 Research Article
Research Article
A Clinical Epidemiological Study of Patients with Coronavirus Disease Associated Mucormycosis Treated at A Tertiary Care Nodal Centre
Mounika Reddy Y1*, Shankar T1, Manish Kumar1, Sreenivas K1 and Subramanyam Darbha2
1Department of Otorhinolaryngology, Head and Neck Surgery, Govt. ENT Hospital, Osmania Medical College, Hyderabad, India
2Subrahmanyam Darbha (M.S. Epidemiology, Public Health) Consultant Biostatistician (Independ-ENT)
Mounika Reddy Y, Postdoctoral Fellow in Implantation Otology, Department of Otorhinolaryngology, Head and Neck Surgery, Govt. ENT hospital, Osmania Medical College, Hyderabad-500095, India.
Received Date: December 16, 2021; Published Date: January 04, 2022
Abstract
Objective: The main objective of this study was to assess clinical and epidemiological factors associated with coronavirus disease associated mucormycosis (CAM) and furthermore to recognize the role of vaccination in preventing the progression of mucormycosis.
Materials and methods: A retrospective observational study was conducted on 300 patients with past history of being treat-ed for coronavirus disease and who presented to our department with symptoms of invasive fungal sinusitis. The data were analyzed to assess the factors associated with CAM.
Results and Conclusion: Receiving COVID-19 vaccination either one or two doses had some statistically significant associa-tion with CAM, however, only a small number of patients received vaccination doses. Other factors including age, gender, dia-betes (denovo vs. chronic), steroid use, oxygen, and remdesivir administration were not significant. Vaccination may play a key role in lessening the sequelae and mortality due to Covid-19 while providing protection against CAM.
Keywords: Coronavirus; Mucormycosis; Invasive fungal sinusitis; Diabetes Mellitus; Vaccination
Introduction
The global Coronavirus disease 2019 (Covid-19) pandemic has affected Indian subcontinent tremendously. It has affected more than 30 million people in India till date and several have succumbed to the disease. As India continues to fight and gain stability over the existing scenario, another imminent threat has emerged as a challenge to India in the form of coronavirus disease associated mucormycosis (CAM). CAM has reached epidemic proportion during India’s second wave of Covid-19 pan-demic, with several risk factors being implicated in its etiopathogenesis.
Covid-19 is an infection caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) virus, which principally binds to the angiotensin converting enzyme 2 receptors and thus invades the respiratory epithelium. The second stage of this disease is more severe caused by aggravation of systemic inflammation and coagulopathy causing direct damage to the blood vessels. The coagulopathy seen is of complement mediated thrombotic microangiopathies leading to endothelial damage of blood vessels and microvascular thrombosis. Moreover, affected patients likewise show an overexpression of inflammatory cytokines, and impaired cell mediated immunity thus leading to increased susceptibility to fungal infections.
Covid-19 has been associated with a horde of clinical symptoms, which starts with just a dry cough and high grade fever in initial days of presentation, to furthermore include different multisystem problems such as shortness of breath, ageusia, an-osmia, diarrhoea, generalised malaise and multiple cranial nerve palsies. Along with
severe pneumonia, it is also associated with several thromboembolic events, acute cardiac injury, renal failure, systemic vasculitis and several opportunistic infec-tions [1-3]. Early identification of these high morbidity conditions is crucial for optimal treatment.
