 Case Report
Case Report
Treatment of Esthetic Sequelae of Peripheral Ossifying Fibroma with Suine Collagen Matrix-Case Report
Manfro R1, García GFF2, Poubel VLN3, Gondak RO4, Souza VZ5* and Silva LR6
1Federal University of Santa Catarina, Florianópolis, Santa Catarina, Brazil
2University of Southern Santa Catarina, Palhoça, Santa Catarina, Brazil
3Catholic University of Brasilia, Federal District, Brasilia, Brazil
4Federal University of Santa Catarina, Florianópolis, Santa Catarina, Brazil
5University of Passo Fundo, Passo Fundo, Rio Grande do Sul, Brazil
6University of the West of Santa Catarina, Joaçaba, Santa Catarina, Brazil
Vilton Zimmermann de Souza, University of Passo Fundo, Passo Fundo, Rio Grande do Sul, Brazil.
Received Date: August 17, 2022; Published Date: September 01, 2022
Abstract
The aim of this study is report the treatment of a case of a peripheral ossifying fibroma. In this case report, we present the clinical course of a 23-year-old female patient with a mass in the gingival tissue. The patient was submitted to excisional biopsy and the defect generated by the removal of the lesion was corrected using biomaterials. One year of follow-up, it was not possible to see any esthetic defect when compared with the contralateral side.
Keywords: Dentistry; Stomatology; Case report
Introduction
Benign gingival lesions usually have good prognosis and management is easily performed. The main problem is lesions situated in anterior maxillary areas. Although technically easy, resection can cause esthetics problems, and treatment is hard to accomplish [1].
There are three categories to bone fibrous lesions. The first one is fibrous dysplasia, followed for reactive lesions and ossifying fibroma neoplasms. Reactive lesions can be categorized as central and peripheral [2]. Peripheral lesions originate from cells located in periodontal ligament and central lesions comes from the endosteum.
Peripheral Ossifying Fibroma (POF) is a reactional lesion that use to appear in the attached gingiva of young women. Its prevalence is 3,1% of all oral tumors and 9,6% of all gingival lesions [3]. The etiology is thought to be originated from an irritating factor, such as plaque, calculus, trauma, misfit prosthesis, dental restorations, and microorganisms [4-6]. There are two theories postulated to understand the etiology. The first one postulates that the lesion initiates as a pyogenic granuloma that becomes calcified. The other one postulates that the lesion originates from an inflammatory hyperplasia of periodontal ligament [4].
Size use to be less than 1,5cm in its biggest part, and its clinical manifestation include sometimes pain, and could cause teeth displacement depending on the size of the lesion [7]. Histologically presents as a fibroblastic proliferation with ossification spots [4].
Normally, treatment is accomplished with surgical excision and local factors removal. Periodontal ligament and periosteum should be also removed to increase the success and reduce recurrence rate [8].
The main objective of this paper is to present a case report of peripheral ossifying fibroma in the anterior region of the maxilla treated with excision and reconstruction with supine collagen matrix.
