 Case Report
Case Report
Aggressive Mucormycosis in a Systemic Lupus Erythematosus Patient: A Case Report and Treatment Approach
Francisco Alves Mestre Neto1*, Marco Antônio Ricci2, Francisco Amadis Batista Ferreira2, Maria Zeina Michiles Sampaio3, Thais Mendonça de Lyra4, Marcos Antônio Fernandes5 and Rodolfo de Freitas Fagionato1
1Member of the Brazilian Medical Association (AMB), São Paulo, São Paulo, Brazil
2Medical and Dental Institute of the Amazon (IMOAM), Manaus, Amazonas, Brazil
3Amazonas State Intensive Therapy Institute (COOPATI), Manaus, Amazonas, Brazil
4Nilton Lins University, Manaus, Amazonas, Brazil
5Member of the Brazilian Association of Otorhinolaryngology (ABORL), Manaus, Amazonas, Brazil
Francisco Alves Mestre Neto, Member of the Brazilian Medical Association (AMB), São Paulo, São Paulo, Brazil.
Received Date: November 08, 2024; Published Date: November 15, 2024
Abstract
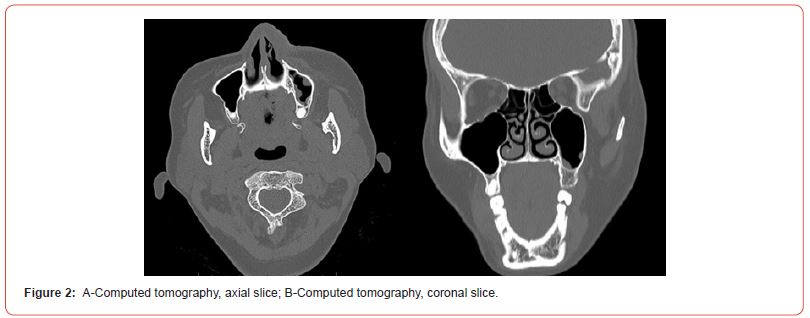
Mucormycosis is a rare, highly aggressive opportunistic fungal infection due to the rapid spread of the pathogen and necrosis of adjacent tissues, often resulting in death. Early diagnosis and prompt clinical and surgical treatment are essential. A 38-year-old female patient with a history of systemic lupus erythematosus presented at Dr. João Lúcio Pereira Machado Hospital and Emergency Room, referred from São Raimundo Emergency Service. She complained of fever, a darkened nasal region associated with itching, and respiratory and visual difficulties. During the physical examination, a necrotic lesion with hyperemic borders on the left nasal ala extending to the hard palate was observed, with hyperemic areas near the teeth of the left hemimaxilla and a whitish lesion suggestive of a necrotic process in the palatine region (Figure 2), leading to a presumptive diagnosis of mucormycosis. Hematological examinations and cranial and facial computed tomography were requested to clarify the case. The evaluation revealed irregular thickening in the subcutaneous cellular tissue, slight mucosal thickening in the left maxillary sinus membrane, and aeration of the middle nasal conchae. The treatment plan adopted included radical surgical debridement with biopsy, antifungal therapy with liposomal Amphotericin B at a daily dose of 08 mg/kg, and admission to the intensive care unit. The aggressive management, involving surgical debridement and antifungal therapy, proved effective for the patient, resulting in a favorable prognosis with no inflammatory or necrotic signs, effectively resolving the case.
Keywords: Mucormycosis; Lupus erythematosus; Treatment approach
Introduction
Mucormycosis is a potentially fatal fungal infection caused by fungi of the order Mucorales, which includes several genera, the most relevant being: Rhizopus spp., Mucor spp., Rhizomucor spp., Absidia spp. It can be classified into six distinct clinical groups based on the anatomical locations involved: rhinocerebral, pulmonary, cutaneous, gastrointestinal, and other or disseminated infections, depending on underlying conditions. Most manifestations are severe, typically starting as sinusitis and progressing to rhinoorbital infection, particularly in immunocompromised individuals [1].
It occurs primarily in immunosuppressed patients, patients with diabetic ketoacidosis or uncontrolled diabetes, those undergoing chemotherapy for lymphoproliferative disease, solid organ transplant recipients, patients with hemochromatosis, and those with concomitant infections [2].