Mucormycosis (the so called black fungus) is a rare, life threatening angioinvasive infection caused by the fungus of the order Mucorales that typically affects immunocompromised individuals. It is found to be fatal in 50 to 80% of cases as it rapidly progresses through the stages of rhinomaxillary, rhino-orbital and rhino-orbito-cerebral mucormycosis (ROCM). Early diagnosis and immediate surgical intervention along with institution of appropriate antifungal therapy saves both sight and life of the patient. The Indian Council of Medical Research released guidelines for the screening, diagnosis, and management of mu-cormycosis in patients with Covid-19. The most recognised causes ascribed to the rise of mucormycosis in Covid-19 patients are uncontrolled diabetes mellitus, acute respiratory distress syndrome (ARDS), those receiving broad-spectrum antibiotics, longer stay of critically ill patients in intensive care units (ICU) especially those who required supportive ventilation and ex-cessive use of corticosteroids for immunosuppression. In the past 3 months, we have seen an immense increase in the num-bers of cases of CAM at our nodal centre. The high incidence of diabetes in our Indian population alongside with excessive use of corticosteroids as a part of treatment for Covid-19 could also be a probability for increased numbers. Coagulopathy leading to several peripheral microthrombi, microangiopathy from diabetes mellitus in addition to immunosuppression from cortico-steroids all could have been a cause in providing an ideal host for the fungus to grow. The main objective of this study was to assess the possible epidemiological factors connected to CAM and furthermore to recognise the role of vaccination in prevent-ing the progression of mucormycosis.
Materials and Methods
A retrospective observational study was conducted at our tertiary care nodal centre in India for the treatment of CAM between April 2021 and June 2021. This study included 300 patients with past history of recently being treated for Covid-19 infection and who presented to our department with symptoms and signs of ROCM. Patients were characterized as recovered from Covid-19 if they were tested negative on a repeat RT-PCR (reverse transcriptase polymerase chain reaction) or if fourteen days had elapsed since the diagnosis.
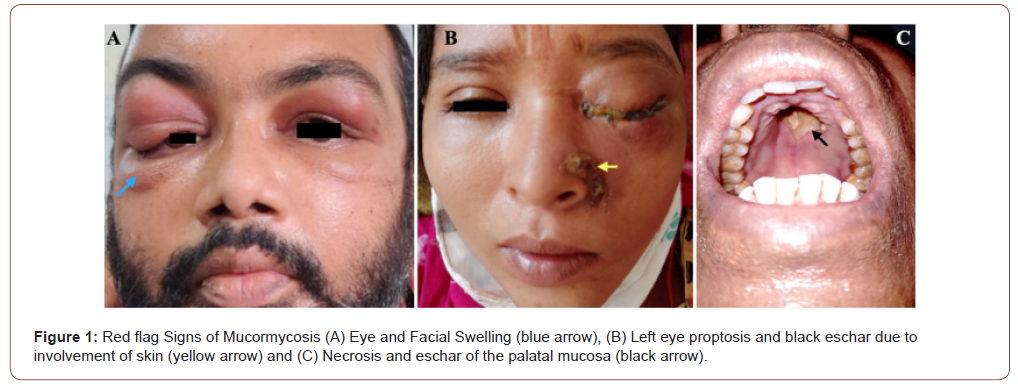
The patients who presented with one or more of the following symptoms and signs of facial pain, headache, jaw pain, necrosis of the palatal bone or mucosa, eye pain, proptosis and visual disturbances (Figure 1). suspicious of ROCM were all included in the study.
Patients were also assessed for the following history before deciding the treatment protocol:
