 Research Article
Research Article
Using Regional Acceleratory Phenomenon andSimple Orthodontic Mechanics for the Management of Impacted Second Lower Molars: A Comprehensive Review
Andre Kon Kam King1*, Pierre Vives2, Dany Kon Kam King3 and Nikolaos Karvelas4
1Specialist in Orthodontics and Dentofacial Orthopedics, Director of the University Diploma of Orthodontic Aligners, University of Reunion, France
2Stomatologist, University Hospital Center of Reunion, Director of the University Diploma of Orthodontic Aligners, University of Reunion, France
3Specialist in Orthodontics, Department of Orthodontics, University of Medicine and Pharmacy “Grigore T. Popa”, Iasi, Romania
4PhD student, Department of Orthodontics, University of Medicine and Pharmacy “Grigore T. Popa”, Iasi, Romania
Andre Kon Kam King, Specialist in Orthodontics and Dentofacial Orthopedics, Director of the University Diploma of Orthodontic Aligners, University of Reunion, France.
Received Date: March 25, 2022; Published Date: April 20, 2022
Abstract
Introduction: Impaction of the lower second molars is quite rare ranging from 0 to 2.3% of the population and represents 0.03 to 0.04% of the overall dental impactions. This article aims to present and illustrate the simple orthodontic management approaches of the impaction of the lower second molars in synergy with Regional Acceleratory Phenomenon along with an overview of the main therapeutic options, their indications, and drawbacks.
Materials and methods: An unrestricted database search was conducted via PubMed, Ovid Medline and Google Scholar performed until January 2022.
Results: The main reason for the impaction or semi-impaction of the second lower molars is the lack of space in the posterior segment which may be necessary to evaluate the benefit/risk ratio at the beginning of impaction to perform the appropriate therapeutic option. Following a brief of the management along with the surgical and orthodontic protocol procedures, a new simplified orthodontic technique is presented combined with miniscrews.
Discussion: The simplified protocol proposed in this article is simple to perform orthodontically, quick, and effective to upright second mandibular impacted molar. A rapid outcome is obtained by maximizing the Rapid Acceleratory Phenomenon created by removal of the wisdom tooth, surgical exposure of the lower second molar, and the thin interseptal bone between the lower second molar and wisdom tooth. However, an experienced clinician is required for the MIs placement.
Conclusion: The contemporary evolution towards orthodontic treatments with a non-extraction protocol and with the benefit of the miniimplants will increase the therapeutic approaches along with the probabilities of easier molar uprighting in the impaction cases.
Keywords: Impaction; Mandibular second molars; Rapid Acceleratory Phenomenon
Introduction
Impaction of the lower second molars is quite rare ranging from 0 to 2.3% of the population [1]. According to Mead (1930) and Grover & Norton (1985) it represents the 0.03 to 0.04% of the dental impactions [2, 3]. However, modernization and the growing demand for therapeutic needs without any extractions make it imperative for the different uprighting aspects. Likewise, the distalization of the lower second molars can ensure the resolving of the crowding and the repositioning of the lower incisors in a non-extraction protocol, combining temporary anchorage devices (TADs) or aligners which can only highlight this allocation.
Correction of the impacted or semi-impacted teeth is even more challenging for the orthodontist when a dilemma arises regarding an optimistic error of estimation where time becomes quite critical. The clinician should make a difficult choice to finish or prolong the treatment in order to avoid the consequences linked to these difficulties. Some of the complications may occur as a risk for cavities, periodontal issues, the appearance of cysts, root resorption of the adjacent teeth, pain associated with the injury of the inferior alveolar nerve, and reduced masticatory function.
This article aims to present and illustrate the simple orthodontic management approaches of the impaction of the lower second molars in synergy with Regional Acceleratory Phenomenon (RAP) along with an overview of the main therapeutic options, their indications, and drawbacks.