Among these risk groups, patients with Systemic Lupus Erythematosus (SLE) stand out. SLE is a chronic autoimmune disease that affects multiple organ systems and often requires intensive immunosuppressive therapies, which increase susceptibility to opportunistic infections such as mucormycosis [3].
Mucormycosis in SLE patients is particularly concerning due to the combination of prolonged immunosuppression and the inherent immune dysfunction associated with the disease [4]. The rhinocerebral involvement is the most common clinical form, often initially presenting as sinusitis but rapidly progressing to orbital and cerebral involvement, further complicating clinical and surgical management. The infection develops aggressively, and without early diagnosis and immediate intervention, it leads to high mortality rates [5].
The general objective of this case report is to describe the clinical presentation, diagnosis, and management of an aggressive mucormycosis infection in a patient with Systemic Lupus Erythematosus (SLE), highlighting the challenges associated with the combination of prolonged immunosuppression and the underlying autoimmune disease. This report aims to illustrate the importance of early identification and prompt intervention in cases of mucormycosis in immunocompromised patients, with the goal of providing insights for clinical practice and improving outcomes in similar conditions.
Case Presentation
A 38-year-old female patient with fair skin and a previous diagnosis of systemic lupus erythematosus presented to the Dr. João Lúcio Pereira Machado Hospital and Emergency Room, referred by the São Raimundo Emergency Care Service, complaining of fever, darkening of the nasal region associated with itching, and respiratory and visual difficulties. During the physical examination, a necrotic lesion with hyperemic borders was observed in the left nasal ala region (Figure 1-A), extending to the hard palate, which showed hyperemic areas near the teeth of the left hemiarch, as well as a whitish lesion suggestive of a necrotic process in the palatal region (Figure 1-B). The presumptive diagnosis was mucor.

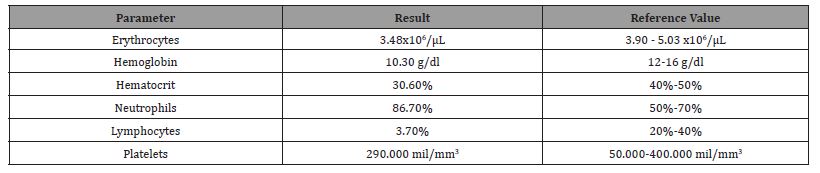
Hemotological examination and cranial and facial CT scans were requested to elucidate the case. Laboratory tests revealed erythrocytes, hemoglobin, hematocrit, and lymphocytes below the reference values (Table 1).
Table 1:Hematological test results.
The CT scan showed the cerebral parenchyma within normal limits, irregular thickening in the subcutaneous cellular tissue, slight mucosal thickening in the membrane of the left maxillary sinus, and aeration of the middle nasal turbinates (Figures 2).
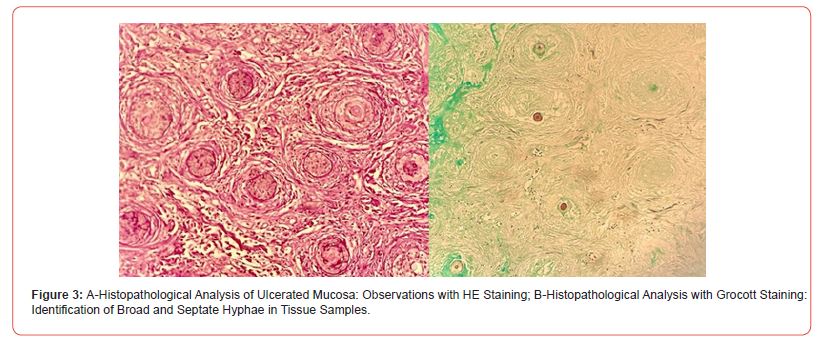
The treatment plan implemented included radical surgical debridement, followed by sending the material for histopathological examination and fungal culture. Antifungal therapy was initiated with liposomal Amphotericin B at a daily dose of 8 mg/kg, and the patient was admitted to the intensive care unit. The histopathological analysis revealed fragments of mucosa covered by ulcerated squamous epithelium, the formation of a fibrinoleukocytic crust, areas of necrosis, and a neutrophilic inflammatory infiltrate. Fungal examination using Grocott and PAS staining was positive, showing the presence of broad, septate hyphae (Figure 3). The findings are consistent with a diagnosis of mucormycosis.