1. History of Covid-19 infection,
2. Diabetes status of the patient (pre-existing or newly diagnosed),
3. History of steroid use during Covid-19 infection,
4. History of use of antiviral drug remdesivir, and
5. History of receiving vaccination for Covid-19.
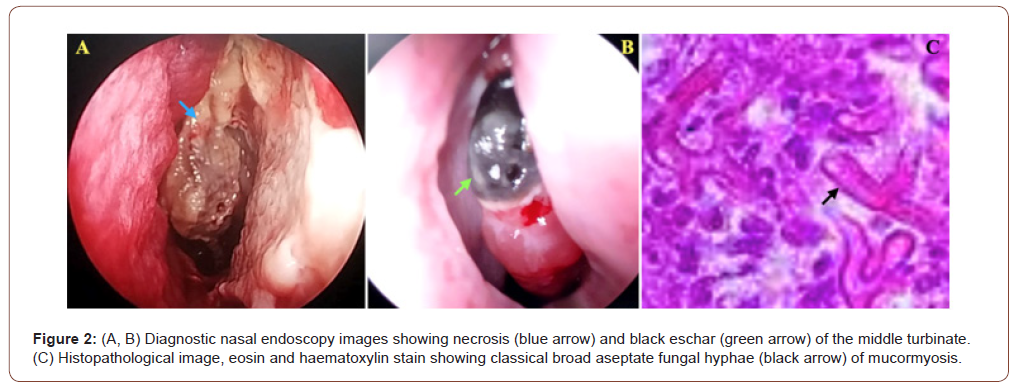
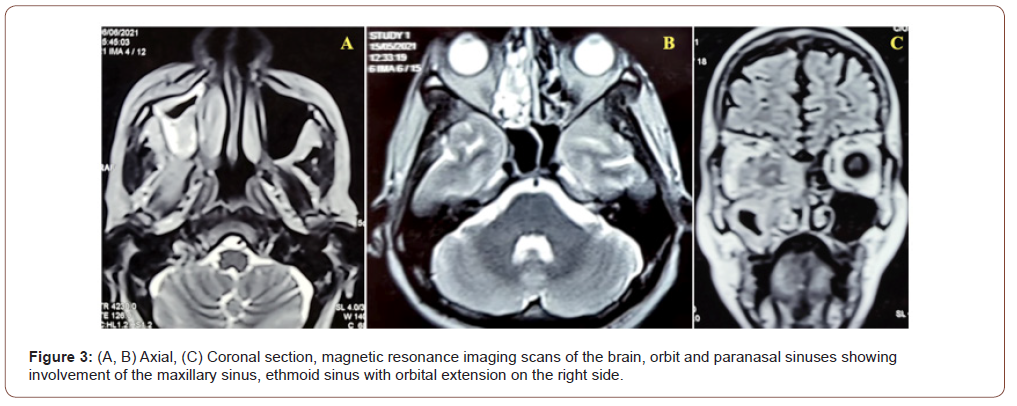
Patients with a history of radiotherapy, chemotherapy, osteoradionecrosis of the jaw, granulocytopenic patients or those on other immunomodulator drugs were excluded from the study. Patient with non Covid-19 associated ROCM were also excluded from the study. Aside from ascertaining the current Covid-19 status with RT-PCR test, routine blood investigations and high resolution com-puted tomography of the chest were done for all the patients. Diagnostic nasal endoscopy was performed to look for signs of invasive fungal sinusitis (Figure 2). Magnetic resonance imaging (MRI) of the paranasal sinuses (PNS) including orbits and brain were performed for all cases (Figure 3). Patients were taken up for surgical exploration and debridement, under endo-scopic guidance and the infected tissue was sent for microbiological and histopathological examination (HPE) to determine and confirm the presence of fungal hyphae (Figure 2). The surgical intervention varied from a simple surgical debridement to maxillectomy (partial/subtotal/total) to orbital exenteration depending on the extent of disease. Depending on the type of fun-gal organism, liposomal amphotericin therapy was instituted at 5mg/kg for mucormycosis. Later at the time of discharge pa-tients were started on oral posaconazole 300mg every 8th hourly on the first day and then continued at once daily dosage. Due to high possibility of nephrotoxicity and electrolyte disturbances due to liposomal amphotericin B, daily renal function tests and serum electrolytes were performed, monitored and managed appropriately. The patients were followed up after discharge regularly at weekly intervals and were taken up for further surgical debridement if any suspicious lesions were noted.
Statistical Methods
Data were collected on patient’s demographics, co-morbidities, history in regards to management with use of corticosteriods, antiviral drugs, oxygen administration both invasive and non invasive during Covid-19 infection and vaccination status of receiving one, two or no doses at all. Data were summarized using mean ± SD (standard deviation) for continuous variables and frequency along with percentage for categorical variables. A logistic regression analysis method was used to determine the factors influencing CAM. Statistical analysis software STATA (StataCorp LLC, 4905 Lakeway Drive College Station, Texas) v.11.2 was used for data analysis.
