 Research Article
Research Article
Comparison of Conventional Single-Frequency Tympanometry with Pressure-Less Acoustic Immittance Measurements of Pathological and Normal Middle Ears
Moayad Anbari1, Shirin Zhumabaeva2, Munar Beishenova2, Dörte Fischer1,3, Shayirbek Sulaimanov2 and Tino Just1*
1Department of Otorhinolaryngology, Head and Neck Surgery, KMG Klinikum, Güstrow, Germany
2Department of Otorhinolaryngology, The National Center of Maternity and Childhood Care, Bishkek, Kyrgyzstan
3Department of Audiology, KMG Klinikum, Güstrow, Germany
Moayad Anbari (OCRID-ID: 0009-0003-5565-6437)
Dr. Shirin Zhumabaeva (OCRID-ID: 0000-0002-9073-1127)
Dr. Munar Beishenova (OCRID-ID: 0009-0000-8375-2563)
Dr. Dörte Fischer (OCRID-ID: 0000-0003-3736-4441)
Professor Shayirbek Sulaimanov (OCRID-ID: 0000-0002-0980-0501)
Professor Tino Just (OCRID-ID: 0000-0003-2036-8569)
Tino Just, M.D., Department of Otorhinolaryngology, Head and Neck Surgery Friedrich-Trendelenburg-Allee 1, D-18273 Güstrow, Germany.
Received Date: November 20, 2024; Published Date: November 27, 2024
Abstract
With a pressure free measurement of the acoustic immittance (PLAI) an acoustic signal (100 – 3000 Hz) is given into the outer ear canal. The technique provides the resonance frequency (RF) and the peak of the admittance.
Aim of this prospective pilot study was to measure the reliability of PLAI and to compare the results with those of the conventional tympanometry. Additionally, it was assessed whether PLAI may differentiate between healthy and pathological tympanic membrane/middle ear.
Material and Methods: PLAI measurements were performed with a CE-certified system MedWave® (Neuranix, Italy). In this prospective study 103 subjects of two Departments of Otorhinolaryngology at the mean age of 53.4 ± 17.2 years (59 men and 44 women) (middle ear group, 70 patients: 15 unilateral and 55 bilateral) and healthy subjects with normal bilateral ears (N=33) were included.
The participants of the study, patients and healthy subjects, obtained a medical report on ear, nose and throat examination, video otoscopy, a pure tone audiometry, PLAI measurement using MedWave® (Neuranix, Italy), conventional tympanometry, and finally a video endoscopy with Valsalva maneuver (forceful attempt of exhalation against a closed airway) in patients with tube ventilations problems or retraction pockets.
Results: The internal consistency is for both, PLAI and tympanometry, satisfying, with Cronbach’s alpha for >.82. For all correlational analyses between measurement 1 and 2, a significant correlation was found for frequency, peak, SC, TPP, ECV and TW (all r’s > 7.1 and all p’s < .001). Additionally, a correlation was found between PLAI peak and the ear canal volume (ECV) (measurement 1 r41= 0.678, p <.001 and measurement 2 r41=.722, p<.001).
For the 73 healthy subjects (normal tympanic membrane and tympanogram type A) the PLAI measurements revealed an average resonance frequency of 397 Hz ± 55.3 Hz ranging from 290-554 Hz and an average peak of 1.65 10-2 mmho was found. While in chronic tube ventilation disorders (N=26) and tympanic membrane perforations ((N=18) a large variability of the PLAI measurements were detected, in patients with acute middle ear infection increased RF values and peaks were measured (528 Hz ± 58.4 Hz ranging from 403 to 597 Hz and a peak of 17.2 10-2 mmho). Only in this group, the agreement of PLAI diagnosis (soft/perforation) and otoscopic diagnosis was higher than 70%.
Conclusion: PLAI provides reliable measurements in healthy subjects and variable values in otoscopic diagnoses like chronic otitis with tympanic membrane perforation. These results can be explained by the discontinuity of the ossiclular chain and stapes fixation due to tympanosclerosis which were not detected by otoscope prior to surgery.
A prospective study with a larger population with chronic otitis and otosclerosis is needed to evaluate the diagnostic value of PLAI in diagnosis of pathologic ears.
Introduction
Single-frequency impedance tympanometry is a well-accepted procedure to assess the middle ear function and is used in many ENT clinics since the 1970s. These tympanometric instruments generated impedance measurements. The Jerger’s classification [1] systems is also well accepted for daily use.. The large variability in measurements and tympanogram shapes in relation of large differences in the patient’s ear canal volume, lead to a limitation to the accuracy of the impedance tympanograms [2]. In 1971, a first admittance instead of impedance tympanometer was available. Several improvements were done to obtained calibrated measurements in absolute physical units (mmho) rather than arbitrary units and to provide constant sound pressure levels.
