 Case Report
Case Report
Transient Global Amnesia Case Report
Benjamin Shao1* and David Young MD2
1Nova Southeastern University, USA
2Emergency Medicine, St. Vincent’s Medical Center-Bridgeport, CT, USA
Benjamin Shao, Nova Southeastern University, USA.
Received Date:February 23, 2024; Published Date:March 12, 2024
Abstract
Transient Global Amnesia (TGA) is a neurological phenomenon causing an individual to experience a benign, temporary loss in memory that is usually anterograde but can also be retrograde in nature. This case report analyzes the presentation, etiology, treatment, and future management of a patient that presented to the emergency department with sudden onset confusion and memory impairment. After ruling out metabolic or structural causes through labs and imaging, the diagnosis of TGA was made and appropriate care was carried out. This case report’s purpose is to showcase the proper criteria to diagnose a patient with TGA as well as highlight the crucial differential diagnoses that ought to be excluded, and how they were excluded. Finally, the history and rarity of TGA, the known and the unknown factors associated with the illness, future prognoses, and treatment options to consider will be discussed.
Introduction
TGA is defined as an acute neurological disorder that results in transient memory loss that is usually anterograde or partially retrograde (Nehring et al., 2023) [1].
https://www.ncbi.nlm.nih.gov/books/NBK442001/
It is abrupt in onset, usually lasting between 1-24 hours. Etiology is currently unknown at this point, but Nehring et al. (2023) have suggested that it is thought to be due to intracranial venous stasis leading to brain ischemia and poor memory. Furthermore, they also found that certain triggers, such as stress and physical exercise, can also induce onset. Patients often present with a sudden loss of memory and orientation to time and place and may even have trouble forming new memories after the incident. Most patients who experience TGA are over the age of 50. Worldwide, its incidence is approximately 2.9-10/100,000 (Harrison & Williams, 2007) [2].
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2658295/
Initial management requires no further diagnostic procedures, as it is often a diagnosis of exclusion with no further treatment nec essary. This case report examines a rare case of TGA that presented at an emergency department in an urban hospital.
Case Presentation
A 64-year-old female arrived by ambulance and presented to the ED with a chief complaint of confusion. The patient stated that she was “outside walking her dogs” in the afternoon, and when she arrived back home, she had no recollection of what had happened or what she had done. Her husband who was with her reported that she began experiencing shaking chills at the time of the episode with reported vomiting and stroke-like symptoms but no associated fever. Prior to this episode, the patient was operating with her normal baseline mental status and had never experienced a similar episode. Upon arrival, the patient did not present with any facial asymmetry and was otherwise nonfocal neurologically. The patient’s lapses of memory appeared to be more retrograde in fashion. No pertinent past medical history, past surgical history, or family history was determined. The patient did not have any history of diabetes or prior metabolic encephalopathies. Social history only revealed 4 standard drinks of wine per week, well within normal range.
Upon physical exam, the patient’s vitals were within normal limits. Her blood pressure was 125/76 on her right arm lying down. Pulse was 89 bpm, 98.4 F, 20 RR, and 98% on room air. The patient was not cachexic with no signs of wasting. She did not present with any signs of trauma or head strike, nor did she complain of any headache, migraines, abnormal gait, or pains. She was alert and oriented to person at the time of initial encounter, although she could not remember why she was brought to the hospital or what the date was. On review of systems, the patient denied any weakness, numbness, tenderness, shortness of breath, nausea/diarrhea, vision loss, trouble with urination, behavioral/psychological concerns, or any other physical complaints.
Basic laboratory tests were ordered on time of arrival. Complete blood count (CBC) and comprehensive metabolic panel (CMP), lactic acid, troponin, and blood glucose were all unremarkable and within normal limits. A blood alcohol and urine tox screen were also collected and were completely negative. Urinalysis revealed no signs of infection, hematuria, or proteinuria. Flu/Covid/RSV tests all came back negative, and ECG was unremarkable. The patient was started on a normal saline (NS) sodium chloride 0.9% bolus at 1,000mL/hr IV. A CT Angiogram (CTA) Head and Neck was completed, showing no abnormalities (Figure 1). A Chest X-ray was also completed and was shown to be unremarkable (Figure 2).


On final disposition, the patient was alert and oriented to time, place, and person. She stated that she could not remember what had happened earlier, confirming the retrograde lapse in memory that she experienced earlier. The patient was informed of the diagnosis of TGA, the co-factors that could trigger an episode, and future management.
Discussion
Early reports of TGA were first published in 1956. Researchers described an acute, transient event that usually occurred in middle- aged/elderly people and was characterized by the abrupt onset of anterograde amnesia coupled with no neurological deficits (Quinette et al., 2006) [3]. (https://academic.oup.com/brain/article/ 129/7/1640/302781?login=true).
