 Research Article
Research Article
Laryngectomy : Experience with 37 Cases in A Tertiary Care Hospital
K.M.Reza-UL-Haq1, Mohammed Yousuf2, Refat Tabassum3, Khaleda Nazneen Bari4 and Richmond Ronald Gomes5*
1Associate Professor, Dept of ENT& Head-Neck Surgery, Delta Medical College, Dhaka, Bangladesh
2Professor & Head, Dept of ENT& Head-Neck Surgery, Delta Medical College, Dhaka, Bangladesh
3Professor (CC), Dept of Biochemistry, Basundhara Ad-din Medical College Hospital, Bangladesh
4Associate Professor, Dept of Opthalmology, Delta Medical College, Dhaka, Bangladesh
5Professor, Dept of Medicine, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh
Richmond Ronald Gomes, Professor, Dept of Medicine, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh.
Received Date:February 05, 2024; Published Date:April 29, 2024
Abstract
Background:Laryngectomy, the surgical procedure involving the removal of the larynx, is a critical intervention often employed in the management of advanced laryngeal conditions, particularly cancer. Laryngeal disorders, such as malignancies, pose significant challenges, necessitating intricate surgical interventions for both therapeutic and palliative purposes.
Objective: To analyze and document the experiences associated with laryngectomy in a Tertiary Care Hospital.
Materials and Methods:A prospective study was undertaken from January 2017 to September 2023, in Delta Medical College and Hospital, Mirpur, Dhaka, involving 37 patients who underwent laryngectomy. Detailed examinations, imaging studies, and histological assessments were performed to stage the disease according to the TNM staging system. Patients were counseled, and informed consent was obtained. Laryngectomy was performed in all cases, and data were collected on a preformed proforma. Statistical analysis was carried out using SPSS version 25
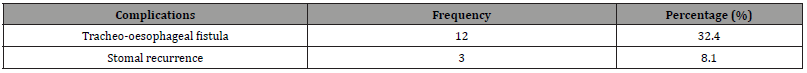
Results:The study predominantly included males (91.9%), and the age distribution ranged from 31 to over 60 years. Various reconstruction techniques were employed, with flap reconstruction being the most common. Tracheo-oesophageal fistula emerged as the primary complication, affecting 32.4% of patients.
Conclusion:This study provides insights into the demographics, reconstruction methods, and complications associated with laryngectomy in advanced carcinoma larynx cases. The predominance of males and the high occurrence of tracheo-oesophageal fistula highlight the need for further research to validate and expand upon these findings. This study serves as a foundation for future investigations, aiming to optimize treatment protocols and improve the overall quality of care for patients undergoing laryngectomy in this region.
Keywords:Laryngectomy; Recurrent laryngeal cancer; Tracheo-oesophageal fistula; Stomal recurrence
Introduction
Following total laryngectomy surgery for advanced or recurrent laryngeal cancer, a laryngectomy stoma is created [1]. Laryngeal cancer stands as the most prevalent head and neck cancer and is the eleventh most common cancer among men globally, although its occurrence in women is relatively rare [2]. Laryngeal carcinomas are categorized based on their anatomical locations, which include the supraglottic, glottis, or subglottic regions [2, 3]. The symptoms of laryngeal cancer vary depending on the tumor’s location, size, and degree of invasion. Information about the tumor’s location and extension pattern within these regions offers insights into the disease’s progression and anticipated response to treatment. The majority of malignant neoplasms in the larynx originate from the surface epithelium, classifying them as either keratinizing or non-keratinizing squamous cell carcinomas (SCC). Additionally, there are rare malignant forms such as verrucous carcinoma, adenocarcinoma, fibrosarcoma, and chondrosarcoma [4].
Head and neck cancer, including laryngeal cancer, is associated with exposure to environmental toxins and chemical carcinogens, such as tobacco and alcohol, asbestos, wood dust, cement, polycyclic aromatic hydrocarbons and therapeutic radiation. Gastroesophageal reflux disease (GERD), nutritional deficiency particularly that of vitamins and iron has been linked with hypopharyngeal and laryngeal carcinoma [5].
