Research Article
Research Article
Convergence Technique is the Easy and Reliable Landmark for Identification of the Facial Nerve in Parotid Surgery
Islam MA1*, Rahman MM2, Mohammad T3, Kazi MM4, Chowdhury NH5, Rahman ASML6 and Milki FU7
1Professor & Head, Otolaryngology–Head & Neck Surgery, Bangladesh Medical college Hospital, Bnagladesh
2Associate Professor & Head, Ad-Din Bashundhara Medical College, Dhaka, Bnagladesh
3Registrar, ENT, Popular Medical College, Dhaka, Bnagladesh
4Assistant registrar, ENT, Bangladesh Medical College Hospital, Bnagladesh
5Assistant Professor, ENT, Bangladesh Medical College, Bnagladesh
6Resident Surgeon, ENT, Bangladesh Medical College Hospital, Bnagladesh
7Consultant, ENT, Bangladesh Medical College Hospital, Bnagladesh
Md Ashraful Islam MBBS, FCPS, FICS, FACS, FRCS (Glasgow), Professor & Head, Otolaryngology-Head & Neck Surgery, Bangladesh Medical College Hospital, Bnagladesh
Received Date: June 29, 2022; Published Date: July 15, 2022
Abstract
Aim and objective: The aim and objective of this study was to evaluate the consistency, accuracy, and safety of the convergence technique in
identifying the facial nerve during parotid surgery.
Patients and methods: A prospective study was carried out between January 2012 to December 2022 at the Tertiary care hospital in Bangladesh.
120 patients were included in the study; amongst them 80 (67%) were males and 40 (33%) were females with a mean age of 43.52±15.63 years.
Patients presented with pleomorphic adenoma (85), chronic sialectasis (05), parotid cyst (02), parotid sinus (01), mucoepidermoid carcinoma (24)
adenoid cystic carcinoma (02) and squamous cell carcinoma (01) were subjected to superficial parotidectomy and total parotidectomy. Surgical
procedures were done by using the convergence technique for identification of the facial nerve trunk.
Results: All 120 patients underwent superficial and total parotidectomy. Facial nerve trunk was successfully identified in all the patients with
no intra-operative complications. Operative time ranged from 50 to 180 minutes with a mean time 90.70±15.68 minutes. Facial nerve deficit of the
marginal mandibular nerve (MMN) was noted in 5 patient (3.8 %), 02 had difficulty in eye closure (1.5%). No patient reported with surgical site
infection, skin flap necrosis and hematoma in all the patients.
Conclusion: Convergence technique is the reliable landmark in the triangle technique for the identification of facial nerve trunk with relative
ease, safety and accuracy during parotid surgical procedure. This can be a very useful method to minimize the facial nerve injury during parotid
surgery.
Keywords: Facial nerve trunk; Styloid process; Convergence technique; Parotid surgery
Background
The facial nerve is one of the most important structures encountered during parotidectomy. The neurovascular structures that pass through the parotid gland from lateral to medial are facial nerve, retromandibular vein, external carotid artery, superficial temporal artery and maxillary artery [1, 2]. The greater auricular nerve emerges along the posterior aspect of the sternocleidomastoid muscle at the Erb’s point, ascends vertically across the oblique sternocleidomastoid muscle and its branches enter the gland from the neck and remains superficial [3]. Parotid surgery is warranted for benign and malignant neoplasm, chronic inflammatory diseases, sialolithiasis, intra-parotid cysts/sinuses and lymphadenopathy; and many other diseases. The methods of identification of the facial nerve and its importance are aptly described by many eminent surgeons using varous anatomical landmarks during parotidectomy [4, 5]. In this article styloid process is considered the very consistent robust anatomical landmark in the triangle technique in conjunction with the tragal cartilage to tragal pointer and the origin of the posterior belly of the digastric muscle at the mastoid tip.
Facial nerve and the parotid gland,
The facial nerve exits from the stylomastoid foramen slightly posterior to the styloid process and anteromedial to the mastoid process [5, 6]. The main trunk is approximately 1.3cm in length enters into the parotid gland and divides into cervico-marginal and zygomatico-temporal branches; and of course, buccal branches (upper and lower buccal) remain common in both the divisions. The cervico-marginal branches supply the muscles of the mouth and neck; and zygomatico-temporal branches supply the muscles of the forehead and eye. The facial nerve arbitrarily divides the gland into superficial and deep lobes [6].