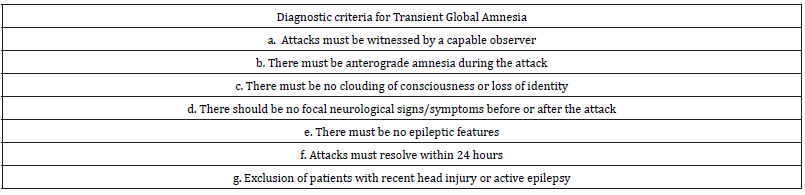
In 1990, Hodges and Warlow established diagnosis criteria
for TGA that are currently followed today. Together, they listed
out 7 diagnostic criteria that a patient must satisfy (Hodges &
Warlow, 1990) [4]. (https://www.ncbi.nlm.nih.gov/pmc/articles/
PMC488242/):
a. Attacks must be witnessed by a capable observer
b. There must be anterograde amnesia during the attack
c. There must be no clouding of consciousness or loss of identity
d. There should be no focal neurological signs/symptoms before
or after the attack
e. There must be no epileptic features
f. Attacks must resolve within 24 hours
g. Exclusion of patients with recent head injury or active epilepsy
Table 1:
The patient included in this case report presented to the ER with many classic symptoms that satisfied the TGA criteria. Her age at 64 fell around the seventh decade of life, which is typically seen in patients with TGA (Miller & Butler, 2022) [5] (https://pn.bmj.com/ content/22/3/201.long). The patient presented with no abnormal laboratory values or abnormal toxicology screens, thus eliminating other secondary causes of amnesia (Huang, 2023) [6]. Additionally, previous studies have demonstrated an increased incidence in patients suffering from TGA after experiencing high-stress situations (Werner et al., 2020; Griebe et al., 2019) [7, 8].
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7492094/) (https://www.sciencedirect.com/science/article/pii/ S0306453018306395?via%3Dihub).
Before final disposition, the patient did admit that she had recently been traveling for various job conferences and was feeling worn down due to occupational stress. Past studies have also revealed differences between the male and female sex in terms of the incidence and development of TGA (Rogalewski et al., 2022) [9]. Furthermore, the researchers discovered a stronger female predominance while also revealing that more emotional triggers were seen in female patients, but more physiologic triggers and chronic hypertension were seen in male patients.
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9571788/). The patient’s matching symptoms for TGA criteria, coupled with her recent stress and the ruling out of other metabolic/structural encephalopathies, lead us to conclude TGA as the final diagnosis.
Currently, the etiology behind TGA is still relatively unknown. The most prominent ideas suggest that the mechanism may be related to migraines, hypoxia, ischemia, venous flow abnormalities, seizures, and psychological/stress-related factors (Huang, 2023) [6].
(https://www.merckmanuals.com/professional/neurologic- disorders/function-and-dysfunction-of-the-cerebral-lobes/ transient-global-amnesia). It is that last point, stress-related factors, that have recently been heavily focused on as a likely etiology behind an increased risk for TGA. Researchers have suggested that the neurons found in the cornu ammonis (CA1) area of the hippocampus are extremely sensitive to stress (Spiegel et al., 2017) [10].
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5661450/).
Stress-related cell damage within this area of the hippocampus
leads to a downward pathophysiological cascade, resulting in poor
memory functioning. Events that can trigger a TGA attack include
but are not limited to:
• Sudden immersion in cold/hot water
• Physical exertion
• Emotional/psychological stress
• Pain
• Medical procedures
• Sexual intercourse
• Valsalva maneuvers.
The aforementioned reasons make it crucial to obtain a detailed patient history and identify any factors that could potentially cause TGA. However, some TGA attacks can occur without any identifiable event, which is ultimately why the etiology behind TGA remains a mystery.
Symptoms related to TGA can also present in other conditions similar to TGA. One common differential diagnosis similar to TGA that is imperative to be ruled out is acute amnesia secondary to an ischemic stroke in the hippocampus. Physicians can distinguish hippocampus ischemia and TGA through careful physical examination of any neurological deficits, such as vision loss, weakness, or hemisensory deficits. Researchers have found that ischemic strokes involving the hippocampus also present with a co-occurrence of other neurological symptoms (Miller & Butler, 2022) [5]. Acute confusion state is another condition that can demonstrate transient amnesia similar to TGA. Oftentimes, an acute confusion state is secondary to metabolic abnormalities or toxin mediated. Therefore, physicians should differentiate by obtaining laboratory results and performing toxicology screens, while also performing a thorough neurological exam to see if patients can sustain coherent streams of thought (Brown, 1997) [11].