Results
Among the 300 patients who were included in the study, 227 (75.6%) were males and 73 (24.33%) were females, with ratio between males to females to be 3.1:1. The age of the patients ranged from 18 years to 80 years with a mean age of 47.05 +/- 10.7 years.
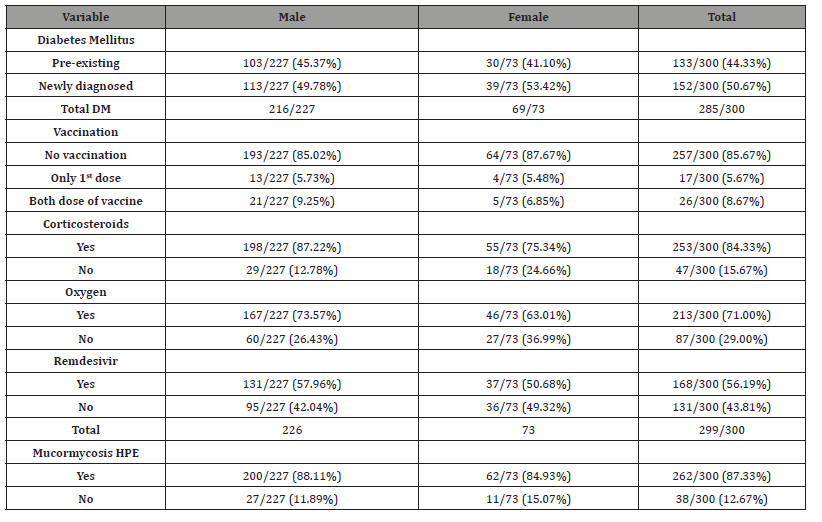
(Table 1) summarises the distribution of factors associated with CAM. Out of the 300 patients, majority 285 (95%) patients were either newly diagnosed or pre-existing diabetics. 213 (71%), 253 (84.33%), and 168 (56.19 %) patients received oxygen support, corticosteriods, and antiviral drug remdesivir respectively during management of Covid-19 infection. Forty-three (43) out of 300 patients received vaccination either just the 1st dose or both the doses at the time of presentation.
All 300 patients presented with either symptoms of sinusitis, facial pain or swelling, headache, jaw pain, eye pain and visual disturbances. Headache was noted in 208 (69.33%), eye pain in 221 (73.67%), facial pain in 253 (84.33%), jaw pain in 56 (18.67%), visual disturbances in 100 (33.33%) of the patients (Figure 4). All patients underwent immediate surgical manage-ment and the tissue was sent for HPE. HPE confirmed mucormycosis was seen in 262 (87.33%) patients, aspergillosis in 11 patient, mixed infection in 4 patients and rest others showed features of chronic sinusitis.
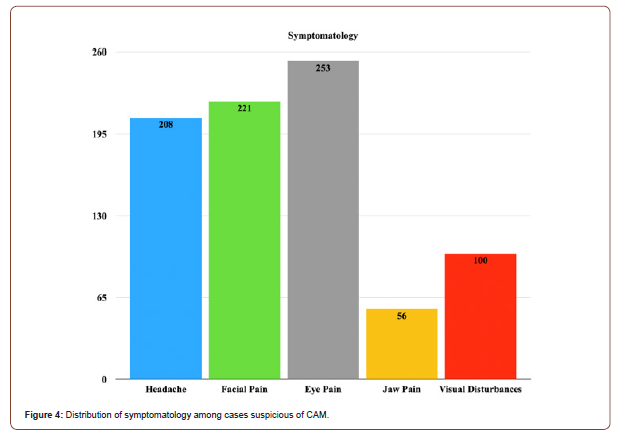
Table 1: Distribution of clinical and epidemiological factors associated with CAM in patients (n=300) presenting at tertiary care nodal center.