In the 1980s, multifrequency tympanometry (MFT) was introduced for clinical application allowing an evaluation of the middle ear acoustic-mechanical response at frequencies between 200 and 2,000 Hz. Feldman demonstrated the advantage of highfrequency tympanometry in the relation of mass-related pathologies of the middle ear [3]. The normal patterns for susceptance and conductance tympanograms based on the number of peaks when using a 678-Hz probe tone was described by Vanhuyse [4]. In comparison to 226-Hz tympanometry, analysis of the susceptance and conductance tympanogram peak patterns at higher probe tone frequencies provides information about changes in mass, stiffness, and resonance frequency. It was found that these measures are advantageous over 226-Hz tympanometry in the diagnosis of middle ear pathology.
Despite many advantages of MTF over single-frequency tympanometry, MTF has not gained widespread acceptance due to several reasons [5]. Main factors were time for additional testing, training, and the availability of MTF devices.
In the early 1980, wideband ear canal recordings are reported that allows measurements of acoustic impedance at frequencies above 2,000 Hz [6]. Margolis et al. showed that wideband reflectance increased frequencies from 250 through 11,300 Hz [7]. Wideband acoustic immittance (WAI) uses a different calibration method than tympanometry. For WAI measurements, ambient and static ear pressures used instead of pressurization of the outer ear canal. The advantage of WAI was to avoid pressure-induced changes of the outer ear canal walls [8]. In newborns it has been demonstrated, that pressurization of the outer ear canal may lead swelling and collapsing of the immature ear canal walls [9]. An increased number of reports were published on the application of WAI in newborn, children, and adults [10-15].
Then, about 10 years later, WAI testing was combined with pressurization of the outer ear canal. Several studies showed that wideband measurements obtained at various ear canal pressures might increase the sensitivity of WAI to diagnose middle ear diseases [16]. The combination of WBI and tympanometry using various static ear canal pressures has named wideband tympanometry (WBT) [17]. WBT assesses the middle ear function with a wideband stimulus (i.e., acoustic click, chirp frequencies between 226-8000 Hz) [18]. It has been demonstrated that the wideband stimulus is more efficient and precise for assessment of the middle ear and is less susceptible to myogentic noise [15]. WBT seems to provide more detailed information on the ear drum-ossicular system and allows a differential diagnosis of otosclerosis. Hein et al. demonstrated a typical absorbance profile of a patient with otosclerosis. The peak absorbance value shifted to higher frequencies. Another clinical application is the wideband absorbance measurement of newborns. Several studies revealed a significant modification of the values of the wideband absorbance within the first months of life caused by development of the external and middle ear [19-21]. Due to the differences of the size of the outer ear canal of adults and neonates, the absorbance measurements between adults and neonates differs significantly. In neonates, absorbance values at low frequencies reveal a decrease at the frequency of 6 kHz [22, 23].
During the 2012 Eriksholm Workshop on wideband absorbance measures of the middle ear, consensus statements were developed, regarding the research needs. Future publications or datasets are needed with population means, population variance, effect size, and sensitivity and specificity for detecting pathologies. The frequency resolution of measurements needs to be specified in all research reports [24].
Aim of this pilot study was to measure the hearing impedance with a novel CE-certified pressure less diagnostic device in adults with various middle ear pathologies and to com-pare the results with those of conventional single frequency impedance tympanometry [25]. The operating principle of PLAI (Pressure Less Acoustic Immittance) is based on new generation electronic components (precision microphones, MEMS Micro-Electro- Mechanical Systems), capable of measuring the acoustic signal in the ear canal and, based on the evaluation of the response in a range between 100 and 3000 Hz, to calculate the Complex Acoustic Admittance.
Material and Methods
Ethical Considerations
The design of the study was approved by the Ethics Committee of the General Medical Council of Mecklenburg West Pomerania (A2024-0183). This prospective study was conducted in strict adherence to the revised version of the Helsinki Declaration.
Participants
For participation, the inclusion criteria were patients with middle ear diseases of one or both ears aged 18-90 years. Patients younger than age of 18, patients with cochlea or middle ear implants, patients with glomus tumor and cognitive disorders were excluded.
Overall, 103 subjects of two Departments of Otorhinolaryngology at the mean age of 53.4 ± 17.2 years (59 men and 44 women) (middle ear group, 70 patients: 15 unilateral and 55 bilateral) and healthy subjects with normal bilateral ears (N=33) were included.
Subjects with no history of inflammation or disease that has impacted the middle ear, nor any recent hearing disability and aural symptoms and normal tympanic membrane with no atrophy, scar, retraction or perforation were defined as normal.
Of the 103 patients (206 ears), 33 subjects had bilateral normal ears (66 normal ears) and 70 patients had either unilateral (15 patients, 15 ears) or bilateral pathologies (55 patients, 110 ears with disease). In summary, 81 normal ears and 125 pathological ears were considered for analyses.
All subjects were informed about the aims of the study and provided their written consent.
Procedure
The participants of the study, patients and healthy subjects, obtained a medical report on ear, nose and throat examination. In all participants, videootoscopy was performed and images and videos were stored. Two ENT surgeons analyzed the data and categorized each ear considering the outer ear canal and the tympanic membrane. In all healthy subjects, acute or chronic otitis and other pathologies were excluded.