Case Report
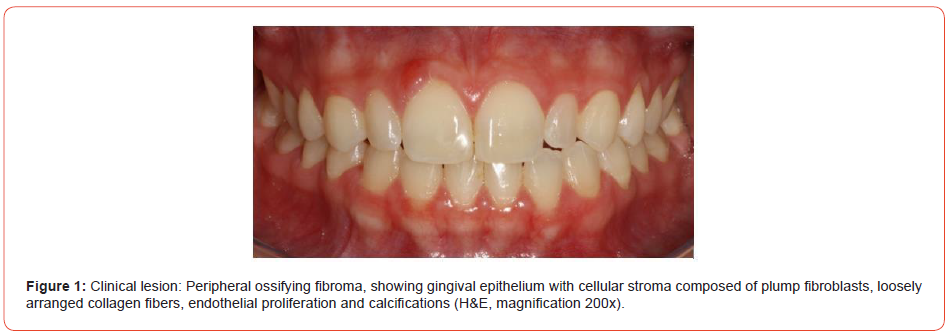
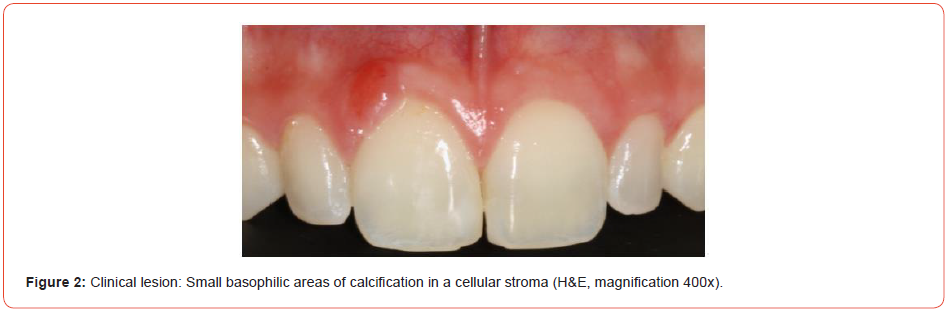
A 23-year-old female was presented to the maxillofacial consultation at Private Clinical in Florianopolis, Santa Catarina, Brazil, with a mass in the gingival tissue. It was painless and it was possible to detect a sessile exophytic lesion located above the right central incisor measuring 3 X 2 X 1,1cm, without changes in color, indurations, or ulcerations. There was no tooth displacement. The mass appeared 5 months before the analysis and had gradually increased in size (Figures 1, 2).
Previously to the excisional biopsy, it was explained to the patient the necessity to remove an additional amount of tissue as a safe margin to avoid recurrences. As well, it was also explained that due to the location of this lesion, it would be necessary to reconstruct at the same time the gingival tissue with bovine collagen matrix.
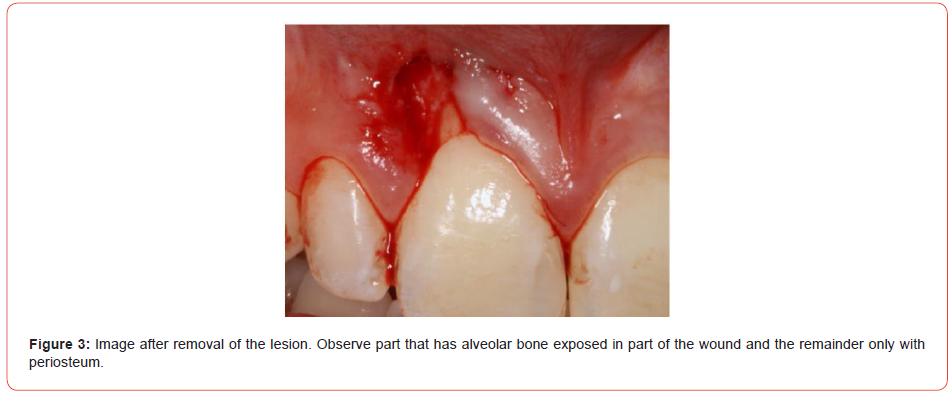
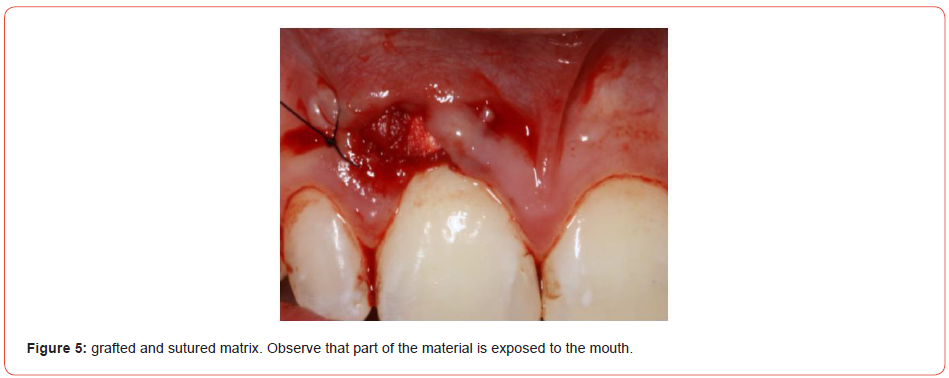
The procedure was performed under local anesthesia using Articaíne 4% with adrenaline 1:100.000. Alveolar superior anterior nerve was blocked using 0,8mL of solution. With a 15C blade, it was done an incision around the lesion and using a proper instrument the lesion was detached. The surgical site was compound with and without periosteum covering alveolar bone (Figure 3). With the aim to avoid a bigger defect and leave exposed bone, it was realized a gingival reconstruction with bovine collagen matrix (Figure 4). This graft was enveloped in the edge of the defect and sutured with mononylon 5-0 with the reminiscent gingival (Figure 5).