The patient showed improvement after the surgical debridement procedure and antifungal therapy. On the 7th postoperative day, signs of tissue healing and regression of the fungal infection in the nasal ala region and hard palate were observed (Figure 4A and 4B).
After 14 days, the patient presented in good general condition, afebrile, normochromic, with a scarred appearance in the lesion area, and regression of the lesion in the palatal region (Figure 4C and 4D).
On the 30th day after debridement and antifungal therapy, the patient presented a good appearance in the nasal region and a cicatricial aspect in the left palatal region, with a discharge planned in two days for maintenance therapy with isavuconazole at home.
The patient returned to the hospital for a follow-up consultation 60 days after the procedure, presenting in good clinical condition, showing signs of fungal infection remission, and without any pain complaints, continuing treatment with isavuconazole at home (Figure 5). It is worth noting that the oral Isavuconazole treatment was continued for an additional 3 months due to an area on the palate that still showed signs of ischemia. Only after this phase was discharge considered, and the treatment for SLE could be adjusted.


Discussion
Patients with SLE, who are immunocompromised, exhibit intrinsic defects in immune function and hypogammaglobulinemia, and are often on immunosuppressive medications such as the anti- CD20 monoclonal antibody (mAb) rituximab and glucocorticoid therapy for the management of lupus nephritis [6]. Therefore, these patients, including the one described in this case report, are at high risk of developing invasive fungal infections.
Prolonged corticosteroid therapy increases the patient’s susceptibility to mucormycosis, leading to dysfunctions in macrophages and neutrophils [7].
There has been a significant increase in the incidence of opportunistic fungal infections worldwide, with an even sharper rise in mucormycosis cases. The clinical manifestations of mucormycosis are varied and depend on the patient’s immune status and underlying conditions [8]. The number of reports of mucormycosis in patients with Systemic Lupus Erythematosus (SLE) has also increased [9].
The occurrence of mucormycosis cases is influenced by climatic factors and seasonal changes, which affect the proliferation of the fungus responsible for the infection, with these elements being closely linked to geographical location [10]. The patient described lives in a region with a hot and humid climate, conditions that favor the dispersion of spores and their reproduction in the soil and organic matter.
The infection is primarily acquired through the inhalation of spores, ingestion of contaminated food, or through wounds and burns. Rhinocerebral mucormycosis is the most common clinical form, characterized by the involvement of the paranasal sinuses and the brain, followed by pulmonary involvement [8]. In the case in question, involvement of the nasal sinus, the nasal ala region, and the hard palate was observed.
Cornely and collaborators (2019) [11] recommend a multimodal approach to the treatment of mucormycosis, which includes radical surgical debridement or resection of the affected area, antifungal therapy, and strict control of predisposing factors such as uncontrolled diabetes mellitus and neutropenia. Smith and collaborators (2022) emphasize that the removal of infected tissue is crucial for the complete eradication of the infection in severe cases. However, surgical outcomes vary depending on each patient’s individual response and the extent of the intervention required for each specific case. Sipsas and collaborators (2018) [12] demonstrated that the resection of necrotic tissues can significantly increase survival rates compared to antifungal therapy alone. In the reported case, a radical surgical debridement was performed, combined with liposomal Amphotericin B at a dose of 8.0 mg/kg/ day, resulting in a remarkable regression of the disease. Evidence suggests that the ideal duration of treatment aligns with the improvement of immunosuppression and clinical findings, allowing for a possible transition to maintenance therapy with isavuconazole or posaconazole, even after the patient’s stabilization [13].
It is important to highlight that if the infection reaches the brain, the mortality rate can exceed 80%. In many cases, the cause of death is the mucormycosis itself rather than the progression of the underlying disease. Early diagnosis and a multidisciplinary therapeutic approach are crucial to reducing morbidity and mortality. Even with treatment, the overall prognosis is unfavorable, with a death rate of 40% to 50% among patients who develop rhinocerebral mucormycosis [11]. Since the underlying systemic disease is generally manageable, diabetic patients have a better prognosis compared to immunosuppressed individuals. If the patient survives, the significant tissue destruction that remains presents both functional and aesthetic challenges [14]. In the reported case, early diagnosis and combined therapy of surgical debridement with Amphotericin B were crucial for the favorable prognosis of the disease [15].