The treatment of patients with laryngeal carcinoma should be planned to provide optimal survival, free of disease, with maximum functional results. The treatment for T1 and T2 lesions usually involves radiotherapy or endoscopic surgery with or without laser. Total laryngectomy alone or in conjunction with neck dissections and/or radiotherapy with or without chemotherapy is used for advanced T3 and T4 lesions [6]. The first laryngectomy was performed by Billroth in 1873 and for much of the 20th century; this procedure has been recognized as the gold standard treatment for advanced cancers of the larynx and hypopharynx [7].
Complications following total laryngectomy such as wound infection, pharyngocutaneous fistula, carotid blow out rupture, chyle leak, airway and swallowing problems increases the morbidity and mortality thus, adversely affect the prognosis [8-10]. Several risk factors have been implicated in the development of complication following total laryngectomy, and these include radical neck dissection, previous radiation, pre-operative tracheostomy and extensive surgery with flap necrosis, poor surgical technique, etc [11]. Early diagnosis and prompt management of these complications is important. This study aims to find out the pattern of complications following laryngectomy in our region.
Materials and Methods
This prospective descriptive study was carried out at the Department of Head and Neck Surgery in Delta Medical College and Hospital, Mirpur, Dhaka, spanning from January 2017 to September 2023. The study involved 37 patients of varied ages and genders who underwent laryngectomy for advanced carcinoma of the larynx. A comprehensive examination, with a focus on laryngeal assessment, was conducted for each patient, accompanied by a detailed medical history. Baseline investigations included neck CT scans, and in cases where CT scans were inconclusive, MRI scans were performed. Metastasis assessment was carried out, and endoscopy with biopsy was performed for histological diagnosis. Disease staging followed the TNM (Tumor, Node, and Metastasis) staging system. Patients and their relatives received counseling on the nature of the disease, treatment options, surgery expenses, and voice rehabilitation. Informed consent was obtained from all patients and their relatives, outlining the risks, benefits, and potential complications associated with total laryngectomy. The study received approval from the hospital’s ethical committee. Laryngectomy was performed on all patients, and data were recorded using a preformatted proforma. Statistical analysis, utilizing SPSS version 25, included presenting frequencies and percentages for qualitative variables and Mean ± SD for quantitative variables.
Results
Table 1:Age distribution of the study subject (n=37).
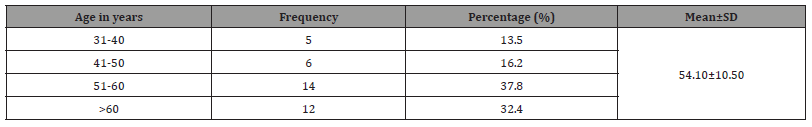
Table 2:Sex distribution of the study subject (n=37).
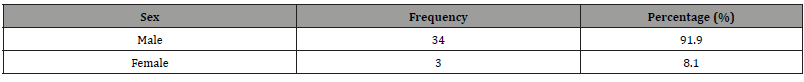
Table 3:Reconstruction type of the study subject (n=37).
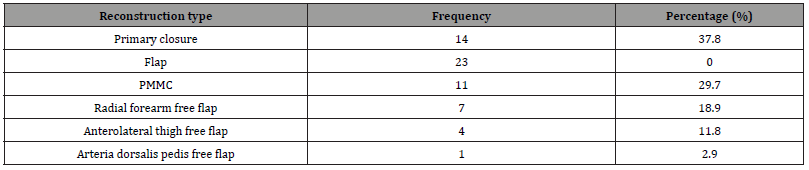
Table 4:Complication of the study subject (n=37).