Introduction
“He who devotes himself to surgery must be versed in the science of anatomy. Those who lack a good grasp of anatomy are prone to serious and even fatal mistakes.” Al-Zahrawi (936-1013 A.D.). The preservation of the facial nerve is one of the most important aspects of a successful parotid surgery because of its critical functions and intimate relation with the parotid gland [7]. It requires great precision because the surgeon has to locate and operate around these important structures. Although there are several ways to locate the facial nerve such as antegrade approach with the identification of the main trunk and the retrograde approach with the identification of its branches to reach the main trunk [7]. Nevertheless, detection of the facial nerve become a crucial point in parotid surgery. The following anatomical landmarks are the key to locate the facial nerve trunk (anterograde) [8].
Tragal pointer (TP): The nerve lies approximately 1.0-1.5cm
deep and slightly anterior and inferior to the tip of the tragal
cartilage
1. Posterior belly of the digastric muscle (PBDM): The nerve lies
approximately 1.0cm deep to the medial attachment of the
posterior belly of the digastric muscle to the digastric groove
of the mastoid bone.
2. Tympanomastoid suture (TMS): Facial nerve trunk is situated
3mm inferior to suture to the stylomastoid foramen.
3. Styloid process (SP): The nerve trunk is found inferolateral to
it.
Retrograde approach of the nerve trunk through one of the
branches of the facial nerve [9].
1. Marginal mandibular branch: it courses the deep surface of the
tail of the parotid and often reliably found at the angle of the
mandible.
2. Buccal branch: it runs parallel to and 1cm below the arch of the
zygoma traveling toward the corner of the mouth.
3. Zygomatic branch: any one of the ophthalmic branch where
they cross the arch of the zygoma near the upper anterior
corner of the gland.
4. Retromandibular vein: This vein is also used as a landmark
when evaluating imaging studies, as this vein marks the
division of the deep and superficial lobes. This relationship
is important as it approximates the depth of the facial nerve
which lie superficially.
Besides all those described above, the following points are also
considered for facial nerve identification.
1. Parotid-mastoid fascia (PMF): The fascia is incised as the final
step before identifying the trunk of the facial nerve. The nerve
is found within fat deep to the parotid-mastoid fascia and
localized employing the landmarks noted above [9, 10].
2. The facial nerve stimulator/monitor helps to localize the nerve
through stimulation with observation of facial movement [11].
3. Partial removal of the mastoid process is done by chisel,
rongeur, or drill to identify nerve in mastoid [12].
4. Gamma probe: It is used to identify a sentinel lymph node (Tc
99 injection done several hours before). The sentinel node was
overlying the lower division of the facial nerve, warranting
identification and preservation of the nerve [11-13].
It is evident from the published literature that there are so many landmarks used to identify the facial nerve trunk because of its variable and inconsistent position. So parotid surgeons yet to reach to a consensus regarding the safety and reliability of each of these landmarks [14].
Material and Methods
Design:Prospective study
Duration:January 2012 to December 2022
Setting:Tertiary care hospital
Study number:120 patients with different parotid diseases underwent parotid surgeries.
Triangle Landmarks:A triangle was made from
a. The tragus to the mastoid tip anteriorly,
b. Along the long axis of the tragus to the styloid process and
c. From the mastoid tip crossing the insertion of the posterior
belly of the digastric muscle to the styloid process (Figure 1).
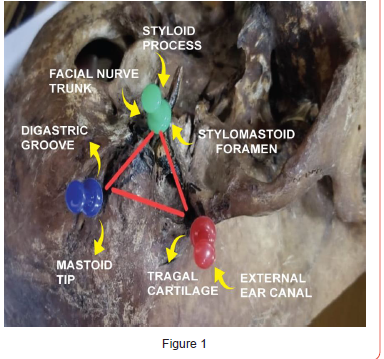
Convergence:A meeting point posterolateral to the styloid
process at the stylomastoid foramen where the lines drawn:
a) along the long axis of the tragus to the styloid process and
b) from the mastoid tip crossing the insertion of the posterior
belly of the digastric muscle to the styloid process (Figure 2).
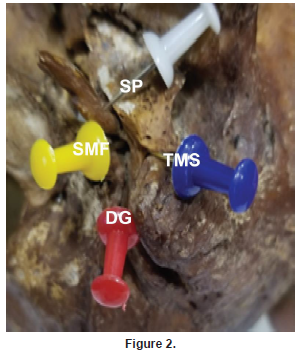
Facial nerve trunk identification: The three most easily identifiable and anatomically constant landmarks were selected and their respective distance from the styloid process was measured. The facial nerve trunk was identified at the point of convergence of the lines from the tragal pointer and mastoid tip across the PBM to the styloid process.
