 Case Report
Case Report
Squamous Cell Carcinoma of the External Auditory Canal: A Sternocleidomastoid Flap Reconstruction
Klecius Leite Fernandes*
Adjunct Professor and Coordinator of the Discipline of Head and Neck Surgery at UFPB. Institution: Lauro Vanderley University Hospital. João Pessoa/PB-Brazil
Klecius Leite Fernandes*, Adjunct Professor and Coordinator of the Discipline of Head and Neck Surgery at UFPB. Institution: Lauro Vanderley University Hospital. João Pessoa/PB-Brazil.
Received Date: August 02, 2022; Published Date: October 03, 2022
Abstract
Introduction: Malignancies of the external auditory canal are rare, representing less than 0, 2% of head and neck tumors. The main cancer of
this area is the epidermoid carcinoma, which differential diagnosis is adenocarcinoma, basal cell carcinoma and adenoid cystic carcinoma. Due to the
rarity of this condition, it has been difficult for a single institution gather enough data to acquire experience and formulate optimal staging system
and treatment strategy guidelines. Therefore, there is no consensus about the best surgery technique for these patients.
Objective: To describe a case of epidermoid carcinoma of the external auditory canal and its reconstructive surgery with sternocleidomastoid
flap.
Case report: We report a case of 59-year-old woman who presented with a 1-year history of a growing lesion on the left tragus, left ear pain,
otorrhea and local itching. The final pathologic diagnosis was epidermoid carcinoma. She had surgery treatment, and the postoperative course was
uneventful. At the 4-year and 8-month checkup after surgery, no sign of a recurrent tumor was observed.
Final comments: Thus, the present study is important because it reviews this rare pathology and its treatment, which is still a matter of
controversy and needs contribution from different institutions of new surgery techniques and treatment strategy.
Keywords: Squamous Cell Carcinoma; Ear Canal; Surgery
Introduction
Malignant neoplasms of the external auditory canal (EAC) are rare, with an incidence of 1/1,000. 000 inhabitants/year [1, 2], representing less than 0.2% of tumors head and neck [3]. Squamous cell carcinoma (SCC) is the most common cancer in this region [3-7], having different characteristics of lesions on sun-exposed skin due to its location and pathogenesis [4]. Other neoplasms originated from in EAC are adenocarcinoma, adenoid cystic carcinoma, basal cell carcinoma, mucoepidermoid carcinoma, ceruminous carcinoma and rhabdomyosarcoma [5].
SCC has a more aggressive behavior and worse prognosis than other CAE tumors, [6] however, when discovered in early stages, it has a good survival rate in up to 100% of patients [4].
ECC squamous cell carcinomas are aggressive tumors [6], that spread primarily by direct extension [3]. Accurate assessment of the deep extent of these tumors and associated lymph node enlargement is only possible through complementary exams, such as computed tomography [3, 8]. For diagnosis definitive, a biopsy of the lesion with histopathological examination is performed.
In general, the management of these patients is based on a combination of surgical approach associated with adjuvant radiotherapy [3, 6, 9, 10]. Because EAC squamous cell carcinoma is a rare pathology, it is difficult for a single center to gather a sufficient number of cases to acquire more experience in the management of this disease and determine staging and treatment protocols [1, 2, 11, 12]. In this context, there is no consensus as to the best surgical technique to be used in these patients [1].
Thus, this study is important because it refers to this rare pathology, whose treatment has not yet been standardized, requiring the contribution of different institutions to determine new treatment modalities and surgical techniques. The main objective of this work is to report a case of squamous cell carcinoma of the external auditory canal, describe the reconstructive surgery used, and carry out a literature review on the subject.
Case Report
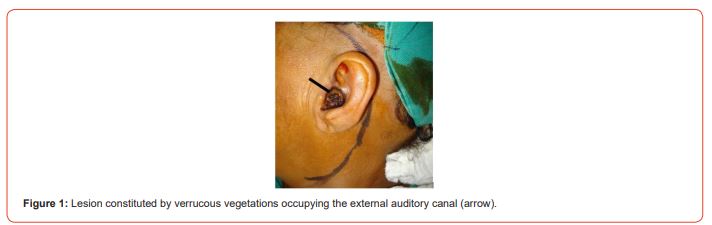
Female patient, 59 years old, farmer, white, was seen with a complaint of lesion in the posterior region of the left tragus, accompanied by otalgia, otorrhea and local pruritus. She reports that this lesion appeared about a year ago and showed progressive growth. Physical examination reveals a lesion consisting of verrucous vegetations occupying the external auditory canal (Figure 1), and absence of cervical lymphadenomegaly. She denies a history of smoking, alcoholism and otitis.