Materials and Methods
An unrestricted database search was conducted via PubMed, Ovid Medline, and Google Scholar in order to identify articles that presented therapeutic management for impacted lower second molars. The strategy search was performed by 15 January 2022, with no language restrictions among the studies. Keywords as “impacted lower second molars”, “orthodontic treatment for included teeth”, “impaction of mandibular second molars”, “Regional Acceleratory Phenomenon” were used along with combinations of them. A total of 360 papers were found, in which finally only 33 articles were included in this review.
Results
Etiology and etiopathogenesis
The main reason for the impaction or semi-impaction of the second lower molars is the lack of space in the posterior segment according to Mead 1930 [2]. The germ of the second mandibular molar is often mesially positioned and can be self-uprighted following the resorption of the anterior border of the mandibular ramus, along with the mesial movement of the first molars by 2.7mm contributing equally [4].
Therefore, provide a better understanding of the repercussions of lack of early germectomy of the wisdom teeth in the sight of posterior crowding. Any therapeutic strategy preventing the mesial movement of the first molars will aggravate the case. In 1993 Kokich and Matthew suggested that treatment with a lingual arch or bumper can increase the odds of the eruption [5]. Similarly, contemporary aligners and miniscrews treatment can effectively distalize the first molars combined with elastic mechanics specifically in Class III patients, which will considerably worsen the result.
An alternative cause proposed by Eckhart involves the iatrogenic effects of the bands that sited on the first molars blocking the eruption of the second molars [6].
Alike, among other anatomical etiologies, Yoshikawa indicated [7]:
• A lack of guidance of the distal root due to an excessive
distance between first and second molars, which frequently
emerges after a premature loss of a temporary first molar [8].
• The absence of mesial drift of the first permanent molar due
to ankylosis of a deciduous molar
• Ectopic position of the follicle.
• The existence of an impediment on the eruption path like a
dentigerous cyst, odontoma, and supernumerary teeth [9].
Classification
According to the level of severity, the impaction can consist of mild, moderate, and severe [10]. An initial inclination of the second molar greater than 20°/ 24° or 30° is significantly associated with a high risk of impaction [1, 11].
Management
It may be necessary to evaluate the benefit/risk ratio at the beginning of an impaction, especially in the existence of proximity to the inferior alveolar nerve which may prevent further complications. In this case, is better to avoid any treatment option.
Extraction methods
The most common approach is the extraction of the second molar and its replacement by the third molar [12, 13]. This intervention can be indicated while following the criteria by Andreasen 1994 [14]:
1. The impacted second molar should be extracted only when the development of the crown of the third molar is completely finished
2. The third molar must be of normal shape and size
3. The third molar should be angled 15 to 30 degrees relative to the axis of the first molar and concerning the roots of the second molar.
Another option is the extraction of the second premolars and closing the distance with the mesial drift of the first molars, thus enchasing the necessary space for the eruption of the lower second molars. Nevertheless, conservative monitoring must precede respecting the above-mentioned complications. The option developed in this article includes extraction of wisdom tooth, surgical exposure, and uprighting of the lower second molar.
Conventional methods
A standard strategy after a surgical exposure is a Nickel- Titanium (Ni-Ti) archwire embedded in a molar tube and bypass the first molar avoiding excessive curvature of the wire [15]. Additional variants could be a 0.14 or 0.16 slightly compressive (U-shaped) NiTi wire with a stop mesial to the second molar tube and a stop distal to the first molar tube or bonded on a miniscrew head which is placed mesial to the first molar.
An alternative and typical method is the use of a stainless-steel wire between the first molar band and the tube on the second molar and an open coil spring compressed between these two adjacent teeth in order to upright and tip distally the second lower molar [16].
Furthermore, uprighting springs made of Titanium Molybdenum Alloy (TMA) sectional cantilever loops can be used to upright and align the impacted tooth [13].