Surgical technique

a. A modified cosmetic incision was made starting 1 to 2cm
above the tragus approaching to the neck behind tragus in the
external auditory canal making a sinuous curve.
b. The approach to the trunk of the facial nerve involves 3 steps.
a) First step, the 3 anatomical landmarks were identified.
b) The first landmark was at the center of the tragal cartilage.
c) From that, a line was traced to the tip of the MP that was the
second landmark.
d) The third landmark was the SP, and the reference triangle was
delineated (Figure 3).
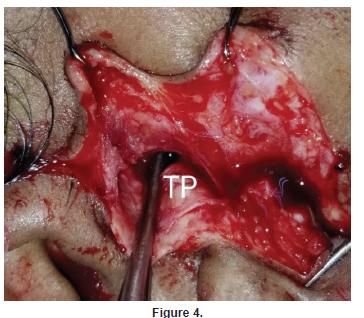
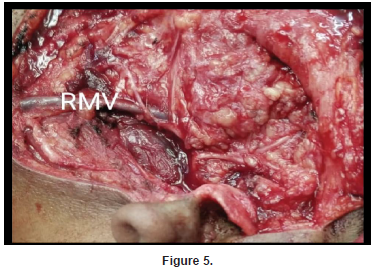
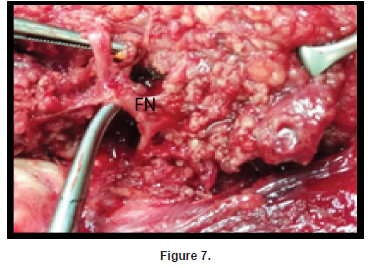
The second step was to make an surgical triangle that started along the long axis from the center of the tragal cartilage crossing the TP to the SP and the third step started from the MP to SP crossing the PBDM that was marked the convergent point at the SP. The predicted position of the facial nerve was located at the reference angle of the surgical triangle lateral to the SP. All references were chosen by means of dissection and palpation; not by objective measurements. Once identified, the facial nerve was freed until its trunk and its major 2 divisions were individualized (Figures 4-7).

Results
The distribution of sex is shown in Table 1.
(Table 1)
130 patients presented in different ages which is shown in
Table 2.
(Table 2)
Parotid surgery was done in 130 patients with different
diseases that depicted in Table 3.
(Table 3)
The facial nerve trunk (FNT) was located at the site of
convergence in all 130 patients that is shown in Table 4.
(Table 4)
Table 1:

Table 2:
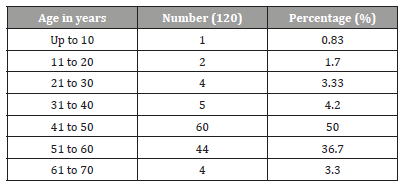
Table 3:

Table 4:

It has been observed in this study that the facial nerve exited the skull through the stylomastoid foramen for a length of 1.3cm approximately; and divide in 2 main divisions cervico-marginal and zygomatico-temporal branches; and of course, buccal branches (upper and lower buccal) remain common in both the divisions within the parotid gland in all 120 patents. A triangle was made from tragal cartilage to mastoid tip with a mean distance of 9.5±1.5mm. The mean distance between tragal pointer to styloid process was 17.5±1mm, posterior belly of digastric from mastoid tip to styloid process was 7.5±1.5mm, tragal pointer to facial nerve trunk was found 13±1.2mm and posterior belly of digastric to facial nerve trunk was 6.5±0.5 mm. The facial nerve was located at the exact convergence between the tragal pointer to styloid process and posterior belly towards styloid process. The main trunk of facial nerve was successfully identified in all cases using Convergence technique in both anatomical and surgical study. So the facial nerve was located at the exact convergence between the tragal pointer to styloid process and posterior belly to styloid process posterolateral to the styloid process at the exit point of the stylomastoid foramen.
Discussion
The location of the facial nerve trunk starts from its exit from the stylomastoid foramen and travels for a short distance of approximately 1.3cm enters into the parotid gland [8, 15]. It then divides into two major branches namely upper and lower divisions such as upper zygomatico-temporal and lower cervico-marginal branches with a common buccal branch to both. These branches supply the ipsilateral face, eye, forehead, temporal region and upper neck. This nerve is arbitrarily but not anatomically dividing the parotid gland in to superficial and deep lobes [16].
The crucial importance of the nerve lies on the fact that this shortest FNT and its branches are intimately related with the parotid gland and other vascular structures which pass through this gland. So the injury to the FNT and even any of its branches is the most common complication of parotid surgery 17 because of the functional and aesthetic point of concern to the patient. As a result, the paramount importance is the identification of the facial nerve during parotidectomy that is practically a paradigmatic procedure [15, 17]. Both the main trunk and peripheral branches must be identified and preserved to prevent permanent aesthetic sequelae and medico-legal actions related to facial paralysis [18]. In this study facial nerve trunk identified with relative ease, safety and accuracy by means of convergence technique.