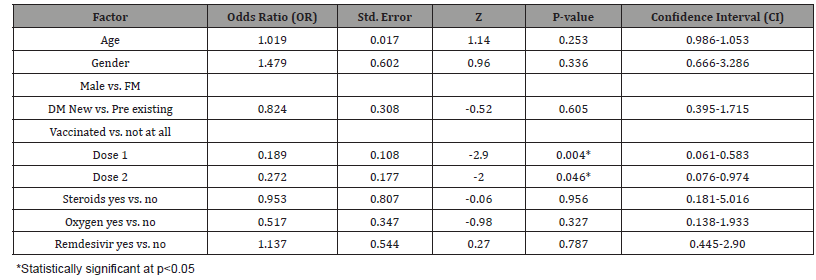
A logistic regression model analysis of data (Table 2) shows receiving one dose of Covid-19 vaccination is protective against CAM (Odds Ratio 0.189, Confidence Interval 0.061-0.583, p-value 0.004). However, receiving two doses of vaccination (Odds Ratio 0.272, Confidence Interval 0.076-0.974, p-value 0.048) is protective but with borderline statistical significance. All oth-er factors included in the model were not significant. Upon further analysis of vaccination variable alone in a parsimonious model retained statistical significance (Odds Ratio 0.206, CI: 0.070-0.604, p-value 0.004) for patients receiving one dose of vaccination, while the protection faded to not significant for those receiving two doses of vaccination.
Table 2: Logistic regression analysis of clinical and epidemiological factors associated with CAM.
Discussion
Mucormycosis is a rare, opportunistic, life threatening, angioinvasive fungal infection that affects immunocompromised indi-viduals, predisposed by diabetes mellitus, corticosteroids, immunosuppressive therapy, immunodeficiency syndromes, haematological malignancies, neutropenia and organ transplantation [4]. This pathogenic fungus is omnipresent, seen occurring naturally in the environment. It can affect the nose, PNS, orbit, central nervous system, lung, gastrointestinal tract, skin, jaw bones, heart, kidney, and the mediastinum [5]. The inhaled spores of the fungi get inoculated into the nose and nasopharynx, lead-ing to tissue invasion, thrombosis, and necrosis. This necrosis spreads from the nose, to the PNS, to the orbit, cavernous sinus and then to the intracranial cavity.
ROCM is the most common presentation and contributes to about two-thirds of all cases of mucormycosis. The worldwide prevalence before the pandemic has been estimated to be 0.005- 1.7 per million population. Chakrabarti et al. have estimated a prevalence of 0.14 per 1000 cases of diabetics in India, which is about 80 times the prevalence of mucormycosis in developed countries [6]. India also occupies the second position in the world as far as the number of diabetics is concerned. This surge in the number of cases of mucormycosis during the second wave could be due the hypoxic environment with high glucose levels, high levels of ferritin, and attenuated phagocytic activity of the leukocytes due to immunosuppression by the virus itself and the corticosteroids used in the management during the second wave of Covid-19 infection. This hypoxic environment is pro-foundly favourable for the fungal spores to germinate and proliferate. Prolonged hospital stay also increases the possibility of nosocomial infection, increased use of corticosteroids and antiviral drugs like remdesivir, and associated co-morbidities are other factors attributed to the increasing incidence of CAM. This study was done with the goal of improving the knowledge about CAM in order to improve the management and outcome.
In the previous reported literature of CAM there was a male predilection (79%) [7]. The median age of CAM in Indian population has been reported to be 45-50.7 years [8-10]. In our study the demographic profile was consistent with previous literature with a mean age of 47.05 years and 227 (75.6%) male patients with male to female ratio of 3.1:1.
CAM occurs both concomitantly with Covid-19 as well as postrecovery. The median time for diagnosis of mucormycosis was 14 days for those who developed signs of mucormycosis after the diagnosis of Covid-19 similar to published literature [11]. All the patients in our study presented with signs of ROCM following recovery from Covid -19 in our series. Delayed ROCM was also noted in a couple of cases, with the greatest length to be 45 days in our study. Literature has shown delayed CAM upto three months post Covid-19 infection [12] and this makes follow-up of Covid-19 patients necessary for a period of three months after recovery.