Simplified Miniscrew method
In 1990 Roberts et al described the use of an implant in the retromolar region, which delivers good stability due to the extremely dense cortical bone [17]. In 1996, Shellart proposed the first osseointegrated implant for the uprighting of the second molar [18]. In addition, Park has suggested a microscrew in the retromolar area to upright the second molar with a distalization force of an elastomeric thread of 50-80 grams [19]. In 2004, Giancotti used a Titanium Miniscrew with a closed NiTi coil spring of 50 g reactivated monthly which conducted an average of 7-9 months treatment [20]. In 2007, Lee and al suggested the use of an elastomeric power chain [21]. Later, Chang and Lin JJ presented a 2 mm diameter stainless steel miniscrew (MIs), which is less brittle and with no need of pilot predrilling, suitable in the retromolar area [22, 23].
Some drawbacks of placing mini-implants in the retromolar area can include inflammation, mucosa swelling as well as the difficulty of insertion of MIs in the mandible from an inexperienced clinician to avoid any unnecessary damage. Moreover, excellent oral hygiene and sometimes a gingivectomy is required. Nevertheless, the elastomeric power chain is preferred to the closed NiTi coil spring.
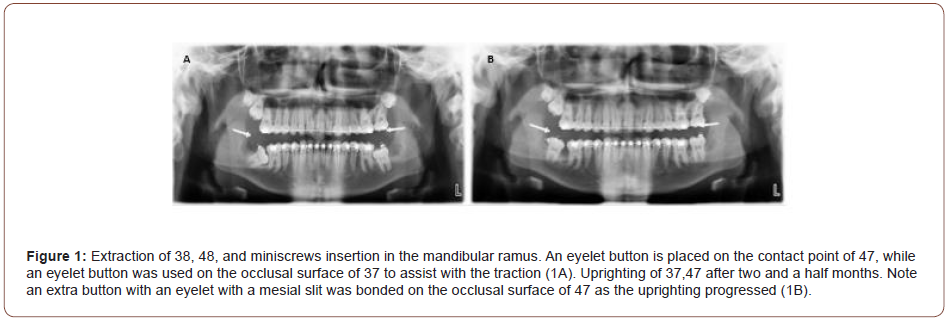
Preparation time can be carried out in one appointment, divided into surgical and orthodontic time. The surgical period includes the extraction of the wisdom teeth, surgical exposure of mandibular second molar, and miniscrew placement at the ascending ramus, while orthodontic time includes the bonding of the lingual button as mesial as possible on the occlusal surface of the second lower molar and the activation with the power chain from the miniscrew head to the bonded button (Figure 1). The two-steps procedure consists of bonding a lingual button and performing the orthodontic activation in the office a few days after surgery. However, precautions undergo that the head of the miniscrew is well exposed outside the mucosa to allow easy elastic power chain insertion and to ensure the dry working field surrounding the second molar with laser or electrosurgical unit for proper bonding protocol.
Autotransplantation
Auto-transplantation can be selected as a therapeutic approach in the matter of a failure of orthodontic alignment or because the patient refuses conventional orthodontic treatment [24]. However, it is linked with crucial potential complexities such as the loss of pulpal vitality, loss of periodontal attachment even as root resorption and ankylosis [25].
Surgical exposure and uprighting
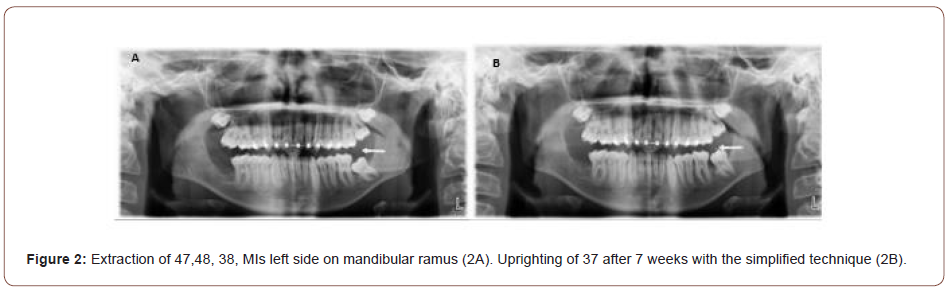
Orthodontic-surgical treatment involves removing the wisdom tooth and surgically exposing the crown of the impacted second molar to bond a button or an eyelet. The simplified version of this method by adding a TAD has the advantage to treat severe impactions particularly when the impacted tooth is quite close to the inferior nerve, in order to avoid any complication linked to its extraction [13, 26]. Thus, this modern approach does not require anchorage anterior to the impacted tooth and as a result, there is no parasitic effect on the lower arch or the occlusion (Figure 2).
