 Mini Review
Mini Review
The TMJ: Gateway to the Airway
Jeff Paz, D.D.S.*
Diplomate American Board Dental Sleep Medicine, Co-Founder, Sleep Apnea Gurus, USA
Jeff Paz, D.D.S., Diplomate American Board Dental Sleep Medicine, Co-Founder, Sleep Apnea Gurus, USA.
Received Date: December 07, 2021; Published Date: January 17, 2022
Mini Review
Close to 1 billion people have OSA, according to the World Health Organization. A couple of treatment options for such breathing problems involve the use of an oral appliance and/or CPAP. These appliances help to open the user’s breathing passage more fully to allow easier breathing through the user’s nose and mouth. As technology advances, people with breathing problems demand increased clinical outcomes and comfort. Previous appliances for improving breathing include custom masks connected to an associated oral appliance. Such an oral appliance may extend the user’s lower jaw forward to open the breathing passage, while the mask allows air or another gas to be delivered to the user’s nose at positive pressure to further open the breathing passage. Previous masks have often failed due to poor fit to the patient’s facial structure. Consequently, previous masks have failed to adequately prevent leakage from around the perimeter of the mask, resulting in discomfort to the user, and not treating breathing problems such as snoring and sleep apnea. As a result of these and other deficiencies, previous masks are inadequate for the needs of many users who experience breathing difficulties.
Perhaps dentists can increase their knowledge on the plethora of treatments for OSA, and specifically, positive airway pressure (PAP). Dentists will benefit if they understand how they can assist and team up with physicians. Similarly, physicians should recognize the putative role of the temporomandibular joint (TMJ) and mandibular stabilization - its proper positioning can be critical for optimal PAP therapy. National statistics on PAP compliance have shown discouraging results, with nightly utilization as low as 51% in some studies but up to 80% in others. One of the chief complaints by patients and clinicians is failing to recognize proper interface or mask fit. One possible solution is combining PAP therapy and oral appliance therapy. With hybrid therapy, many of the challenges of PAP intolerance can be improved, resulting in better clinical outcomes. Hybrid therapy utilizes a standard PAP machine to deliver positive air pressure through a standard nasal and/or oronasal interface in conjunction with an oral appliance. Hybrid therapy is essentially divided into two parts: Class 1 is PAP and oral appliance utilized at the same time. Both entities remain independent of one another. Class 2 involves connecting the PAP directly to the oral appliance. The TAP-PAP CS (nasal pillows) is one application of class 2 hybrid therapy and the TAP-PAP CM (custom face mask, CFM) is another application of type 2 hybrid therapy.
One must understand some of the common PAP pitfalls in hopes of assisting the physician in managing the airway. It is usual and customary, during PAP titration studies, patients are placed on full face masks from the beginning of the night to prevent difficulties related to oral pressure leakage, which can occur from the pressure gradient when opening the mouth while on PAP. In other instances, the sleep study starts with a nasal mask but the technologist quickly transitions to a full one when oral pressure leakage occurs. Another clinical scenario may be a patient is titrated with a nasal mask the entire titration, the issue may arise when the patient experiences therapy difficulties at a later date. May we assume the patient simply switch to a full mask under the optimal pressure identified while wearing the nasal mask will also be the optimal pressure on the full mask?
One challenge that requires addressing is during sleep, pressure can leak from the full mask around the mouth or chin as the mandible drops due to relaxation. Patients may tighten the lower straps to improve the seal-but this frequently worsens the airway obstruction by further retruding the mandible. Hybrid PAP-OA therapy offers a unique solution to previously mentioned problem by stabilizing the mandible, therefore offering a stable fitting mask.
Briefly, the oral appliance may serve as a fixed anchorage being it attaches the mask to the skeleton via the mandible and achieves stabilization by way of the maxilla. This allows the elimination of straps and possible reduction of PAP pressure being the mouth does not drop open therefore eliminates the pressure leakage site. The potential TMJ side effects are reduced by not having to advance the lower jaw as much, therefore lessening the strain on the TMJ, tendons, muscles, and facial ligaments. This binary approach of hybrid therapy is unique and potentially offers improved clinical outcomes to the current monophasic approach.
In 2011 El-Solh et al. [1] performed a multipatient study that assessed the efficacy of using an OA in conjunction with an PAP system compared to PAP alone. After 3 days of treatment the combination approach allowed for a significant reduction in the pressure necessary to maintain upper airway patency as well as reduction of residual apnea-hypopnea index (AHI). CPAP pressures were reduced from 9.4±2.3 cm H2O to 7.3±1.4 cm H2O, and residual AHI was reduced from 11.2±3.9 to 3.4±1.5 respiratory events/h of sleep.
In 2016, De Vries et al. [2] evaluated seven patients with moderate to severe OSA who were being treated with CPAP pressures (>10cm H2O) who were then treated with hybrid therapy OA with an integrated set of nasal pillows. After 3 months a polysomnographic study was performed. Four of seven patients reported hybrid therapy to be more comfortable and effective and preferred it over conventional CPAP. There were no differences between baseline (conventional CPAP) and follow-up (hybrid therapy) scores in compliance, satisfaction, daytime sleepiness, and quality of life. Effectiveness of hybrid therapy was good as AHI significantly decreased from median AHI at diagnosis (64.6 events/h; range, 31.0–81.0) to median AHI with hybrid therapy (1.5 events/h). It was concluded that although pressure could be lowered, hybrid therapy was perceived as a comfortable alternative to conventional CPAP.