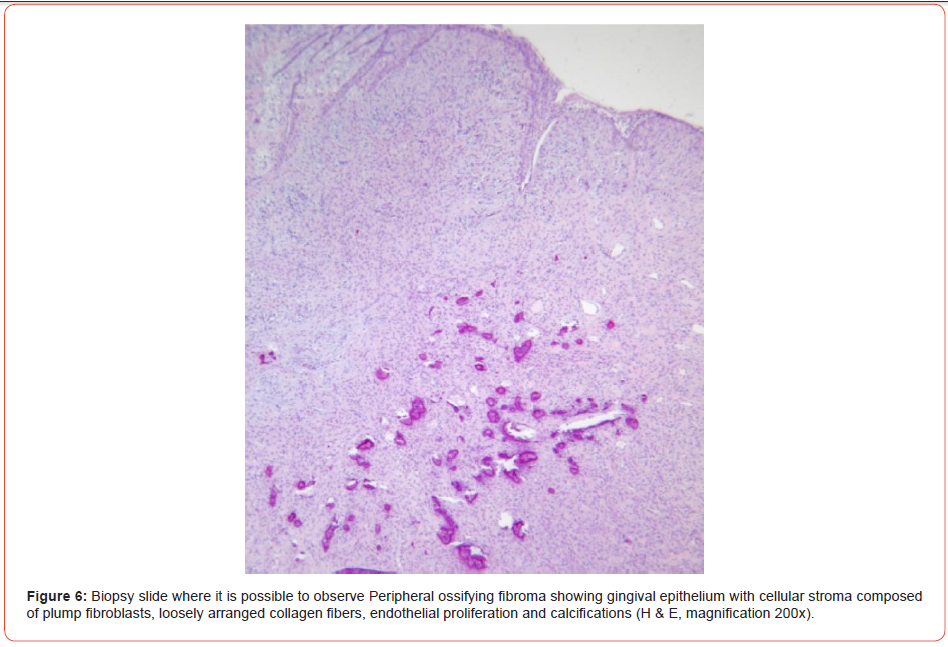
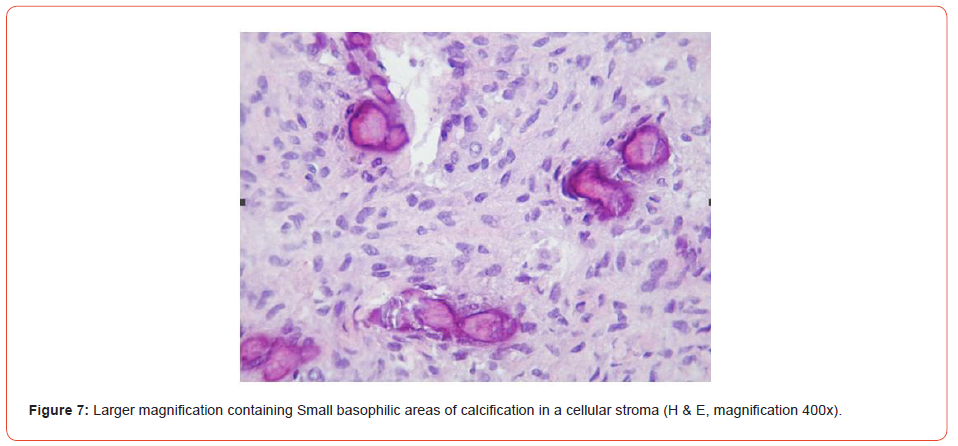
The material was sent to the Buccal Pathology Laboratory situated at the Federal University of Santa Catarina, Brazil. Histologically, the specimen showed an intact gingival epithelium overlying the connective tissue stroma (Figure 6). The connective tissue was densely fibro cellular with endothelial proliferation and several irregular basophilic calcified areas (Figure 7). A mild chronic inflammatory infiltrate was noted into the lamina propria. Based on histological findings, the lesion was diagnosed as peripheral ossifying fibroma.