Discussion
Laryngeal malignancy constitutes 20% of all head and neck malignancies. The choice of treatment for laryngeal malignancy depends on several factors, including the tumor stage, its location, presence of lymph node metastasis, the overall condition of the patient, and any associated comorbidities. In cases of advanced T3 and T4 stage laryngeal tumors, the primary treatment approach involves laryngectomy followed by postoperative radiotherapy [2].
In this study laryngectomy was performed in patients having age range from 32-70 years with mean age of 54.10+10.50 years which is comparable to study of Iseh [12] where age range was 30- 70 years (mean, 53.8 years). Another study Wahid, et al. [2] reported laryngectomy was performed in patients having age range from 38-72 years with mean age of 57.34+S.D 9.6 years [2]. Carcinoma larynx is more common in people of middle or older age because of more exposure of this age group to carcinogens.
In this study male (91.9%) were the dominant victims of carcinoma larynx which is in accordance to the work of Bhandary [13] who reported that 87 (96%) were males and 3 (4%) were females. Another study Wahid, et al. [2] reported male were the dominant victims of carcinoma larynx. The reason for predominant involvement of males could be their more exposure to risk factors of laryngeal tumours.
This study shows the predominant complication, tracheo-oesophageal fistula, accounts for 32.4% of cases. Notably, the absence of stomal recurrence raises questions about the effectiveness of certain interventions. The complication of tracheostomal stenosis is reported to have an overall incidence of 33% in the literature [14- 16]. Similar study Aliyu and Riseh8 found the most common complication after laryngectomy is pharyngocutaneous fistula, wound infection and pharyngocutaneous fistula are the two most common complications, with 4(20%) patient each developing these complications. Post-operative wound infections are a major source of infectious morbidity in laryngectomy patients. The overall incidence of post-operative wound infection reported after major head and neck surgery is 23% and this becomes higher in those patients who have received pre-operative radiotherapy [17]. Similarly Weber [18] also reported that the incidence of major and minor complications ranged from 52% to 59%. Bajaj and colleagues [19] also encountered minor and major complications after laryngectomy and pharyngocutaneous fistula were 15.2% in his study. Similarly, the wound infection in this study is in accordance to Maharjan [20] report where wound infection was 20% but he had higher incidence in form of pharyngocutaneous fistula (30%) and superficial flap necrosis (15%). The results of this study are also at variance from the results of Qureshi [21] who had fistula in 23% and wound infection in 5% patients only.
Conclusion
This study shows the majority of patients were male. The primary treatment approach involved laryngectomy, and the reconstruction techniques varied, with flap reconstruction being the predominant method. Tracheo-oesophageal fistula emerged as the most prevalent complication. However, further research and larger- scale studies are warranted to validate these findings and explore additional factors influencing the outcomes of laryngectomy in the context of advanced carcinoma larynx. This study serves as a foundation for future investigations aimed at refining treatment protocols and enhancing the overall quality of care for patients undergoing laryngectomy in this region.
Acknowledgment
None.
Conflict of Interest
No Conflict of Interest.
References
- Jackson C, Grigg C, Green M, Grigg R (2019) Care of laryngectomy stomas in general practice. Aust J Gen Pract 48(6): 373-377.
- Wahid FI, Khan A, Khan IA (2013) Total laryngectomy: an experience of 26 cases in a tertiary care hospital. JLUMHS 12(01): 34-38.
- Elmiyeh B, Dwivedi RC, Jallali N, Chisholm EJ, Kazi R, et al. (2010) Surgical voice restoration after total laryngectomy: An overview. Indian J Cancer 47: 239-247.
- Ritoe SC, Bergman H, Krabbe PF, Kaanders JH, van den Hoogen FJ, et al. (2006) Cancer recurrence after total laryngectomy: treatment options, survival, and complications. Head Neck 28: 383-388.
- Sharifian HA, Najafi M, Khajavi M (2008) Early oral feeding following total laryngectomy. Tanaffos 7: 64-70.
- Babin E, Blanchard D, Hitier M (2011) Management of total laryngectomy patients over time: from the consultation announcing the diagnosis to long term follow-up. Eur Arch Otorhinolaryngol 268: 1407-1419.