Surgical protocol
Miniscrew insertion: Cone Beam CT aims to locate the mandibular canal and its relationship with the wisdom teeth along with the second molar. Its purpose is to assess the difficulty of the extraction and the level of severity of the impaction. It also allows, to determine the quantity of bone available for placement of the MIs as well as the distance of the mandibular canal from the bony edge, to evaluate the depth for the insertion of MIs without damaging the inferior alveolar nerve. Extraction of the third molar followed by surgical uprighting of the second lower molar ensures the absence of ankylosis [27].
Placement of MIs is proposed of 14mm and 2mm (OBS) diameter [28]. As described, the MIs are placed on the anterior border of the ascending ramus so that the MIs head can be exposed through the mucosa, thus providing 5 mm of clearance to attach an elastic power chain properly. A 2 mm diameter is the most appropriate for good stability [26].
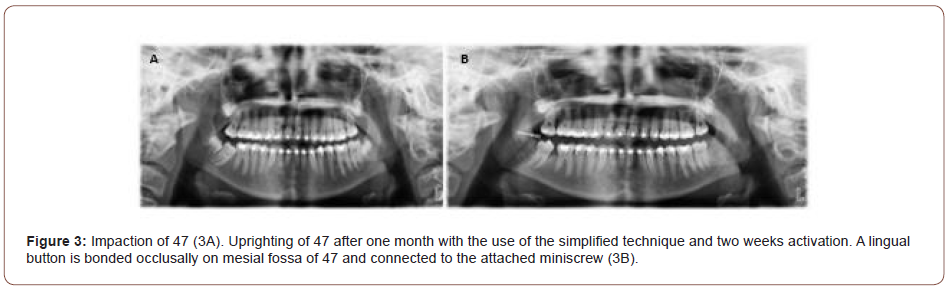
The optimal position of MIs head is to obtain a pulling force as parallel as possible to the occlusal surface of the second molar. This orientation allows a distal and occlusal force around the center of resistance of the second molar and as a result an easy and rapid uprighting of the impacted tooth right from the start of treatment (Figure 3).
On the other hand, positioning the MIs higher on the ramus could cause possible occlusal interference with the maxillary second molar. In case the MIs head is too horizontal concerning the occlusal plane, the elastic power chain could be dislodged easily but nevertheless, a flowable composite material may occasionally support it.
Orthodontic protocol
The operative field should be dry, a surgical suction and a fourhanded work are particularly recommended. In the presence of a severe impaction with mesioinclination of the second molar, a traction hook or a lingual button with an eyelet with a mesial slit must be bonded on the distal marginal fossa or on the distal contact point of the impacted molar.
