, Asari Κ, Asaria J, Hilger P (2008) Grafts andimplants in rhinoplasty -Techniques and long-term results. Op Tech Otolaryngol Head Neck Surg 19: 42-599.
- Casanueva F, Rosel P (2014) Domal cephalic point in rhinoplasty: A new alternative in nasal tip contours. Rev Otorhinolaryngol Cir Head Neck 74: 208-214.
- Faba G, Cornejo S, Gutiérrez D, Breinbauer H (2011) Grafts in rhinoseptoplasty: Experience of the Otorhinolaryngology Department of the Pontificia Universidad Católica de Chile. Rev Otorhinolaryngol. Cir Head Neck 71: 14-22.
- Tardy ME, Denny J, Fritsch ΜΗ (1985) The versatile cartilage autograft in reconstruction of the nose and face. Laryngoscope 95: 523-533.
- G Botti (1996) Thick skin and cosmetic surgery of the nasal tip: how to avoid the cutaneous polly beak. Aesthetic Plast Surg 20: 421-427.
- Casanueva F (2016) Nasal tip grafts in primary rhinoplasty. Journal of Otolaryngology and Head Neck Surgery 76: 21-30.
- Pedroza L (2013) Technique the standard in the correction of thick noses in primary rhinoplasty. CES University, Bogota-Colombia.
- Tham C, Lai YL, Weng CJ ET AL (2005) Silicone augmentation rhinolasty in an Oriental population. Ann Plast Surg 54: 1-5.
- Pedroza F A (2002) 20-year review of the “new domes” technique for refining the drooping nasal tip. Arch Facial Plast Surg 4:157-163.
- Scoenrock Ld, Repucci Ad (1994) Correction of subcutaneous facial defects using Gore-Tex. Fac Plast Surg Clin N Am 2: 373-388.
- Faba G, Cornejo S, Gutiérrez D, Breinbauer H (2011) Grafts in Rhinoseptoplasty. Journal of Otolaryngology and Head Neck Surgery 71: 14-22.
- Shirakabe Y, Suzuki Y, Lam Sm (2003) A systematic approach to rhinoplasty of the Japanese nose. A thrirty-year experience. Aesthetic Plast Surg 27: 221-231.
- Juri J, Juri C, Grilli A, Zeaiter MC, Belmont J (1986) Correction of secondary nasal tip. Annals of plastic surgery 16(4): 322-332.
- Ozturan O, Yenigun A, Tugrui S (2018) Adjunctive Use of the Dermocartilaginous Ligament for Dorsal Irregularities in Primary Rhinoplasty. J Craniofac Surg 29(6): e618-e621.
-
Antonio de Jesús Adame Legorreta*, Mónica Mariana Paz Alonso and Julio César López-Valdés. Evaluation of the Level of Hetero Perception of the “T” Graft for the Management of Nasal Tip in A Group of Mexican Patients. On J Otolaryngol & Rhinol. 6(1): 2022. OJOR.MS.ID.000629.
-
Nasal surgery, Nasal tip, Rhinoplasty, T-graft, Nose, Neck, Primary rhinoplasty, Mixed nose, Facial surgeon, Thick skin.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