She reports that three months ago, she was clinically diagnosed with chronic otitis media by performing a computed tomography (CT) scan of the ear and mastoid. This revealed tissue formation located inside the left external auditory canal adjacent to the tympanic membrane, without signs of invasion to the middle ear or bone erosion, and presence of ceruminous plug and left external otitis.
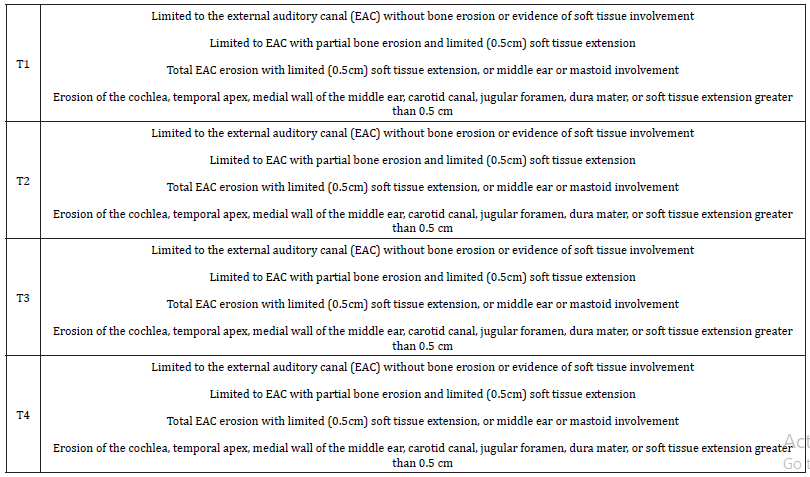
Thus, the patient was staged T1, using the modified Pittsburg system, and underwent biopsy of the lesion, which was compatible with squamous cell carcinoma.
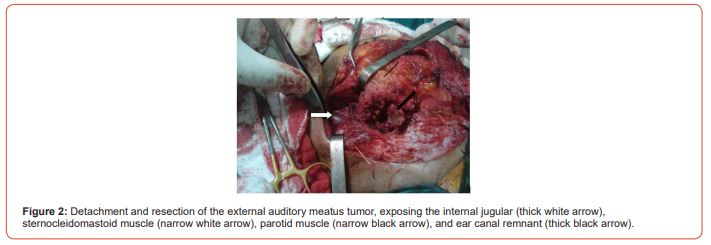
The patient underwent general anesthesia with orotracheal intubation. The surgical procedure began with a Fish incision, an arcuate retroauricular incision extending from the temporal line superiorly to the cervical region just below the angle of the mandible (Figure 1). The flap was detached together with the external ear until close to the labial commissure, requiring an intra-auricular incision in the outermost part of the EAC, allowing the medial detachment of the flap. After advancement of the flap, there was exposure of the mastoid, insertion of the left sternocleidomastoid muscle (SCOM), parotid fascia, and cervical levels I and II. The facial nerve trunk was identified at the exit of the mastoid-style foramen and, shortly thereafter, dissected up to its bifurcation, allowing medial dislocation of the left parotid. Thus, the EAC lesion was removed under direct vision with a safety margin, leaving only a small area of anterior skin (Figure 2). Intraoperative frozen section biopsy of the surgical specimen confirmed free margins. An UPPER NECK was then performed (emptying of cervical levels II and III), but freezing did not identify disseminated disease to the neck.
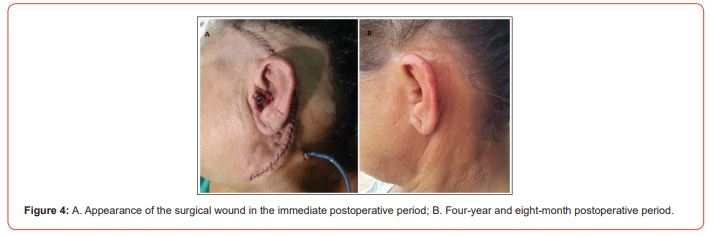
The reconstruction was performed with the rotation of an ECOM muscle flap, pedunculated in the occipital artery, which was sutured in the remaining skin of the EAC, tunneling the neo external auditory canal (Figure 3). The flap with the external ear was positioned in the original location and the ear was sutured in the neoconduct. A silicone mold was placed in it, which remained for thirty days, being removed on an outpatient basis (Figure 4).