(https://www.sciencedirect.com/science/article/pii/ S0196064497700131#aep-section-id10). Psychogenic amnesia is another differential that presents similarly to TGA. However, this condition is often seen in younger populations and typically will present with personality changes unlike TGA (Brown, 1997) [11]. Clinicians must address other avenues that can cause transient amnesia, as these conditions all present similarly and must be ruled out before concluding TGA.
The treatment for TGA currently is to provide general supportive measures due to its unclear etiology. Given its temporary, self-limiting condition, no specific treatments are indicated for a patient experiencing TGA unless there are secondary underlying etiologies (i.e. hypertension, trauma, metabolic abnormalities) (Hsieh et al., 2020) [12].
(https://www.sciencedirect.com/science/article/pii/ S0303846720304297). If that is the case, specific treatment guidelines related to that etiology needs to be followed. If there are no underlying conditions, then researchers have found that no specific treatments are necessary and to only provide supportive measures such as pain management, fluids, etc.
The prognosis of TGA is relatively good, as Hodges and Warlow (1990) reported that symptoms were only temporary and lasted <24 hours (repeat https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC488242/). Furthermore, only 3-24% of patients who previously suffered from a TGA attack experienced recurrence of symptoms (Miller et al., 1987) [13]. (https://pubmed.ncbi.nlm. nih.gov/3574671/). Studies have also reported no increased risk of future strokes or severe cerebrovascular events (Arena et al., 2017) [14]. (https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC5682935/).
Conclusion
TGA remains to be a rare, mysterious diagnosis often as a result through diagnosis of exclusion. This benign condition, known to cause temporary anterograde and retrograde memory loss, presents with vague symptoms that are also commonly seen in other types of etiologies. Therefore, it is imperative for clinicians to do a proper work-up to rule out other neurological/metabolic conditions beforehand. By following the diagnostic criteria and performing the necessary imaging/lab studies, clinicians can safely and effectively manage TGA.
Acknowledgement
None.
Conflict of Interest
None.
References
- Nehring SM, Spurling BC, Kumar A: Transient Global Amnesia. [Updated 2023 Jul 17]. In. StatPearls [Internet, Treasure Island (FL): StatPearls Publishing; 2024.
- Harrison M, Williams M (2007) The diagnosis and management of transient global amnesia in the emergency department. Emerg Med J 24: 444-445.
- Peggy Quinette, Bérengère Guillery Girard, Jacques Dayan, Vincent de la Sayette, et al. (2006) What does transient global amnesia really mean? Review of the literature and thorough study of 142 cases. Brain 129: 1640-1658.
- Hodges JR, Warlow CP (1990) Syndromes of transient amnesia: towards a classification. A study of 153 cases. J Neurol Neurosurg Psychiatry 53: 834-843.
- Miller TD, Butler CR (2022) Acute-onset amnesia: transient global amnesia and other causes. Practical Neurology. 22: 201-208.
- Transient Global Amnesia (2023)
- Werner R, Keller M, Woehrle JC (2020) Increased incidence of transient global amnesia during the Covid-19 crisis?. Neurol Res Pract 26.
- Martin Griebe, Anne Ebert, Frauke Nees, Katharina Katic, Benjamin Gerber (2019) Enhanced cortisol secretion in acute transient global amnesia. Psychoneuroendocrinology 99: 72-79.
- Rogalewski A, Beyer A, Friedrich A (2022) Transient Global Amnesia (TGA): Sex-Specific Differences in Blood Pressure and Cerebral Microangiopathy in Patients with TGA. J Clin Med 30: 5803.
- Spiegel DR, Smith J, Wade RR (2017) Transient global amnesia: current perspectives. Neuropsychiatr Dis Treat 24: 2691-2703.
- Jeremy Brown (1997) ED Evaluation of Transient Global Amnesia. Ann of Emerg Med 30: 522-526.
- Sun Wung Hsieh, Yuan Han Yang, Bo Lin Ho, Shan Tzu Yang, Chun Hung Chen (2020) The long-term risk of epilepsy after transient global amnesia: A population-based cohort study. Clin Neurol Neurosurg 197: 106086
- Miller JW, Petersen RC, Metter EJ, Millikan CH, Yanagihara T (1987) Transient global amnesia: clinical characteristics and prognosis. Neurology 37: 733-737.
- Arena JE, Brown RD, Mandrekar J, Rabinstein AA (2017) Long-Term Outcome in Patients With Transient Global Amnesia: A Population-Based Study. Mayo Clin Proc 92: 399-405.
-
Benjamin Shao* and David Young MD. Transient Global Amnesia Case Report. On J Otolaryngol & Rhinol. 6(5): 2024. OJOR.MS.ID.000646.
-
Neurological disorder, TGA, Retrograde memory loss, Transient amnesia, Toxicology screens, Neurological deficits, Vision loss, Psychological stress, Stress related factors
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