All participants obtained a pure tone audiometry, pressure less measurement of acoustic immittance using MedWave® (Neuranix, Italy), conventional tympanometry, and finally a video endoscope with Valsalva maneuver (forceful attempt of exhalation against a closed airway) in patients with tube ventilations problems or retraction pockets.
PLAI (Pressure Less Acoustic Immittance)
The end of the MedWave® probe was inserted in the lateral portion of the external outer ear canal. The test system applies a 100 to 3000 Hz signal. Evaluation of the responses results in a calculation of the complex acoustic admittance. MedWave® provides objective numerical terms: Fr (Hz)- value of the frequency at which the maximum value of the admittance curve occurs and P (Peak Admittance Value).
Conventional tympanometry
Tympanometry was performed with Madsen® Zodiac (type 1096) (Otometrics) at 226Hz from -400 to +200 daPa. The following results were used for calculation: TPP (tympanometric peak pressure), ECV (equivalent ear canal pressure), ECV (equivalent ear canal volume), and SA (static peak admittance) and type of the tympanogram (Jerger types: A (peak within normal limits for both pressure and height), Ad (peak is within normal limits for pressure but shows more compliance than normal), As (peak is within normal limits for pressure but shows less compliance than normal), B (flat with no significant peak), C the height of the peak is or is not within normal limits and is more negative than normal).
After classification of the otoscopic finding (normal or abnormal) conventional tympanometry was classified.
For test-retest reliability healthy subjects with normal ear (normal outer ear canal and normal tympanic membrane) and tympanogram type A were included. In one ear, no sufficient closure of the outer ear canal could be reach while measuring the tympanometry (case excluded).
Statistical Analyses
To measure the stability and precision of PLAI and conventional measurements, Cronbach’s reliability statistic was performed. Statistical tests (Kolmogorov test and Shapiro-Wilk test) indicated non-normal distribution for all parameters, all p’s<.05. Nonparametric tests were performed for group comparisons whenever appropriate. Pearson statistic was used for correlational analyses.
The alpha level was set to 0.05. SPSS version 30.0 (SPSS Inc. Chicago, IL, USA) was used for statistical analyses.
Results
Overall, 81 ears (33 healthy subjects with bilateral normal ears (N=66) and the contralateral ear of 15 patients with unilateral ear pathology) were classified as normal (normal tympanic membrane and outer ear canal and normal hearing).
73 out of the 81 normal ears revealed a tympanogram type A (As and Ad were excluded). For those participants, the PLAI measurements were used to create normative data of PLAI. 41 out of 73 ears were tested twice to analyze the test-retest reliability.
For reliability analysis, Cronbach’s alpha was calculated to assess internal consistency for PLAI and tympanometric measurements (Table. 1). The internal consistency is for both, PLAI and tympanometry, satisfying, with Cronbach’s alpha for >.82.
Table 1: Test-Retest reliability (Cronbach’s alpha) for normal ears) (N=41).
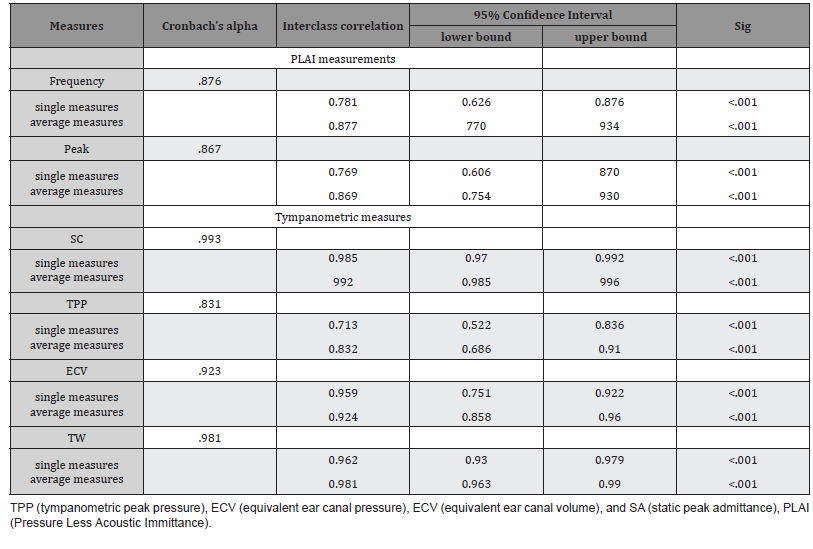
For all correlational analyses between measurement 1 and 2, a significant correlation was found for frequency, peak, SC, TPP, ECV and TW (all r’s > 7.1 and all p’s < .001). Additionally, a correlation was found between PLAI peak and the ear canal volume (ECV) (measurement 1 r41= 0.678, p <.001 and measurement 2 r41=.722, p<.001).
For the 73 ears the PLAI measurements revealed an average resonance frequency of 397 Hz ± 55.3 Hz ranging from 290-554 Hz and an average peak of 1.65 10-2 mmho was measured (Table 2 and Figures 1 and 2).
Table 2: Descriptive statistics of PLAI measurements.