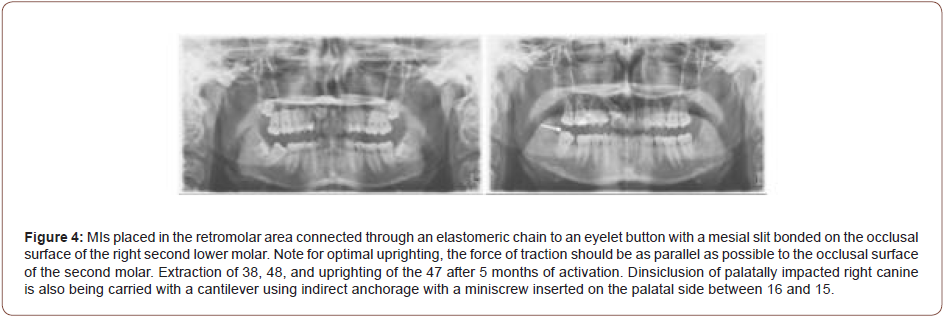
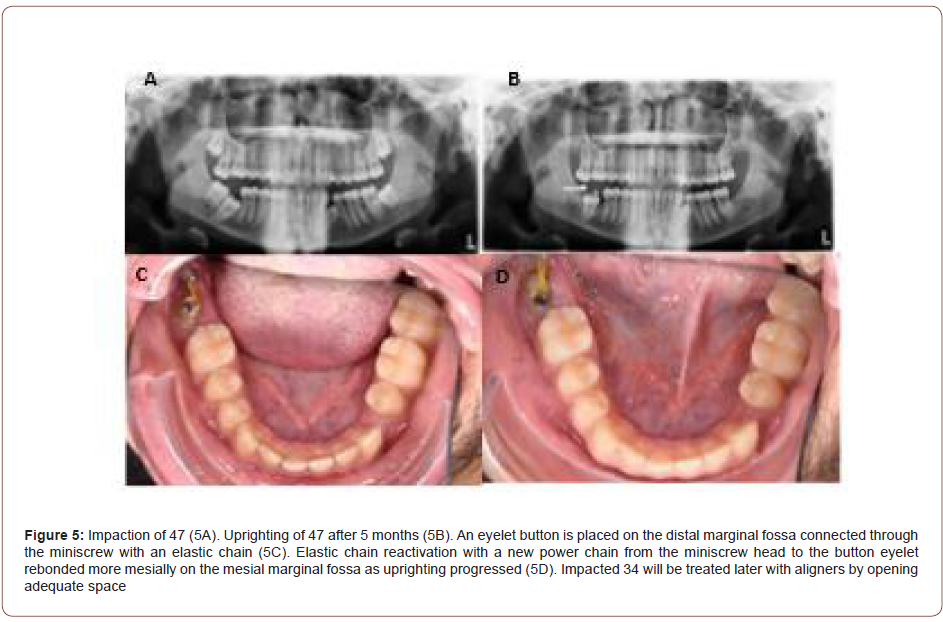
In patients with moderate or mild issues, these auxiliaries will be bonded as mesially as possible on the occlusal surface (Figures 4, 5). The auxiliary eyelet with a mesial slit provides better anchorage for the elastomeric power chain than the lingual button.
Etching is carried out with phosphoric acid 35%, then rinsing with water syringe, drying followed by Orthosolo bond agent, and then the button is glued using a 3M Rely X Unicom Civomer lightcured with a Valo UV lamp allowing a faster setting.
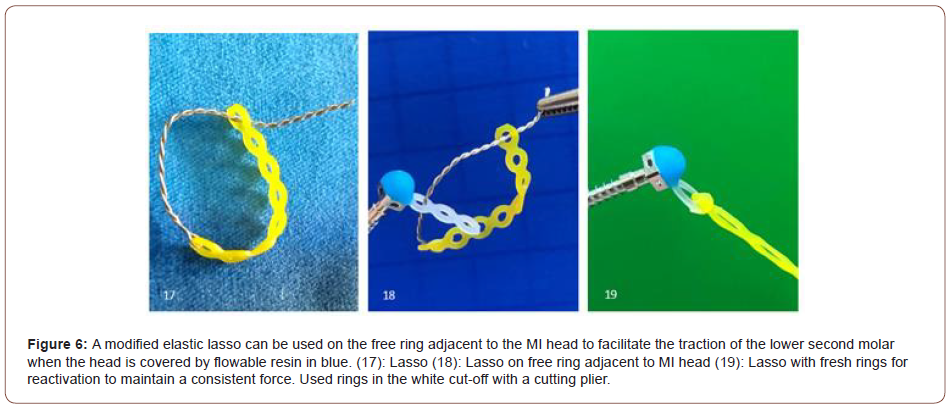
Attachment eyelet
The elastic power chain will be stretched from the head of the MIs to the traction hook or the mesial eyelet with an average of 200 to 250 grams to acquire an average constant force of 100-125 grams after decay [27-29]. The reactivation will take place every three weeks, taking advantage of the RAP caused by extraction of the wisdom tooth, surgical exposure of the lower second impacted molar, and the thin interseptal bone between lower second molar and wisdom tooth Liou [30, 31]. A new elastic power chain at every appointment is necessary to maintain a constant force. In the case where the MIs head is covered with flowable resin, a modified elastic lasso can be used on the free ring adjacent to the MIs head to facilitate the traction (Figure 6). On the other hand, when the MIs head is covered by the mucosa, the elastic lasso will be attached to the ring still exposed out of the mucosa. Uprighting results were obtained on an average of 3-4 months.