In reviewing the published literature until now, there are different ways of identification of the facial nerve such as anterograde and retrograde procedure; and by using so many devices namely facial nerve monitor/stimulator, gamma probe etc [8-13]. The most common and easy technique to identifying the FNT at its point of exit from the stylomastoid foramen before it divides in to upper and lower main branches in the parotid gland is the preferred method of getting the facial nerve [19] that has clearly demonstrated and shown in this technique.
It is anatomically proven that, a very constant landmark for facial nerve is the stylomastoid foramen (SMF) situated posterolateral to the styloid process from where the FNT exits from the temporal bone. But during surgical procedure especially in the diseased parotid gland, it is very difficult to find the styloid process and particularly this foramen; as it is mainly a palpatory landmark and most importantly because it remains surrounded by thick fascia which is continuous with the periosteum of skull base [20-22]. In this study the convergence point was taken a reliable and easy landmark based on the styloid process using the triangle technique described above to locate the FNT from the SMF.
It is evident that tragal pointer (TP) is considered a very popular landmark and the nerve usually lies approximately 1.0- 1.5cm deep and slightly anterior and inferior to the tip of the tragal cartilage (TC) [22, 23]. The only drawback of the tragus is that it is a cartilaginous structure which is mobile, asymmetrical having a blunt and irregular tip. In this study convergence point was marked on the basis of styloid process with another anatomical landmark such as SMF, TC and TP.
In this study triangle was considered as the basic model to find out the point of convergence where mastoid process was taken mainly a outer palpatory landmark, the process lies deep to the insertion of the sternocleidomastoid muscle (SCM). Posterior belly of the digastric muscle (PBDM) lies medial to SCM. The FNT lies approximately 1.0cm deep to the medial attachment of the posterior belly of the digastric muscle to the digastric groove of the mastoid tip which is easily identifiable by drawing a line from the MT along the PBDM to the styloid process which corresponds to the other published literature [24-26]. In this study it was seen that this line meets to a point posterolateral to the styloid process with another line drawn from TP to styloid process; that is the convergence point lies over the FNT.
The present study set out to locate the ease and accuracy of facial nerve identification using the triangle formed by the tragal cartilage, the mastoid tip and the styloid process. The FNT was accurately and quickly found at the point of convergence of the long axis from the TP to SP and from MT across the PBDM to styloid process. For easy and prompt identification of the nerve trunk, the surgeon needs to systematically look for the anatomical landmarks.
Recommendations
The proposed surgical triangle and the angle at the point of convergence inferolateral to the SP was practically the anatomical orientation that could make surgery around the parotid region safer and quicker. This approach offers substantial advantages when compared with other methods described in the published literature so far. It evaluates nerve position accurately; the 3 anatomical landmarks are easy to identify and styloid process is easily located by palpation during surgery and are not distorted by the pathologic conditions.
Conclusion
The point of convergence of the triangle technique is the consistent, prominent and easily identifiable anatomical landmark described in this article allowed a fast and safe identification of the facial nerve and may be of significant help during parotid surgery. Operative identification of the facial nerve trunk is a step-by-step procedure in which identification of the anatomic landmarks is highly advisable. The final success of the operation depends to a vast extent on the safe handling of the facial nerve and its branches as well as the use of bipolar diathermy during the surgical procedure.
Acknowledgement
We are grateful to Kauser Ahmed Shahin, Graphic Designer, UniMed UniHealth Pharmaceuticals Limited for his secretarial assistance.
Conflict of Interest
No conflict of interest.
References
- Alexander de Ru J (2001) Landmarks for parotid gland surgery. J Laryngol Otol 115: 122-125.
- Somnath S, Pal S, Sengupta M, Chowdhury K, Saha VP, et al. (2014) Identification of Facial Nerve During Parotidectomy: A Combined Anatomical & Surgical Study. Indian J Otolaryngol Head Neck Surg 66(1): 63-68.
- Murphy R, Dziegielewski P, O’Connell D, Seikaly H, Ansari K (2012) The great auricular nerve: an anatomic and surgical study. J Otolaryngol Head Neck Surg 41(suppl 1): S75-S77.
- Wetmore SJ (1991) Surgical landmarks for the facial nerve. Otolaryngol Clin North A 24(3): 505-530.