Microscopic examination of the resected product showed welldifferentiated, superficially invasive squamous cell carcinoma, without affected lymph nodes, with free margins
The patient evolved satisfactorily, with preservation of hearing, and did not present recurrences until the follow-up of four years and eight months after the surgery.
Discussion
Squamous cell carcinoma of the external auditory canal affects individuals between the fifth and seventh decades of life, with a higher prevalence in women [3]. Unlike SCC of the auricle, which is associated with sun exposure [13] and actinic damage, [6] these tumors have different pathogenesis [4, 6]. They are associated with a history of cholesteatoma [5], HPV infection [9, 11], chronic suppurative otitis media and exposure to chemicals, with the most important factor appearing to be previous radiotherapy [5, 6].
The symptoms of presentation are varied, with otorrhea being the main symptom.6 The patient may also experience bleeding, otalgia, dizziness, deafness and facial paralysis. The classic history is of a patient complaining of otorrhea and otalgia with a report of chronic otitis, which is identified in at least one third of the patients [3]. In this context, it is common for the physician to diagnose a suppurative chronic otitis media and treat it. conservatively, delaying the diagnosis of SCC and worsening its prognosis [6].
CAE squamous cell carcinomas are aggressive tumors [6], however, when discovered in early stages, they have a good survival rate in up to 100% of patients [4].
These tumors spread primarily by direct extension, with the main affected sites being the auricle, the middle ear, the parotid gland, the temporomandibular joint, the facial nerve, the carotid canal and the jugular fossa. From the middle ear involvement, the tumor can affect mastoid cells, middle and posterior cranial fossa [3] and dura mater [8]. Distant metastases are rare and lymph node involvement is uncommon; when it occurs, it is due to the involvement of the retropharyngeal, preauricular and upper cervical chains [3].
Poor prognostic factors are middle ear invasion, lymphadenomegaly, facial nerve palsy, extensive tumor [3], dural involvement [8], and moderate to severe pain at the first visit [6]. Facial nerve invasion may be present in up to 35% of patients with advanced disease, and it is an indicator of poor prognosis [8]. It is also known that the presence of middle ear invasion reduces fiveyear survival from 59% to 23% [3].
The definitive diagnosis of these tumors is performed through biopsy of the lesion with histopathological examination.3 Regarding staging, there is still no consensus in the literature [8], but the system by Arriaga et al. [14] from the University of Pittsburg modified by Moody, Hircsh and Myers [15] has been shown to be useful and has gained support in the literature [8, 13]. This staging system is based on preoperative clinical factors and CT findings, as shown in (Table 1) [1].
Table 1:Modified Pittsburgh Staging.
Accurate assessment of the deep extension of tumors in the auricular region and associated lymph node enlargement is only possible through complementary tests [3, 8]. Computed tomography and magnetic resonance imaging (MRI) are the main tests used [3, 9, 10], and may also be angiography should be performed to evaluate the carotid artery, if a surgical approach is necessary [8], and audiometry [11].
Treatment depends on the size of the lesion, the location, the extent of the disease and the patient’s clinical conditions, and may require reconstructive techniques and microsurgery. Some authors advocate en bloc resection with partial, subtotal or total temporal bone resection, according to the tumor extension verified in the preoperative imaging exams [8]. According to Nyrop and Grontevd (2002), T1 and T2 tumors do not require extensive resection of the temporal bone, provided that adjuvant radiotherapy is provided for cases of incomplete tumor resection.
In general, the management of these patients is based on a combination of a surgical approach associated with adjuvant radiotherapy [3, 6, 9, 10].
Despite the classic diagnostic confusion with chronic otitis media, our patient had an early diagnosis, probably because the lesion was located in a very apparent region of the external auditory canal, facilitating its identification. In these cases, the prognosis is usually better, as confirmed by CT, which showed a T1 staging, with tissue formation located inside the left external auditory canal adjacent to the tympanic membrane, without signs of invasion to the middle ear or bone erosion.
Regarding the treatment, the INCA Internal Conduct Manual (2007) states that the reconstruction can be performed with locoregional flaps made from the temporal muscle, sternocleidomastoid muscle, scalp, pectoralis major myocutaneous, dorsal trapezius myocutaneous, latissimus dorsi and the from microsurgical flaps with rectus abdominis.