Discussion
In the cases of impacted second lower molars, the alternatives include extraction of premolar along with mesialization of the first and second molar, extraction of the impacted tooth, extraction of the third molar and uprighting of the second molar, and autotransplantation of the second lower molar depending on the feasibility of each treatment option. The factor guiding this selection is the severity of the impaction, its anatomical relationship, the surgical difficulty, crown and root formation of the teeth concerned, and the patient’s age. It is critical to make an early diagnosis to be able to serve within the optimal time and thereby reducing treatment and the potential complications [32].
For surgical-orthodontic uprighting, the literature describes a wide spectrum of methodologies with the advantages and weaknesses of each.
The simplified protocol proposed in this article is simple to perform orthodontically, quick, and effective to upright second mandibular impacted molar. A rapid outcome is obtained by maximizing the RAP created by removal of the wisdom tooth, surgical exposure of the lower second molar, and the thin interseptal bone between the wisdom tooth and the lower second molar. However, an experienced clinician is required for the MIs placement. In addition, it resolves the impaction without generating any parasitic effect. Placement of a 14mm MI at the beginning of the surgical procedure on the mandibular ramus, is highly recommended by Chang and Lin SY by placing the MI head in the mucosa in a less inflammatory field which is particularly beneficial for rapid and painless removal of the elastomeric chain for its reactivation [26, 28]. Nevertheless, this method cannot be indicated when the mandibular second molar is in a high position relative to the occlusal plane.
The use of a NiTi closed spring coil suggested by Necka, et al. requires a minimum distance between the screw head and the button. One drawback of this method is that the tension may not be constant when this distance is considerably decreased especially at the end of treatment. In addition, impeccable hygiene is mandatory in an area where it is quite difficult to clean. The elastomeric thread suggested by Park will be more challenging to reactivate to receive constant force due to complicated manipulation in a limited posterior segment with inflammation and bleeding [19]. This operation becomes even more problematic when the thread is buried into the inflamed mucosa, which may frequently require gingivectomy. The usefulness of an average of 100-125 grams as persistent as possible is advised taking into account the decay of the power chain over time and saliva. Taking advantage of the RAP during the first four months consequent to the extraction of the wisdom tooth among the coronal clearance of the second molar, and the thin interseptal bone distal to the lower second molar, the overall treatment time may be considerably shortened.
The elastic power chain qualifies as a more comfortable and systematic change during reactivation. The power chain can be adjusted every three weeks, to compensate for the force loss due to decay. However, Sivolella, et al. suggested an elastic change every two weeks which seems an interesting road of investigation [33]. It can be explained with a slightly quicker correction time of approximately 2-4 months. The eyelet button with a mesial slit placed mesially stimulates more profitable power chain retention on the crown side and therefore facilitates its reactivation over the classic lingual button in which the power chain can be disinserted during chewing.
In the case of gingival hypertrophy, an elastic lasso is recommended, as it provides an easy, rapid, and painless method of preserving a steady tractive force.
In addition, this method can be accomplished during the retention phase without any effect on the occlusion. The alignment of the lower second molar can be completed with an active aligner on the affected tooth. Another option could be the application of segmented partial brackets on the first and second molar while maintaining the anchorage with a lingual arch, passive splint, or any other form of stabilization.