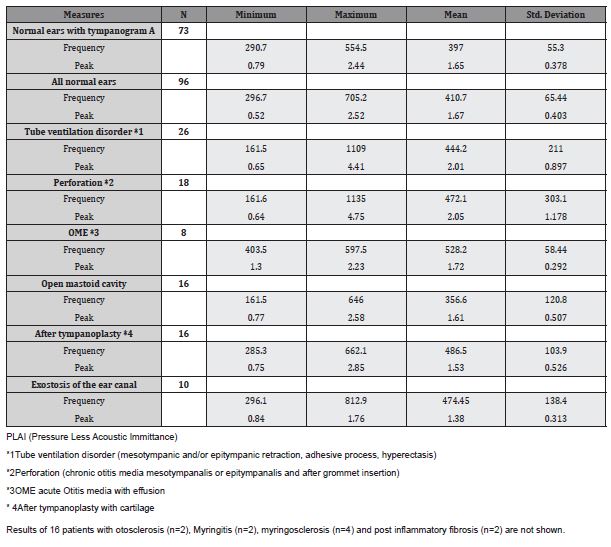
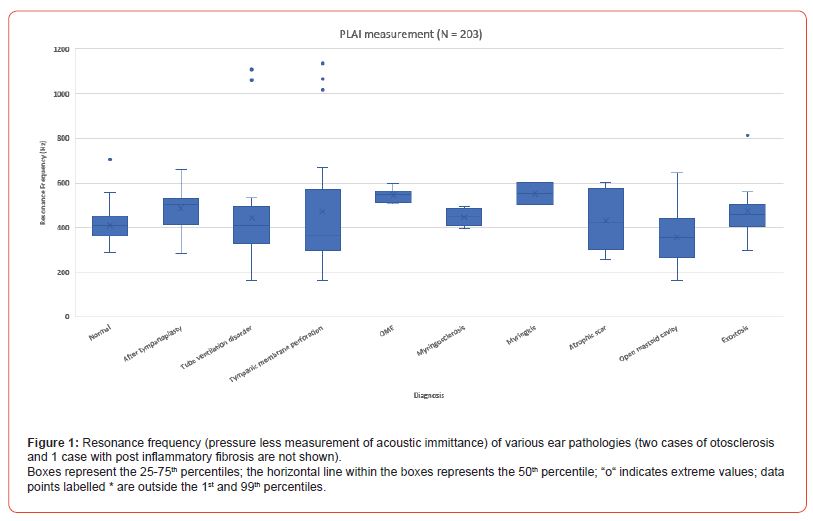
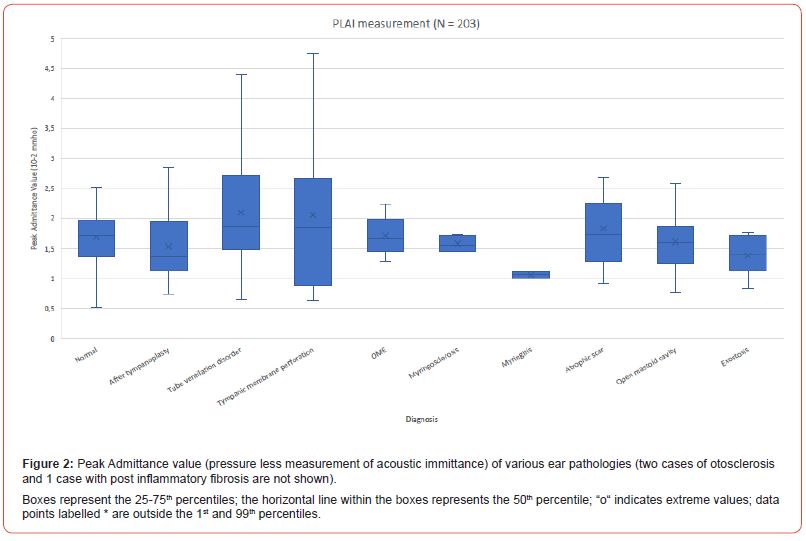
For all 26 ears with tube ventilation disorder (mesotympanic and/or epitympanic retraction, adhesive process, hyperectasis) without middle ear effusion an average resonance frequency of 444 Hz ± 211 Hz ranging from 161-1109 Hz an average peak of 2.01 10-2 mmho was determined.
Eighteen Patients with perforation of the tympanic membrane (chronic otitis media mesotympanalis or epitympanalis and after grommet insertion) revealed an average frequency of 472 Hz ± 303 Hz ranging from 161-1136 Hz.
For those patients with acute middle ear inflammation with effusion an average resonance frequency of 528 Hz ± 58.4 Hz ranging from 403-597 Hz an average peak of 1.72 10-2 mmho was found.
In those 73 ears with a normal tympanic membrane and a tympanogram type A 57 ears (78%) revealed a normal finding with PLAI (Table 3).