- Lefebvre JL, Rolland, Tesselaar M, Bardet E, Leemans CR, et al. (2009) Phase 3 Randomized Trial on Larynx Preservation Comparing Sequential vs Alternating Chemotherapy and Radiotherapy. J Natl Cancer Inst 101: 142-152.
- Aliyu D, Riseh K (2015) Clinical profile of post-operative complications of total laryngectomy for laryngeal carcinoma: A 12-year observation in Sokoto, Nigeria. Orient Journal of Medicine 27(3-4): 99-104.
- Javed A, Zafar A, Azeem A, Malik IA (2006) Complications of total laryngectomy. Pak J Sci 22(1): 33-37.
- Ganly I, Patel S, Matsuo J, Singh B, Kraus D, et al. (2005) Postoperative complications of salvage total laryngectomy. Cancer 103: 2073-2081.
- Maharjan R, Adhikari P, Khalilullah S, Sinha BK, Baskota DK (2010) Early complications of total laryngectomy: A retrospective study. Nepalese Journal of ENT Head & Neck Surg 1: 17-18.
- Iseh K (2011) Total Laryngectomy for Laryngeal Cancer in a Nigerian Tertiary Health Center: Prognosis and Outcome. J Surg Tech Case Rep 3: 23-30.
- Bhandary SK, Bhat VS, Shenoy MS (2011) Laryngectomy: From stridor to survival-Our Experience. NUJHS 1: 75-80.
- Hall FT, O’Brien CJ, Clifford AR, McNeil EB, Bron L, et al. (2003) Clinical outcome following total laryngectomy for cancer. ANZ J Surg 73: 300-305.
- Pengiran SDN, Marina MB, Mohd RMY, Primuharsa PSHA, Sani A (2010) Complications following tracheoesophageal puncture: A tertiary Hospital Experience. Ann Acad Med Singapore 39: 565-568.
- Pantvaidya GH, Raina S, Mondal A, Deshmukh A, Nair D, et al. (2017) Total laryngectomy: Surgical morbidity and outcomes – A case series. Indian J Cancer 54: 621-625.
- Ampil FL, Nathan CO, Calito G, Lian TF, Aarstad RF (2004) Total laryngectomy and postoperative radiotherapy for T4 laryngeal cancer: a 14-year review. Am J Otolaryngol 25: 88-93.
- Weber RS, Berkey BA, Forastiere A, Cooper J, Maor M, et al. (2003) Outcome of salvage total laryngectomy following organ preservation therapy: the Radiation Therapy Oncology Group trial 91-11. Arch Otolaryngol Head Neck Surg 129: 44-49.
- Bajaj Y, Shayah A, Sethi N, Harris AT, Bhatti I, et al. (2009) Clinical outcome of total laryngectomy for laryngeal carcinoma. Kathmandu University Medical Journal 7: 258-262.
- Maharjan R, Adhikari P, Khalilullah S, Sinha BK, Baskota DK (2010) Early complications of total laryngectomy: A retrospective study. Nepalese Journal of ENT Head & Neck Surg 1: 17-18.
- Qureshi SS, Chaturvedi P, Pai SS, Chaukar DA, Deshpande MS, et al. (2005) A prospective study of pharyngocutaneous fistula following total laryngectomy. J Cancer Res Ther 1: 51-56.
-
K.M.Reza-UL-Haq, Mohammed Yousuf, Refat Tabassum, Khaleda Nazneen Bari and Richmond Ronald Gomes*. Laryngectomy : Experience with 37 Cases in A Tertiary Care Hospital. On J Otolaryngol & Rhinol. 6(5): 2024. OJOR.MS.ID.000650.
-
Laryngectomy, Head and neck cancer, Swallowing problems, laryngeal conditions, Tracheostomy, Lymph node, Carcinoma larynx, Reconstruction techniques, Laryngeal disorders, Tracheo-oesophageal.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