The etiology of CAM appears to be multifactorial. The possible epidemiological factors for CAM could be pre-existing or new-ly diagnosed Covid-19 related hyperglycemia, impaired cell mediated immunity, necrosis of the nasal mucosa, hypoxia due to Covid 19 infection, use of systemic corticosteroids, and nosocomial infections in hospitalized patients.
In our present study 213 (71%) patients received oxygen (invasive or noninvasive) during Covid-19 infection. Our study showed similar incidence to other studies conducted in India which was around 77% among 235 patients. Remdesivir, a anti-viral drug has been authorized for emergency use among Covid -19 patients. In our series, 168 (56.19 %) of the patients re-ceived remdesivir during the Covid -19 infection and may not have a played a significant role in increasing the risk of ROCM. Corticosteroids have been maligned for their role in immunosuppression and thus increasing the susceptibility to mu-cormycosis. A cumulative dose greater than 600 mg for prednisolone and 2-7gm of methylprednisolone has been found to predispose immunocompromised patients to mucormycosis [13]. Prolonged use of more than 3 weeks of high dose systemic cor-ticosteroid has also been implicated as a risk factor for mucormycosis in non Covid-19 patients. According to the previous published literature, 76.3% of the patients with Covid-19 associated ROCM gave history of use of systemic corticosteroids [14]. and this fraction was much higher about 88% among Indian population. Our data revealed that systemic corticosteroids had been used in 253 (84.33%) of the patients which was similar to published literature [15].
Diabetes Mellitus (DM) has been identified as an independent risk factor for mucormycosis [15]. The SARS Covid-19 virus is said to damage the pancreatic islet cells producing new onset DM or worsening of the already existing DM. The cytokine storm indirectly fuels this by resulting in insulin resistance. Corticosteroids also precipitate hyperglycemia progressing to diabetic ketoacidosis. Hyperglycemia causes glycosylation of both transferrin and ferrtin, thus reducing the ability of transfer-rin to chelate iron. This low ph acidic environment presents an additive effect causing an overall increase in free iron levels, providing a fertile environment for the fungus to grow and thrive [12, 15]. In Indian patients with Covid-19, DM was seen in 11-23% of the hospitalized patients. New onset DM was seen in 20.6% of patients with mild to moderate Covid-19. According to previous literature, during the pre covid era the risk of mucormycosis is said to be 7.5 times higher in diabetics than the gen-eral population [16].
In a large series of mucormycosis cases from India in the pre- Covid-19 era, 74% of the patients were diabetics [17]. A study done by John et al, in a series of 41 cases of Covid-19-associated ROCM, 93% were diabetics [14]. Our data showed similar results, ma-jority 287 (95.6%) patients were diabetic patients, of which 133 (44.33%) were pre-existing diabetics and 152 (50.67%) were newly diagnosed diabetics. ROCM is not known to affect healthy individuals except in rare cases. This is important because in patients presenting with signs and symptoms of ROCM in the background of Covid-19, one should still investigate thoroughly and have a high index of suspicion even in the absence of an underlying comorbidity.
ROCM shows charachteristic red flag warning signs and symptoms which allows early diagnosis as compared to mucormycosis at other anatomical sites. The most common symptoms reported in our study were headache (69.33%), eye pain (73.67%), facial pain (84.33%), jaw pain (18.67%) and visual disturbances (33.33%).