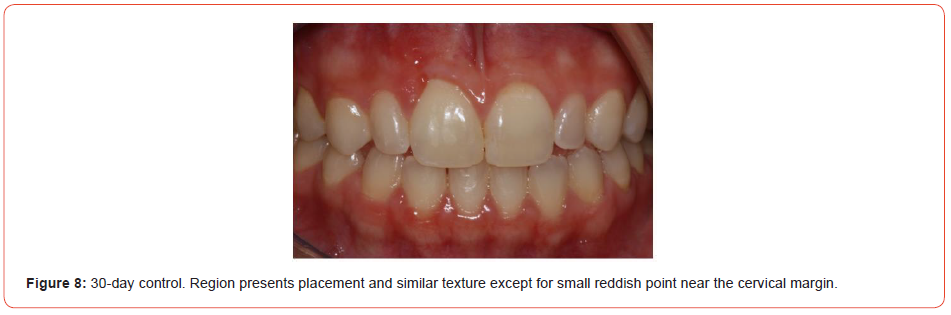
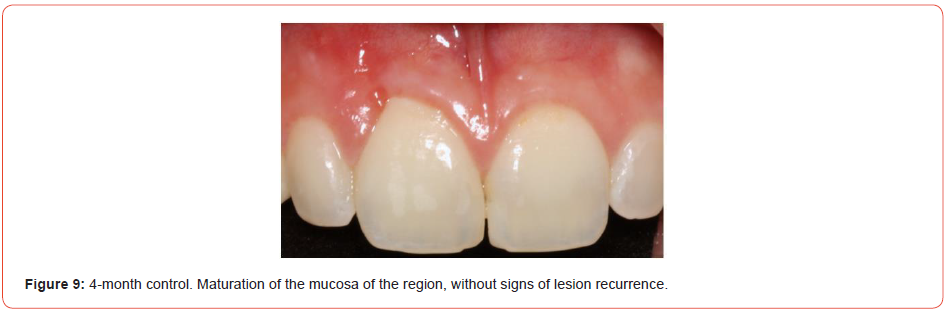
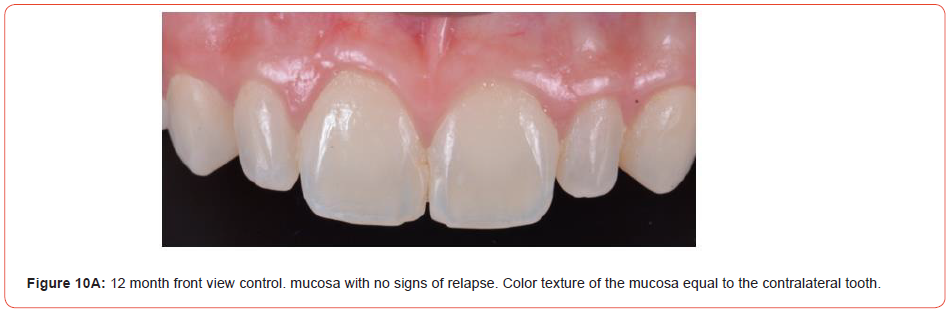
The knots were removed after 10 days of surgical procedure. Hygiene was conducted with flexible cottons embedded with Di gluconate of chlorhexidine 0,12%. In the 30th day of follow-up, it was observed a partial substitution of the graft for health gingiva without clinical evidence of acute inflammation (Figure 8). After 4 months the surgical site presented as health gingiva without defect and with the color as pink as the adjacent ones (Figure 9). One year of follow-up, it was not possible to see any esthetic defect when compared with the contra-lateral incisor (Figures 10A, 10B).