Conclusion
The contemporary evolution towards orthodontic treatments with a non-extraction protocol and with the benefit of the miniimplants will increase the therapeutic approaches along with the probabilities of an easier molar uprighting in the impaction cases.
The clinician will turn to the simplest and most predictive treatment possible. It could be interesting to integrate this simplified orthodontic technique proposed among our therapeutic tools, because it has the advantage of treating the impacted mandibular second molar in any type of severity from mild, moderate, to severe impactions while respecting anchorage. The simplified method defined in this study appears to significantly reduce the treatment time.
All these factors should be taken into consideration to provide the best treatment plan without jeopardizing the patients while all the results should be interpreted with caution.
Acknowledgement
None.
Conflict of interest
The authors state there is no conflict of interest.
References
- Cassetta M, Altieri F (2017) The influence of mandibular third molar germectomy on the treatment time of impacted mandibular second molars using brass wire: A prospective clinical pilot study. Int J Oral Maxillofac Surg 46(7): 905-911.
- Mead S (1930) Incidence of impacted teeth. International J Orthodontics 16: 885-890.
- Grover PS, Norton L (1985) The incidence of unerupted permanent teeth and related clinical cases. Oral Surg Oral Med Oral Pathol 59: 420-425.
- Majourau A, Norton LA (1995) Uprighting impacted second molars with segmented springs. Am J Orthod Dentofacial Orthop 107: 235-238.
- Kokich VG, Mathews DP (1993) Surgical and orthodontic management of impacted teeth. Dent Clin North Am 37: 198-201.
- Eckhart JE (1998) Orthodontic uprighting of horizontally impacted mandibular second molars. J Clin Orthod 32: 621-624.
- Yoshikawa K, Ohga N, Satoh C, Sato J, Kitagawa Y (2018) Surgical extrusion of completely impacted mandibular second molars: A technical case report with 3 years clinical and radiographic follow-up. Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology 30(5): 409-412.
- Shapira Y, Borell G, Nahlieli O, Kuftinec MM (1998) Uprighting mesially impacted mandibular permanent second molars. Angle Orthod 68: 173-178.
- Frank C (2000) Treatment options for impacted teeth. J Am Dent Assoc 131: 623-632.
- Lau CK, Whang CZ, Bister D (2013) Orthodontic uprighting of severely impacted mandibular second molars. Am J Orthod Dentofacial Orthop 143(1): 116-124.
- Cassetta M, Altieri F, Di Mambro A, Galluccio G, Barbato E (2013) Impaction of permanent mandibular second molar: A retrospective study. Med Oral Patol Oral Cir Bucal 18(4): e564.
- De-la-Rosa-Gay C, Valmaseda-Castellón E, Gay-Escoda C (2006) Spontaneous third-molar eruption after second-molar extraction in orthodontic patients. Am J Orthod Dentofacial Orthop 129(3): 337-344.
- Mah M, Takada K (2016) Orthodontic management of the impaction of the second mandibular molar. French Orthodontics 87(3): 301-308.
- Andreasen JO, Håkanson L, Buckhöj P, Acevedo A, Chardin H (1994) Atlas of dental reimplantation and transplantation. Barcelona; Milan; Paris; Masso.
- Going RE, Reyes-Lois DB (1999) Surgical exposure and bracketing technique for uprighting impacted mandibular second molars. J Oral Maxillofac Surg 57: 209-212.
- Pogrel MA (1995) The surgical uprighting of mandibular second molars. Am J Orthod Dentofacial Orthop 108: 180-183.
- Roberts WE, Marshall KJ, Mozsary PG (1990) Rigid endosseous implant utilized as anchorage to protract molars and close an atrophic extraction site. Angle Orthod 60(2): 135-152.
- Shellhart WC, Moawad M, Lake P (1996) Implants as anchorage for molar uprighting and intrusion. Angle Orthodontics 66(3): 169-72.
- Park HS, Kyung HM, Sung JH (2002) A simple method of molar uprighting with microimplant anchorage. J Clin Orthod 36: 592-596.