Mucormycosis is highly angioinvasive and thus leads to extensive necrosis of tissues, however bone erosion is not a typical finding, and thus CT scan may fail in detecting early disease. In our series, contrast-enhanced MRI of the paranasal sinuses, orbit and brain was the preferred imaging modality of choice. It detects early involvement of soft tissues especially in cases with extensive orbital and intracranial spread. Diagnostic nasal endoscopy allows for quick inspection to look for a black es-char and thus allowing to take biopsy for microbiological and HPE. The management of mucormycosis essentially involves control of hyperglycemia or any other risk factor, optimal surgical debridement, and medical management with antifungal agents. Previous published literature showed that that survival was 70% when treated with both amphotericin and surgical debridement, 61% with amphotericin deoxycholate, 57% with surgery alone and only 3% in patients who underwent no treatment [18]. Amphotericin B is the antifungal drug of choice for mucormycosis. It has been used in 88% of the patients of CAM. Even in our series, almost all patients had received liposomal amphotericin B. The liposomal form is preferred since it is less nephrotoxic and, therefore, higher doses may be given for a prolonged duration. In patients with compromised renal functions, posaconazole and isavuconazole have been found to be effective alternatives, but amphotericin B remains the treatment of choice. A study from India has shown posaconazole to be highly effective as salvage therapy for ROCM with complete resolu-tion in 67% of the patients [19]. Intraorbital amphotericin B deoxycholate injection in a concentration of 3.5 mg/mL has shown to be effective for life and eye salvage in certain case reports. Endoscopic surgical debridement of paranasal sinuses was per-formed as a primary management in all of the cases in our series. Simultaneous PNS debridement with orbital exenteration or intraorbital amphotericin injection or matxillectomy was performed in cases based on the extent of disease. Orbital exentera-tion is conventionally done in cases with no visual potential, with diffuse orbital involvement, but with the disease limited to the orbit without or minimal extension to the cavernous sinus. CAM is a rapidly progressive disease, with a high 30-90% mortality rate in cases with intracranial involvement [6, 7, 11].
For cases associated with COVID-19, the overall mortality has been estimated to be 31%. Vaccination has always played a ma-jor role in eradicating communicable diseases. So was also the case in Covid-19 infection, in which vaccination played a key role to break the chain of transmission and also in reducing severity of the disease. Prior vaccination results in less severe disease against subsequent infection thus preventing coagulopathy and further impairment of humoral and cell mediated im-munity. The patients in our study had either received Covishield which is a recombinant, replication deficient chimpanzee adenovirus vector encoding the SARS-CoV-2 Spike glycoprotein vaccine manufactured by Serum Institute in India or Covaxin which is a whole virion inactivated vaccine developed by Bharat Biotech India. Similar results were observed in our study that showed patients who received vaccination were slightly more protected from developing mucormycosis. Thus encouraging government to promote several awareness campaigns regarding benefits of vaccination inorder to prevent serious life threat-ening sequelae of Covid-19 infection [20].
Limitations
The follow up of CAM patients is limited and majority are still under active treatment. Very few patients of the study population were vaccinated. Information regarding vaccination being protective against developing CAM is still very minimal and more number of vaccinated patients should be included in the study to come to any firm conclusion.
Conclusion
CAM predominantly affects middle aged males with majority of the patients developing onset of ROCM symptoms between day 10 and day 14 from the diagnosis of Covid-19. Post Covid-19 follow-up for a period of three months is recommended, as delayed presentation can occur up to three months. The red flag signs and symptoms of severe headache, facial pain, eye pain, jaw pain and visual disturbances should be recognized promptly, followed by a confirmatory diagnosis by diagnostic nasal endoscopy and HPE. Contrast-enhanced MRI is the imaging modality of choice. Liposomal amphotericin B is the drug of choice for treatment of CAM. PNS debridement should be radical and may combined with orbital exenteration/maxillectomy based on the extent of disease. Patients with CNS involvement have better prognosis when PNS debridement and orbital exenteration along with antifungal therapy are included in their management. A longer follow-up is essential to determine the prognosis conclusively, but the analysis of our data does provide some insightful information that may help plan the management of CAM. A large data should be collected regarding the vaccination status of the patients and the confirmation of CAM, to come to a firm conclusion regarding its protective role from the deadly black fungus.
Acknowledgement
The authors would like to gratefully acknowledge the medical postgraduates and consultants who con-tributed in collection of data for this article. We are also grateful to all the patients who volunteered to participate in this study.
Funding
No funding was required to conduct the study.
Competing Interests
None declared.
References
- Giustino G, Pinney SP, Lala A, Reddy VY, Johnston-Cox HA (2020) Coronavirus and cardiovascular disease, myocar-dial injury, and arrhythmia: JACC focus seminar. J Am Coll Cardiol 76(17): 2011-2023.