Discussion
Peripheral ossifying fibroma (POF) is a lesion which is easily treated and has a good prognosis when periosteal resection is included in treatment plan. Recurrence rate varies from 2 to 9% according to literature [4, 9-12]. As mentioned previously, the main problem concerning this treatment is lesions located in anterior region, which brings a poor esthetic outcome. Furthermore, other issues are possible like radicular exposition, dentinary hyper sensibility and impossibility of hygiene maintenance.
Other question that must be discussed previously is the reconstruction time. Many authors would rather await for initial healing to detect the real damage extension [13]. Another group defends that begin lesion with low risk of recurrence should be treated with reconstruction at the same time of surgery. Though, the last ones try to avoid damages to the adjacent structures [14].
Many techniques have been proposed in literature with the goal to avoid these poor esthetics outcomes as subepithelial connective tissue graft (SCTG) or a coronally positioned flap (CPF), laterally positioned flap (LPF). CPF has a high success rate, although it cannot be realized in regions with an insufficient amount of quarantined tissue and also it cannot be realized in the presence of a very short vestibule. SCTG needs a donor site, and this technique is too sensitive. LPF seems to be a good alternative [1, 8].
Mucograft (MG) is a collagen matrix composed of type I and III porcine collagen without cross-linking or chemical treatment. It has two layers, one is thin and the other one is smooth compact [15]. Studies evaluating the behavior of this material have demonstrated minimal inflammation and absence of multinucleated giant cells, as well as a high success rate for reconstruction of bone defects [16, 17]. Some authors have stated that resorbable collagen membrane (RCM) used to guide bone regeneration has been better than MG [15, 18].
In this case report presented the authors decided to use a simultaneous reconstruction using xenogeneic graft with aim to protect the surgical area. The expectancy after this procedure was to reconstruct the residual defect using a autologous graft from the palate, due the lack of evidence in literature about the results achieved with this material. But, after following up the patient, it was able to see an excellent outcome. In the first months the results were promisor and after 4 months the second time reconstruction was rejected, because there were no signs of sequelae, which was confirmed after 12 months of follow up.
This paper hypothesized that xenogeneic gingival matrix could be a good choice for primary reconstruction of tumors located on anterior region of the maxilla, which avoids a later reconstruction and improves the prognosis.
Summary
The objective of this work is to report the treatment of a case of peripheral ossifying fibroma. In this case report, we present the clinical evolution of a 23-year-old female patient with a mass in gingival tissue. The patient underwent excisional biopsy and the defect generated by the removal of the lesion was corrected with biomaterials. After one year of follow-up, it was not possible to observe any aesthetic defect when compared to the contralateral side.
Acknowledgement
None.
Conflict of interest
No Conflict of Interest.
References
- Bosco AF, Bonfante S, Luize DS, Bosco JM, Garcia VG (2006) Periodontal plastic surgery associated with treatment for the removal of gingival overgrowth. J Periodontol 77: 922-928.
- Franco-Barrera MJ, Zavala-Cerna MG, Fernandez-Tamayo R, Vivanco-Perez I, Fernandez-Tamayo NM, et al. (2016) An update on peripheral ossifying fibroma: case report and literature review. Oral Maxillofac Surg 20: 1-7.
- Salaria SK, Gupta N, Bhatia V, Nayar A (2015) Management of residual mucogingival defect resulting from the excision of recurrent peripheral ossifying fibroma by periodontal plastic surgical procedure. Contemp Clin Dent 6: S274-S277.