- Al-Qahtani KH (2020) A new landmark for the identification of the facial nerve during parotid surgery: A cadaver study. Laryngoscope Investig Otolaryngol 5(4): 689-693.
- Janes RM (1940) The Treatment of Tumours of the Salivary Glands by Radical Excision. Can Med Assoc J 43(6): 554-559.
- Pereira JA, Merí A, José Potau JM (2004) A Simple Method for Safe Identification of the Facial Nerve Using Palpable Landmarks. Arch Surg 139(7): 745-747.
- de Ru Javan, BleyB, Lubsen RL, Hordijk GJ (2001) Landmarks for parotid gland surgery. J Laryngol Otol 115: 122-125.
- Lathrop FD (1949) Technique of exposing the facial nerve as an aid to surgery of the parotid gland. Surg Clin North Am 29673- 29677.
- Conley J (1978) Search for and identification of the facial nerve. Laryngoscope 88: 172-175.
- McCabe BF, Work WP (1968) Parotidectomy with special reference to the facial nerve. Otolaryngology IV (Sec III): 37-53.
- Lydiatt DD (2003) Medical Malpractice and Facial Paralysis. Arch Otolaryngology Head Neck Surg 129: 50-53.
- Stennert E, Wittekindt C, Klussman PJ, Arnold G, Guntinas-Lichius O (2004) Recurrent Pleomorphic Adenoma of the Parotid Gland: A Prospective Histopathological and Immunohistochemical Study. The Laryngoscope 114: 158-163.
- Redaelli de Zinis LO, Piccioni M, Antonelli AR, Nicolai P (2008) Management and prognostic factors of recurrent pleomorphic adenoma of the parotid gland: personal experience and review of the literature. Eur Arch Otorhinolaryngology 265(4): 447-452.
- Makeieff M, Pelliccia P, Letois F, Mercier G, Arnaud S, et al. (2010) Recurrent Pleomorphic Adenoma: Results of Surgical Treatment. Ann Surg Oncol 17(12): 3308-3313.
- Witt RL, Weinstein GS, Rejto LK (2005) Tympanomastoid suture and digastric muscle in cadaver and live parotidectomy. Laryngoscope 115(4): 574-577.
- Holsinger FC, Bui DT (2007) Anatomy, function, and evaluation of the salivary glands; in Myers EN, Ferris RL (Eds.): Salivary Gland Disorders. Berlin, Springer, p 1-16.
- Wang SJ, Eisele DW (2007) Superficial parotidectomy; in Myers EN, Ferris RL (Eds.): Salivary Gland Disorders. Berlin, Springer, pp 247-246.
- Joseph ST, Sharankumar S, Sandya CJ, Sivakumar V, Sherry P, et al. (2015) Easy and Safe Method for Facial Nerve Identification in Parotid Surgery. J Neurol Surg B Skull Base 76(6): 426-431.
- Saha S, Pal S, Sengupta M, Chowdhury K, Saha VP, et al. (2014) Identification of facial nerve during parotidectomy: a combined anatomical & surgical study. Indian J Otolaryngol Head Neck Surg 66(1): 63-68.
- Borle RM, Jadhav A, Bhola N, Hingnikar P, Gaikwad P (2019) Borle's triangle: A reliable anatomical landmark for ease of identification of facial nerve trunk during parotidectomy. J Oral Biol Craniofac Res 9(1): 33-36.
- Owusu JA, Parker NP, Rimell FL (2013) Postoperative facial nerve function in pediatric parotidectomy: a 12-year review. Otolaryngol Head Neck Surg 148(2): 249-252.
- Hogg SP, Kratz RC (1958) Surgical exposure of the facial nerve. Arch Otolaryngol 67: 560-561.
- Kratz RC, Hogg S (1958) Surgical exposure of the facial nerve. J Laryngol Otol 72(11): 902-905.
- Byars LT (1952) Preservation of the Facial Nerve in Operations for Benign Conditions of the Parotid Area. Ann Surg 136(3): 412-419.
- Janes RM (1957) Tumors of the parotid gland. Ann R Coll Surg Engl 21(1): 1-20.
-
Islam MA, Rahman MM, Mohammad T, Kazi MM, Chowdhury NH, Rahman ASML, Milki FU. Convergence Technique is the Easy and Reliable Landmark for Identification of the Facial Nerve in Parotid Surgery. On J Otolaryngol & Rhinol. 5(4): 2022. OJOR. MS.ID.000619.
-
Parotid surgery, Facial nerve, Marginal mandibular nerve, Neurovascular structures, Sinuses, Parotid gland, Styloid process, Upper neck, Skull base, FNT.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.