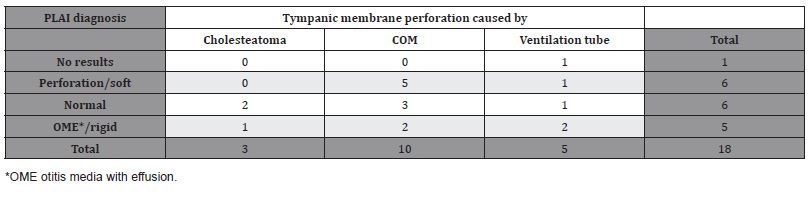
Eighteen out of 206 participants had a tympanic membrane perforation detected by otoscopy. Using PLAI measurement, 33% were diagnosed “perforation” (Table 4). Six patients were categorized as normal and five patients as OME using PLAI. In one patient no result was presented by PLAI.
Table 3: PLAI diagnosis in participants with a normal tympanic membrane tympanogram type A (N=73).
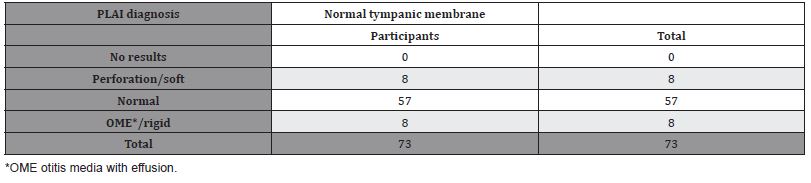
Table 4: PLAI diagnosis in tympanic membrane perforation (N=18).
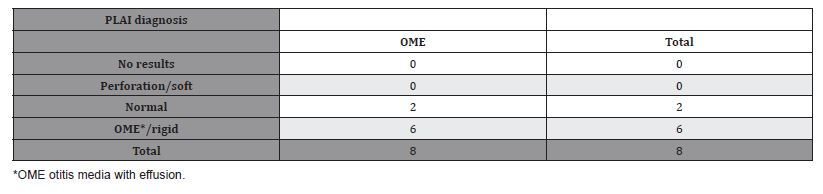
Otitis media with effusion was detected by otoscopy in eight patients. Using PLAI, 75% were diagnosed as OME while the remaining two patients were categorized as normal (Table 5).
Table 5: PLAI diagnosis in OME (N=8).
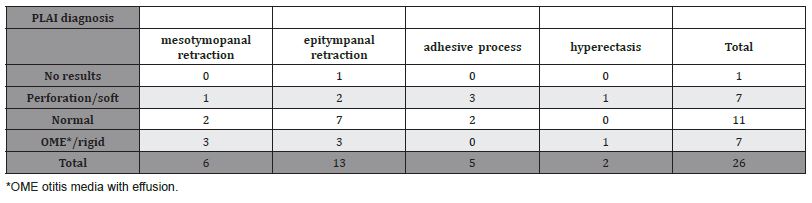
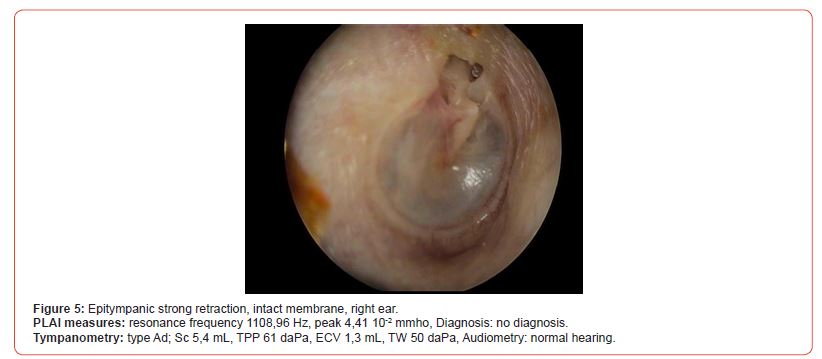
A tube ventilation disorder was diagnosed in 26 patients (Table 6). For two patients, a mesotympanic perforation was indicated by using otoscopy. Pneumatic otoscopy revealed a strong retraction pocket instead of a perforation. About 50% of the ears with epitympanal retraction was classified as normal with PLAI.
In seven cases, the diagnosis perforation was made using PLAI, whereby a perforation was excluded by pneumatic otoscopy.
In all 5 cases with adhesive process, the aeration of the upper parts of the tympanic membrane was visible during Valsalva maneuver.
Table 6: PLAI diagnosis in tube ventilation disorders (N=26).
Figures 3-6 show characteristic findings of four ears with adhesive process, epitympanic retraction and hyperectasis. In the 5 cases with adhesive process and also in hyperectasis, the resonance frequency was between 296-333 Hz, Resulting in lower values than the average value of the normal ears (397 Hz, Table 2). Epitympanic retractions show a large variation of the resonance frequency.