- Barot VJ, Chandran S, Vishnoi SL (2013) Peripheral ossifying fibroma: A case report. J Indian Soc Periodontol 17: 819-822.
- Kashyap B, Reddy PS, Nalini P (2012) Reactive lesions of oral cavity: A survey of 100 cases in Eluru, West Godavari district. Contemp Clin Dent 3: 294-297.
- Eversole LR, Rovin S (1972) Reactive lesions of the gingiva. J Oral Pathol 1: 30-38.
- Sacks HG, Amrani S, Anderson K (2012) "Gigantiform" peripheral ossifying fibroma: report of a case. J Oral Maxillofac Surg 70: 2610-2613.
- Walters JD, Will JK, Hatfield RD, Cacchillo DA, Raabe DA (2001) Excision and repair of the peripheral ossifying fibroma: a report of 3 cases. J Periodontol 72: 939-944.
- Mishra AK, Maru R, Dhodapkar SV, Jaiswal G, Kumar R, Punjabi H (2013) Peripheral cemento-ossifying fibroma: A case report with review of literature. World J Clin Cases 1: 128-133.
- Mishra MB, Bhishen KA, Mishra S (2011) Peripheral ossifying fibroma. J Oral Maxillofac Pathol 15: 65-68.
- Khan FY, Jan SM, Mushtaq M (2013) Multicentric peripheral ossifying fibroma: A case report and review of the literature. J Indian Soc Periodontol 17: 648-652.
- Hunasgi S, Raghunath V (2012) A clinicopathological study of ossifying fibromas and comparison between central and peripheral ossifying fibromas. The journal of contemporary dental practice 13: 509-514.
- Kumar R, Jaiswal S, Sharma A, Andhare V, Sabir H (2015) Peripheral odontogenic fibroma: a rare gingival neoplasm with clinico-pathological differential diagnosis. J Exp Ther Oncol 11: 17-21.
- Zhu YQ, Wang YQ, Tang YC, Li CZ (2016) Initial periodontal therapy for the treatment of gingival pregnancy tumor. Genet Mol Res 15.
- Ramalingam S, Babay N, Al-Rasheed A, Amani Basudan, Nasser Nooh, et al. (2016) Efficacy of Mucograft vs Conventional Resorbable Collagen Membranes in Guided Bone Regeneration Around Standardized Calvarial Defects in Rats: A Histologic and Biomechanical Assessment. Int J Periodontics Restorative Dent 36 Suppl: s99-s107.
- Cioban C, Zaganescu R, Roman A, A Muste, F Beteg, et al. (2013) Early healing after ridge preservation with a new collagen matrix in dog extraction sockets: preliminary observations. Rom J Morphol Embryol 54: 125-130.
- Ghanaati S, Schlee M, Webber MJ, Ines Willershausen, Mike Barbeck, et al. (2011) Evaluation of the tissue reaction to a new bilayered collagen matrix in vivo and its translation to the clinic. Biomed Mater 6: 015010.
- Babay N, Ramalingam S, Basudan A, Nasser Nooh, Mohammed Al-Kindi, et al. (2016) Efficacy of Mucograft vs Conventional Resorbable Collagen Membranes in Guided Bone Regeneration Around Standardized Calvarial Defects in Rats: An In Vivo Microcomputed Tomographic Analysis. Int J Periodontics Restorative Dent 36 Suppl: s109-121.
-
Manfro R, García GFF, Poubel VLN, Gondak RO, Souza VZ* and Silva LR. Treatment of Esthetic Sequelae of Peripheral Ossifying Fibroma with Suine Collagen Matrix-Case Report. On J Dent & Oral Health. 6(2): 2022. OJDOH.MS.ID.000631. DOI: 10.33552/OJDOH.2022.06.000631.
-
Peripheral ossifying fibroma, Maxillary areas, Gingival lesions, Periodontal ligament, Gengival reconstruction, Biomaterials, Gingival tissue, Reconstruction of tumors, bone regeneration, Giant cells
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