- Diao B, Wang C, Tan Y, Chen X, Liu Y (2020) Reduction and functional exhaustion of T cells in patients with corona-virus disease 2019 (COVID-19). Front Immunol 11: 827.
- Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LF (2020) The trinity of COVID-19: immunity, inflammation and intervention.
- Nat Rev Immunol 20(6): 363-374.
- Hirabayashi KE, Idowu OO, Kalin-Hajdu E, Oldenburg CE, Brodie FL (2019) Invasive fungal sinusitis: risk factors for visual acuity outcomes and mortality. Ophthalmic Plast Reconstr Surg 35(6): 535-542.
- Sugar AM (1992) Mucormycosis. Clinical infectious diseases 14(Supplement_1): S126-S129.
- Prakash H, Chakrabarti A (2021) Epidemiology of Mucormycosis in India. Microorganisms 9: 523.
- Singh AK, Singh R, Joshi SR, Misra A (2021) Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabetes Metab Syndr 15(4): 102146.
- Kayina CA, Haritha D, Soni L, Behera S, Nair PR (2020) Epidemiological & clinical characteristics & early outcome of COVID-19 patients in a tertiary care teaching hospital in India: A preliminary analysis. Indian J Med Res 152(1-2): 100-104.
- Mohan A, Tiwari P, Bhatnagar S, Patel A, Maurya A et al (2020) Clinico-demographic profile & hospital outcomes of CO-VID-19 patients admitted at a tertiary care centre in north India. Indian J Med Res 152(1-2): 61-69.
- Marimuthu Y, Kunnavil R, Anil NS, Nagaraja SB, Satyanarayana N (2021) Clinical profile and risk factors for mortality among COVID-19 inpatients at a tertiary care centre in Bengaluru, India. Monaldi Arch Chest Dis 91(3).
- Hoenigl M, Seidel D, Carvalho A, Rudramurthy SM, Arastehfar A (2021) The Emergence of COVID-19 Associated Mucormycosis: Analysis of Cases From 18 Countries.
- Sen M, Honavar SG, Bansal R, Sengupta S, Rao R, Kim U (2021) Epidemiology, clinical profile, management, and out-come of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India-Collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC), Report 1. Indian Journal of Ophthalmology 69(7): 1670-1692.
- Lionakis MS, Kontoyiannis DP (2003) Glucocorticoids and invasive fungal infections. Lancet 362(9398): 1828-1838.
- John TM, Jacob CN, Kontoyiannis DP (2021) When uncontrolled diabetes mellitus and severe COVID-19 converge: the perfect storm for mucormycosis. J Fungi (Basel) 7(4): 298.
- Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA (2019) The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clinical Microbiology and Infection 25(1): 26-34.
- Bala K, Chander J, Handa U, Punia RS, Attri AK (2015) A prospective study of mucormycosis in north India: experience from a tertiary care hospital. Med Mycol 53(3): 248-257.
- Patel A, Kaur H, Xess I, Michael JS, Savio J (2020) A multicentre observational study on the epidemiology, risk fac-tors, management and outcomes of mucormycosis in India. Clin Microbiol Infect 26(7): 944-e949.
- Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA (2005) Epidemiology and outcome of zygomyco-sis: a review of 929 reported cases. Clin Infect Dis 41(5): 634-653.
- Manesh A, John AO, Mathew B, Varghese L, Rupa V (2016) An emerging therapeutic option for invasive rhino‐orbito‐cerebral mucormycosis. Mycoses 59(12): 765-772.
-
Mounika Reddy Y, Shankar T, Manish Kumar, Sreenivas K, Subramanyam Darbha. A Clinical Epidemiological Study of Patients with Coronavirus Disease Associated Mucormycosis Treated at A Tertiary Care Nodal Centre. On J Otolaryngol & Rhinol. 5(2): 2022. OJOR. MS.ID.000609.
-
Coronavirus, Mucormycosis, Sinusitis, Fungal infections, Inflammatory cytokines, Rhinomaxillary, Corticosteriods, Facial pain, Headache, Intracranial cavity.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