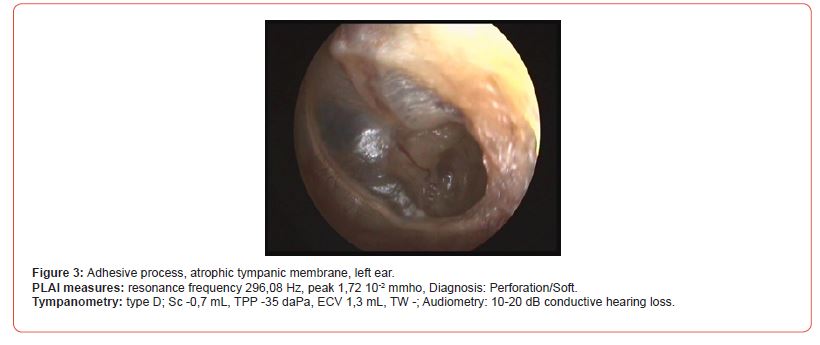
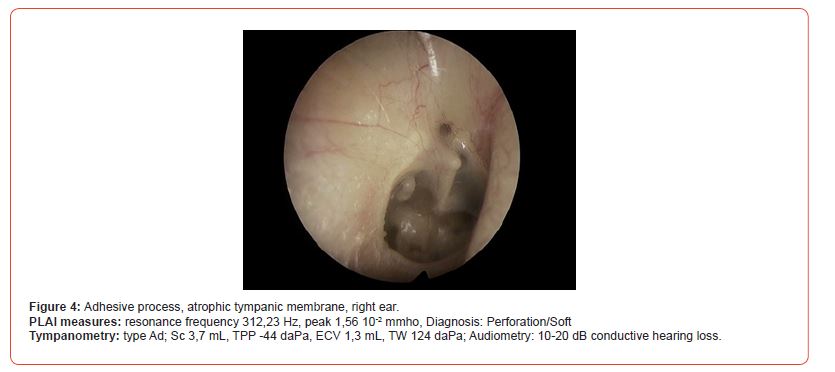

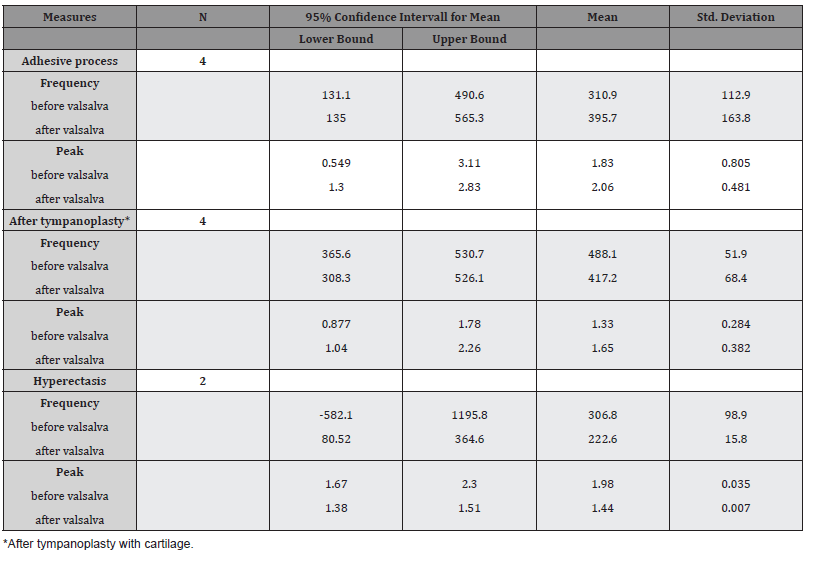
In 10 ears with three different conditions PLAI measurements were performed before and after Valsalva maneuver. In cases of an adhesive process the attachment of the tympanic membrane onto the promontory was detected by video endoscopy. During Valsalva maneuver the upper part of the tympanic membrane showed clearly an aeration and excavation of the tympanic membrane. PLAI measurement (Table 7) revealed a lower mean resonance frequency compared to normal ears (Table 2) before Valsalva maneuver.
Valsalva maneuver tends to slightly increase the resonance frequency in adhesive process and to decrease the admittance peak after tympanoplasty.
Table 7: Descriptive statistics of PLAI measurements before and after Valsalva maneuver (N=10).
Discussion
Conventional single-frequency (226 Hz) tympanometry is routinely used in many clinics and outpatient departments to detect middle ear pathologies since the 1970s [5]. It is influenced by the stiff-ness property of the middle ear. Mass loading of the ossicles may impair ossicular dynamics and sound transmission of higher frequencies to the inner ear. This might not be detected by singlefrequency (226 Hz) tympanometry. Therefore, the diagnostic application of this method is limited [26]. However, there is the possibility to change the frequency for measuring, but is still unclear what frequency is most suitable for a given patient. Conventional tympanometry uses pressure changes of the outer ear canal. This may lead to a collapse of the outer ear canal and pain in newborns. Several tympanic conditions, such as perforation of the tympanic membrane, cartilage-reconstructed tympanic membranes and ventilation tubes) provide no results using tympanometry.
WAI is an alternative immittance measuring method that might provide information of the middle ear without pressure. WAI uses a wideband stimulus over a wide range of frequencies and measures the energy reflected back from or absorbed into the tympanic membrane and the middle ear. In contrast to conventional tympanometry, WAI reflects the mass, stiffness and resonance frequency of the middle ear. Several studies show that WAI provides value information to predict and differentiate various middle ear diseases [12, 14, 27-30]. However, WAI has not yet been integrated in clinical practice for several reasons. Among these, no access to equipment, lack of training and /or confidence in measuring WAI [31] and complexity of interpreting WAI measures [30, 32] can be mentioned.