In the patient presented in this study, reconstructive surgery was performed with a sternocleidomastoid flap, which despite being a technique mentioned in the INCA Internal Conduct Manual (2007), no work was found in the literature that reported the use of this surgical technique.
The patient evolved satisfactorily, preserving her hearing, without relapses so far, which is equivalent to a follow-up of four years and eight months after the operation.
Final Comments
We present a case that used a sternocleidomastoid flap in the reconstruction of the external auditory canal, with excellent aesthetic and functional results. Currently, there is no consensus on the best type of surgical procedure for these tumors, due to the rarity of the pathology and the consequent difficulty in joining a large number of cases in the same service [1, 2, 11, 12]. We conclude that studies with greater number of patients to determine surgical treatment protocols for EAC squamous cell carcinoma.
Acknowledgement
None.
Conflict of Interest
None.
References
- Nyrop M, Grøntevd A (2002) Cancer of the external auditory canal. Arch Otolaryngol Head Neck Surg 128: 834-837.
- Ogawa K, Nakamura K, Hatano K, Uno T, Fuwa N, et al. (2007) Treatment and prognosis of squamous cell carcinoma of the external auditory canal and middle ear: a multiinstitutional retrospective review of 87 patients. Int J Radiation Oncology Biol Phys 68(5): 1326-1334.
- Gonzalez FM, Paes Junior AJO, Tornin OS, Souza RP (2007) Carcinoma espinocelular do conduto auditivo externo: estudo por tomografia computadorizada de seis casos. Radiol Braz 38 (3): 181-185.
- Hoshikawa H, Miyashita T, Mori N (2012) Surgical Procedures for External Auditory Canal Carcinoma and the Preservation of Postoperative Hearing. Cases Rep Surg 2012: 1-4.
- Boamah H, Knight G, Taylor J, Palka K, Ballard B (2011) Squamous Cell Carcinoma of the External Auditory Canal: a case report. Cases Reports in Otolaryngology 2011: 1-4.
- Lobo D, Llorente J, Suárez C (2007) Squamous Cell Carcinoma of the External Auditory Canal. Skull Base 18 (3): 167-172.
- Chung JH, Lee SH, Park CW, Tae K (2012) Mucoepidermoid Carcinoma in The External Auditory Canal: a case report. Cancer Res Treat 44 (4): 275-278.
- Ministry of Health (2007) National Cancer Institute. INCA Internal Routine: head and neck surgery service. Rio de Janeiro: CEDC.
- Ong CK, Pua U, Chong VFH (2008) Imaging of carcinoma of the external auditory canal: a pictorial essay. Cancer Imaging 8: 191-198.
- Trojanowska A, Drop A, Trojanowski P, Rosinska Bogusiewicz K, Klatka J, et al. (2012) External and middle ear diseases: radiological diagnosis based on clinical signs and symptoms. Insights Imaging 3: 33-48.
- Arora S, Sharma JK, Pippal S, Sethi Y, Yadav A (2009) Carcinoma de osso temporal com extensão intracraniana. Braz J Otorhinolaryngol 75 (5): 765.
- Gillespie MB, Francis HW, Chee N, Eisele DW (2001) Squamous Cell Carcinoma of the Temporal Bone: a radiographic-pathologic correlation. Arch Otolaryngolol Head Neck Surg 127: 803-807.
- Madsen AR, Gundgaard MG, Hoff CM, Maare C, Holmboe P, et al. (2008) Cancer of the external auditory canal and middle ear in Denmark from 1992 to 2001. Head Neck 30: 1332-1338.
- Arriaga M, Curtin H, Takahashi H, Hircsh BE, Kamerer DB (1990) Staging proposal for external auditoy meatus carcinoma based on preoperative clinical examination and computed tomography findings. Ann Otol Rhinol Laryngol 99: 714-721.
- Moody SA, Hircsh BE, Myers EN (2000) Squamous Cell Carcinoma of the External Auditory Canal: an evaluation of a staging system. Am J Otol 21: 582-588.
-
Klecius Leite Fernandes*. Squamous Cell Carcinoma of the External Auditory Canal: A Sternocleidomastoid Flap Reconstruction. On J Otolaryngol & Rhinol. 5(5): 2022. OJOR.MS.ID.000623.
-
Head and neck tumors, Cell carcinoma, Auditory canal, Smoking, Otitis media, Lymph nodes, Dizziness, Deafness, Facial paralysis, Parotid gland, Middle ear.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