Long term management of Compromised Neuromuscular Patient with non-invasive ventilation.
Physical Exam
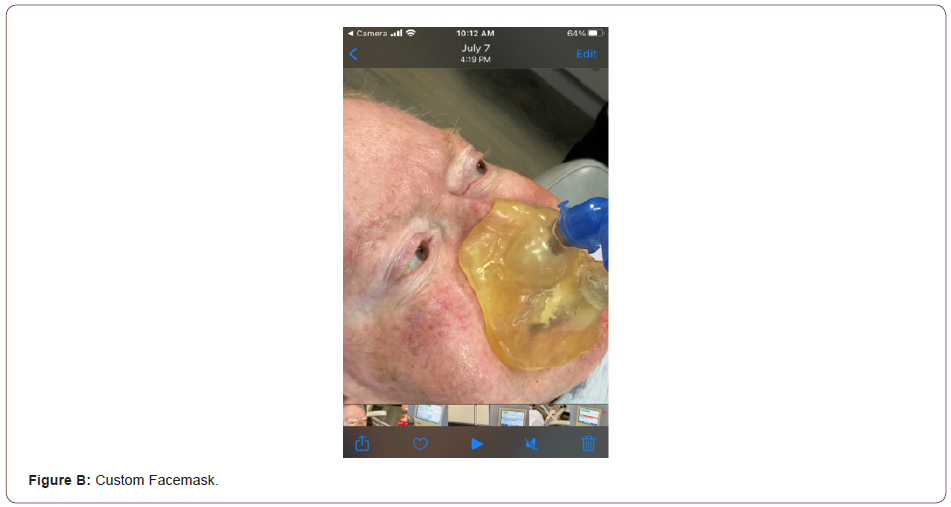
Patient presents to clinic, having utilizing hybrid respiratory therapy nightly for over ten years- undergoes his annual compliance examination. Oral appliance and custom facemask is cleaned and inspected, no evidence of structural compromise, acceptable clinical fit and function. Patient reports, “I would like to get a new one, this is well over ten-years-old...I know that it will give out eventually and don’t really like how it is turning yellow.”
Patient is a 78-year-old male.
Physical examination: General: The patient appears wellnourished,
in no acute distress. Remainder of exam requiring
physical contact not performed as precautionary measure in light
of ongoing Covid 19 pandemic.
Past medical history:
1. History of polio.
2. Hypertension.
3. History of prostate cancer status post radiation therapy in
2008. Prostate cancer has remained in complete remission. The
patient continues to annual follow up with his urologist.
4. Osteoporosis.
Social History: The patient denies any history of alcohol or tobacco use. He is a retired accountant. History of poliomyelitis- Onset: 01/01/1954-He was on an iron lung for approximately 30 years and severe dystrophy in his respiratory muscles and skeletal muscles
Shortness of breath with walking or lying down (polio); Difficulty walking.
Difficulty breathing (polio)
Stiffness or pain in the joints of the fingers, hands, wrists,
elbows, shoulders, neck, back (polio) other neurologic issue: YParalysis
(polio)
Dyspnea-wears home oxygen at home during the night-can use
in the day if needed.
Trilogy positive ventilator- 6. History of poliomyelitis-STABLE
786.12: Personal history of poliomyelitis
Dr. Hughes-saw pt 10/30/2020 some increase in dyspnea
recently however not bad today
R06.00: Dyspnea, unspecified
Neurologic: Gait and Station: irregular gai
t; post-polio
syndrome, has a cane unable to use walker.
Plan: No change to current medications, Continue Ventilator
and oxygen. Return to the clinic in one year.
Oral appliance and custom facemask providing non-invasive
ventilatory care-2010. A. Phillips ventilator. B. Custom Facemask-
Pt was originally fitted in 2010 (Figures A, B).
We hope the above article highlights the need for a change in
treatment paradigm. This is certainly not a new therapy for OSA
but we hope this article raises awareness of the much needed
collaboration between sleep physicians and qualified dentistswhich
is key. As the technology of hybrid therapy improves, so will
the need for further research-all in hopes of expanding the clinical
applications for the custom facemask.
Acknowledgement
There was no external funding for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- El-Solh AA, Moitheennazima B, Akinnusi ME (2011) Combined oral appliance and positive airway pressure therapy for obstructive sleep apnea: a pilot study. Sleep Breath 15: 203-208.
- De Vries GE, Doff MH, Hoekema A, Kerstjens HA, Wijkstra PJ (2016) Continuous positive airway pressure and oral appliance hybrid therapy in obstructive sleep apnea: patient comfort, compliance, and preference: a pilot study. Journal of Dental Sleep Medicine, 3(1): 6.
-
Jeff Paz. The TMJ: Gateway to the Airway. On J Dent & Oral Health. 5(3): 2022. OJDOH.MS.ID.000612. DOI: 10.33552/OJDOH.2022.05.000612.
-
Oral appliance, Mouth, Sleep apnea, Nasal pillows, Hybrid therapy, Daytime sleepiness, Apnea hypopnea index, Facial ligaments, Mask
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