In this pilot study, single-frequency tympanometry was used to diagnose various conditions of the outer ear canal, tympanic membrane and the middle ear to assess the influence of Valsalva maneuver on the PLAI results. In a first step the reliability of PLAI measurements were compared with those of conversional single frequency tympanometry in healthy ears. There were no differences found between the measurements of both methods in all parameters. The internal consistency values were in all parameters better than 0.87 for PLAI (ranging from 0.87 to 0.88) and 0.83 for tympanometry (ranging from 0.83 to 0.99) (Cronbach’s alpha).
A limitation of this pilot study was the reduced number of patients for the various groups. However, some results are discussed in more detail. While 75% of those with OME were diagnosed as “OME” using PLAI, only 33% of the patients with perforation of the tympanic membrane were identified as “perforation”. This group showed the highest variation of the measurement results. The effect of location and size of the perforation on the PLAI measurements needs to be assessed in a larger population. Additionally, the testretest results before and after Valsalva maneuver reveals that pressurization prior to PLAI measurements seems to have a strong impact on the test results. A strong retraction of the tympanic membrane/retraction pocket before Valsalva maneuver provides different test results after Valsalva maneuver. In some cases, a ballooned (hyperinflated) tympanic membrane was determined after Valsalva maneuver. This hyperinflation may also occur in patients with atelectatic ears. Several authors demonstrated that using tympanometry after walking in the morning, a hyperectasis (ballooned tympanic membrane) [33-35] appeared and returned to the former retracted atelectatic degree. Therefore, otoscopy prior to PLAI measurement is needed to explain the test results. Additionally, pressurization (Valsalva maneuver, tympanometry) before PLAI measurement has also been considered.
With the knowledge that newborns and children provides different normative values, we focused in this pilot study on patients over the age of 18 years. We found reliable results in healthy subjects. However, in patients with middle ear diseases, there is also a spectrum of factors that may affect the PLAI results, e.g. the size of the outer ear canal. We demonstrated that exostosis may also affect the PLAI measurements even when the tympanic membrane is normal. The stiffness of the tympanic membrane increases after cartilage tympanoplasty. This also affects the resonance of outer and middle ear systems, depending on the thickness of the cartilage used for reconstruction of the tympanic membrane. In further studies, the biological material, fascia or cartilage, has to be considered.
To better understand and interpret the PLAI results and further to facilitate its clinical application further studies should focus on various conditions of the middle ear, e.g. chronic otitis media with or without perforation, otosclerosis and ventilation disorders.
Keypoints
- Pressure less acoustic immittance measurements provides a good test-retest reliability results
- PLAI provides in nearly all cases reliable test results regardless of the condition of the tympanic membrane
- Atelectatic middle ears (mesotympanic retractions, adhesive process) characteristically decrease the resonance frequency of the middle ear
- OME increase the resonance frequency of the middle ear
Acknowledgement
None.
Conflict of Interest
The authors have no funding and no conflicts of interest to disclose.
References
- Jerger J (1970) Clinical experience with impedance audiometry. Arch Otolaryngol 92(4): 311-24.
- Shahnaz N, Al Makadma H, Sanford CA (2023) The Rise and Fall of Aural Acoustic Immittance Assessment Tools. Semin Hear 44(1): 5-16.
- Feldman AS (1976) Tympanometry: application and interpretation. Ann Otol Rhinol Laryngol 85(2 Suppl 25 Pt 2): 202-8.
- Vanhuyse V, Creten W, Van Camp K (1975) On the W-notching of tympanograms. Sacand Audiol 4(1): 45-70.
- Emanuel DC, Henson OE, Knapp RR (2012) Survey of audiological immittance practices. Am J Audiol 21(1): 60-75.
- Stinson MR, Shaw EA, Lawton BW (1982) Estimation of acoustical energy reflectance at the eardrum from measurements of pressure distribution in the human ear canal. J Acoust Soc Am 72(3): 766-73.
- Margolis RH, Saly GL, Keefe DH (1999) Wideband reflectance tympanometry in normal adults. J Acoust Soc Am 106(1): 265-80.
- Keefe DH, Levi E (1996) Maturation of the middle and external ears: acoustic power-based responses and reflectance tympanometry. Ear Hear 17(5): 361-73.
- Holte L, Margolis RH, Cavanaugh RM (1991) Developmental changes in multifrequency tympanograms. Audiology 30(1) :1-24.
- Ellison JC, Gorga M, Cohn E, Fitzpatrick D, Sanford CA, et al. (2012) Wideband acoustic transfer functions predict middle-ear effusion. Laryngoscope 122(4): 887-94.
- Keefe DH, Bulen JC, Arehart KH, Burns EM (1993) Ear-canal impedance and reflection coefficient in human infants and adults. J Acoust Soc Am 94(5): 2617-2638.
- Feeney MP, Grant IL, Marryott LP (2003) Wideband energy reflectance measurements in adults with middle-ear disorders. J Speech Lang Hear Res 46(4): 901-911.
- Hunter LL, Tubaugh L, Jackson A, Propes S (2008) Wideband middle ear power measurement in infants and children. J Am Acad Audiol 19(4): 309-324.