- Giancotti A, Arcuri C, Barlattani A (2004) Treatment of ectopic mandibular second molar with titanium miniscrews. Am J Orthod Dentofacial Orthop 126: 113-117.
- Lee KJ, Park YC, Hwang WS, Seong EH (2007) Uprighting mandibular second molars with direct miniscrew anchorage. J Clin Orthod 41: 627-635.
- Chang CH, Roberts WE (2013) A retrospective study of the extra-alveolar screw placement on buccal shelves. Int J Orthod Implantol 32: 80-89.
- Lin John Jin- Jong (2017) Creative Orthodontics Blending the Damon System and TADS to Manage Difficult Malocclusions. (3rd Edn) Scala Printing Co., Ltd, Taiwan, pp: 131.
- Huth KC, Nazet M, Paschos E, Linsenmann R, Hickel R, et al. (2013) Autotransplantation and surgical uprighting of impacted or retained teeth: a retrospective clinical study and evaluation of patient satisfaction. Acta Odontologica Scandinavica 71(6): 1538-1546.
- Jang Y, Choi YJ, Lee SJ, Roh BD, Park SH, et al. (2016) Prognostic factors for clinical outcomes in autotransplantation of teeth with complete root formation: survival analysis for up to 12 years. Journal of endodontics 42(2): 198-205.
- Lin Shih-Yung, Simple Mechanics to Upright Horizontally Impacted Molars with Ramus Screws, Dr Shih-Yung Lin, Dr Chris Chang, W Eugene Roberts 1IBOI Diplomate, 2 Founder, Beethoven Orthodontic Center, Publisher, International Journal of Orthodontics & Implantology, 3 Consultant, International Journal of Orthodontics & Implantology 2015.
- André Weissheimer, Arno Locks, Luciane Macedo de Menezes, Adriano Ferreti Borgatto, Carla D’Agostini (2013) Vitro evaluation of force degradation of elastomeric chains in Orthodontics. Dental Press J Orthod 18(1): 55-56.
- Chang C, Lin SY, Roberts WE (2016) Forty consecutive ramus bone screws used to correct horizontally impacted mandibular molars. Int J Orthod Implantol 41: 60-72.
- Murphy C, Kalajzic Z, Chandhoke T, Utreja A, Nanda R (2016) The effect of corticision on root resorption with heavy and light forces. Angle Orthod 86: 17-23.
- Liou EJW, Huang CS (1998) Rapid canine retraction through distraction of the periodontal ligament. Am J Orthod Dentofacial Orthop 114(4): 372-382.
- Anthony A Vargas, Daniel B Bruin, Michael J Stewart, Jake T Wilding, Daniel D Dunham, et al. (2021) Utilizing the Regional Acceleratory Phenomenon and Dental Implant Anchorage for Distalization and Intrusion of a Mesially Tipped Mandibular Molar: A Case Report. Clin Adv Periodontics 11(1): 4-10.
- Berdah Dylan (2018) Orthodontic management of impacted or impacted second molars. THESIS Presented and publicly defended before the Faculty of Odontology of Marseille University Le.
- Stefano Sivolella, Michela Roberto, Paolo Bressan, Eriberto Bressan, Serena Cernuschi et al. (2012) Uprighting of the Impacted Second Mandibular Molar with Skeletal Anchorage, University of Padua, Departments of Oral Surgery and Orthodontics Italy.
-
Andre Kon Kam King, Pierre Vives, Dany Kon Kam King and Nikolaos Karvelas. Using Regional Acceleratory Phenomenon and Simple Orthodontic Mechanics for the Management of Impacted Second Lower Molars: A Comprehensive Review. On J Dent & Oral Health. 5(4): 2022. OJDOH.MS.ID.000619. DOI: 10.33552/OJDOH.2022.05.000619.
-
Orthodontic mechanics, Orthodontically, Tooth, Orthodontic management, Teeth, Odontoma, Wisdom tooth, Second molar, Inflammation and bleeding
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