Conclusion
Patients with Systemic Lupus Erythematosus (SLE) face a high risk of developing invasive fungal infections such as mucormycosis, due to intrinsic immunosuppression and the use of immunosuppressive therapies. The combination of climatic and geographic factors can increase susceptibility to infection, particularly in regions with hot and humid climates, like the one where the patient in this case resides. Rhinocerebral mucormycosis, being the most common form of the disease, presents a significant therapeutic challenge, with a high mortality rate, especially when the infection extends to the brain. However, early diagnosis and an aggressive therapeutic approach, including radical surgical debridement and antifungal treatment with Amphotericin B, are crucial for improving prognosis. The described case highlights the importance of prompt and effective intervention to maximize survival chances and minimize functional and aesthetic complications associated with the disease.
Acknowledgement
None.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- Junqueira JT de S, Costa BDS, Almeida CLL de (2022) Mucormycosis: epidemiological aspects, diagnostic methods and therapeutic approaches. Brazilian J Dev 8(12): 80955-80968.
- Skiada A, Pavleas I, Drogari Apiranthitou M (2020) Epidemiology and diagnosis of mucormycosis: An update. J Fungi 6(4): 1-20.
- Sigera LSM, Gamage KKK, Jayawardena MN (2018) Cutaneous mucormycosis caused by Saksenaea vasiformis in a patient with systemic lupus erythematosus. Clin Case Reports 6(9):1730-1734.
- Prakash H, Chakrabarti A (2019) Global epidemiology of mucormycosis. J Fungi 5(1).
- Chandrasekar P, Miceli (2012) Safety and efficacy of liposomal amphotericin B for the empirical therapy of invasive fungal infections in immunocompromised patients. Infect Drug Resist 1(1): 9.
- Hung HC, Shen GY, Chen SC (2015) Pulmonary Mucormycosis in a Patient with Systemic Lupus Erythematosus: A Diagnostic and Treatment Challenge. Case Rep Infect Dis 2015: 1-5.
- Walsh TJ, Gamaletsou MN, McGinnis MR, Hayden RT, Kontoyiannis DP (2012) Early clinical and laboratory diagnosis of invasive pulmonary, extrapulmonary, and disseminated mucormycosis (zygomycosis). Clin Infect Dis. 54(SUPPL. 1): 55-60.
- Roden MM, Zaoutis TE, Buchanan WL (2005) Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis 41(5): 634-653.
- Weng CT, Lee NY, Liu MF (2010) A retrospective study of catastrophic invasive fungal infections in patients with systemic lupus erythematosus from southern Taiwan. Lupus 19(10): 1204-1209.
- Seidel D, Wurster S, Jenks JD (2024) Impact of climate change and natural disasters on fungal infections. The Lancet Microbe 5(6): e594-e605.
- Cornely OA, Alastruey Izquierdo A, Arenz D (2019) Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis 19(12): e405-e421.
- Sipsas NV, Gamaletsou MN, Anastasopoulou A, Kontoyiannis DP (2018) Therapy of mucormycosis. J Fungi 4(3): 1-17.
- Laquan Li, Wei Lu ST (2021) Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. IEEE Trans Radiat Plasma Med Sci 176(1): 139-148.
- Didehdar M, Chegini Z, Moradabadi A (2022) Gastrointestinal mucormycosis: A periodic systematic review of case reports from 2015 to 2021. Microb Pathog 163(December 2021): 105388.
- Wolthers MS, Schmidt G, Gjorup CA, Helweg Larsen J, Rubek N, et al. (2021) Surgical management of rhinocerebral mucormycosis: A case series. JPRAS Open 30: 33-37.
-
Francisco Alves Mestre Neto*, Marco Antônio Ricci, Francisco Amadis Batista Ferreira, Maria Zeina Michiles Sampaio, Thais Mendonça de Lyra, Marcos Antônio Fernandes and Rodolfo de Freitas Fagionato. Aggressive Mucormycosis in a Systemic Lupus Erythematosus Patient: A Case Report and Treatment Approach. On J Otolaryngol & Rhinol. 7(2): 2024. OJOR.MS.ID.000656.
-
Fungal infections, Rhinocerebral mucormycosis, Antifungal therapy, Pulmonary involvement, Nasal sinus, Systemic lupus erythematosus, Maxillary sinus, Nasal turbinates, Rhino orbital infection
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