- Prieve BA, Feeney MP, Stenfelt S, Shahnaz N (2013) Prediction of conductive hearing loss using wideband acoustic immittance. Ear Hear 34 Suppl 1: 54S-59S.
- Prieve BA, Vander Werff KR, Preston JL, Georgantas L (2013) Identification of conductive hearing loss in young infants using tympanometry and wideband reflectance. Ear Hear 34(2): 168-178.
- Keefe DH, Simmons JL (2003) Energy transmittance predicts conductive hearing loss in older children and adults. J Acoust Soc Am 114(6 Pt 1): 3217-3238.
- Sanford CA, Hunter LL, Feeney MP, Nakajima HH (2013) Wideband acoustic immittance: tympanometric measures. Ear Hear 34 Suppl 1: 65S-71S.
- Hein TAD, Hatzopoulos S, Skarzynski PH, Colella-Santos MF (2017) Wideband tympanometry. In: Hatzopoulos S, (Edr.), Advances in Audiology: Intech; p. 29-42.
- Kei J, Sanford CA, Prieve BA, Hunter LL (2013) Wideband acoustic immittance measures: developmental characteristics (0 to 12 months). Ear Hear 34 Suppl 1:17S-26S.
- Aithal S, Kei J, Driscoll C (2014) Wideband absorbance in young infants (0-6 months): a cross-sectional study. J Am Acad Audiol 25(5): 471-481.
- Aithal V, Kei J, Driscoll C, Swanston A, Roberts K, et al. (2014) Normative sweep frequency impedance measures in healthy neonates. J Am Acad Audiol 25(4): 343-354.
- Hunter LL, Feeney MP, Lapsley Miller JA, Jeng PS, Bohning S (2010) Wideband reflectance in newborns: normative regions and relationship to hearing-screening results. Ear Hear 31(5): 599-610.
- Silva KA, Urosas JG, Sanches SG, Carvallo RM (2013) Wideband reflectance in newborns with present transient-evoked otoacoustic emissions. Codas 25(1): 29-33.
- Feeney MP, Hunter LL, Kei J, Lilly DJ, Margolis RH, et al. (2013) Consensus statement: Eriksholm workshop on wideband absorbance measures of the middle ear. Ear Hear 34 Suppl 1: 78S-79S.
- Terkildsen K, Nielsen SS (1960) An electroacoustic impedance measuring bridge for clinical use. Arch Otolaryngol 72: 339-346.
- AlMakadma H, Kei J, Yeager D, Feeney MP (2023) Fundamental Concepts for Assessment and Interpretation of Wideband Acoustic Immittance Measurements. Semin Hear 44(1): 17-28.
- Keefe DH, Sanford CA, Ellison JC, Fitzpatrick DF, Gorga MP (2025) Wideband aural acoustic absorbance predicts conductive hearing loss in children. Int J Audiol 51(12): 880-891.
- Merchant GR, Al-Salim S, Tempero RM, Fitzpatrick D, Neely ST (2021) Improving the Differential Diagnosis of Otitis Media With Effusion Using Wideband Acoustic Immittance. Ear Hear 42(5): 1183-1194.
- Merchant GR, Neely ST (2023) Conductive Hearing Loss Estimated From Wideband Acoustic Immittance Measurements in Ears With Otitis Media With Effusion. Ear Hear 44(4): 721-731.
- Sanford CA, Brockett JE, Aithal V, AlMakadma H (2023) Implementation of Wideband Acoustic Immittance in Clinical Practice: Relationships among Audiologic and Otologic Findings. Semin Hear 44(1): 65-83.
- Al-Salim S, Skretta D, Merchant GR (2024) Survey of Wideband Acoustic Immittance Use by Clinical Audiologists. Am J Audiol 33(1): 254-268.
- Grais EM, Wang X, Wang J, Zhao F, Jiang W, et al. (2021) Analysing wideband absorbance immittance in normal and ears with otitis media with effusion using machine learning. Sci Rep 11(1): 10643.
- Sade J (2001) Hyperectasis: the hyperinflated tympanic membrane: the middle ear as an actively controlled system. Otol Neurotol 22(2): 133-139.
- Hergies L, Magnuson N (1985) Morning pressure in the middle ear. Arch Otolaryngol 111: 86-89.
- Bylander A, Tjernstrom O, Ivarsson A, Andreasson L (1985) Eustachian tube function and its relation to middle ear pressure in children. Auris Nasus Larynx 12 Suppl 1: S43-S45.
-
Moayad Anbari, Shirin Zhumabaeva, Munar Beishenova, Dörte Fischer, Shayirbek Sulaimanov and Tino Just. Comparison of Conventional Single-Frequency Tympanometry with Pressure-Less Acoustic Immittance Measurements of Pathological and Normal Middle Ears. On J Otolaryngol & Rhinol. 7(2): 2024. OJOR.MS.ID.000659.
-
Middle ears, Ear canal, Otorhinolaryngology, ENT clinics, Ear pathology, Low frequencies, Tympanometry, Cochlea or middle ear implants, Cognitive disorders
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






