 Review Article
Review Article
The Role of Orthodontics in Idiopathic Condylar Resorption: A Literature Review
Amna Hasan*, Emory Byrd, V Wallace McCarlie, Jamie Bloss and Iquebal Hasan
East Carolina University, School of Dental Medicine, Department of Surgical Sciences, Department of Pediatric Dentistry and Orthodontics and Dentofacial Orthopedics, North Carolina, USA
Amna Hasan, East Carolina University, School of Dental Medicine, Department of Surgical Sciences, Department of Pediatric Dentistry and Orthodontics and Dentofacial Orthopedics, 1851 MacGregor Downs Road, Mail Stop 701, Greenville, North Carolina 27834-4354, USA.
Received Date: September 27, 2021; Published Date: October 27, 2021
Abstract
Idiopathic Condylar Resorption (ICR) is a pathologic condition affecting the temporomandibular joint that secondarily may present as an anterior open bite, increased overjet, Class II malocclusion, or mandibular retrognathia. Although ICR is a relatively uncommon condition, orofacial pain and orthodontists can recognize its symptoms and presentation. The treatment options can range from nonsurgical to surgical approaches. Although the skeletal and dental malocclusions secondary to the condition are anomalies often treated by orthodontists, the pathological cause of this presentation may require adjustments to typical treatment modalities. Since cases of ICR are rare, there are limited opportunities to conduct randomized clinical trials, making a compilation of case reports relevant data to review to help establish a standardized treatment protocol. Here we review the current ICR treatment trends, focusing on orthodontic management.
Introduction
Idiopathic Condylar Resorption (ICR) is a pathologic condition affecting the temporomandibular joint (TMJ), which results in progressive decreases in the size and morphology of the condyles [1]. The condition is characterized by lysis and repair of TMJ articular fibrocartilage and underlying subchondral bone [2]. The exact cause and pathogenesis of ICR remains unclear, however, it most often presents bilaterally in women between the ages of 15-35 years of age [1]. Some describe the pathogenesis of ICR in terms of abnormal joint loading and pressure resorption following various dental treatments such as occlusal therapy, orthodontics, orthognathic surgery, or third molar extraction; or based on nontreatment factors including internal derangement, parafunction, trauma, and unstable occlusion [1]. However, other predisposing factors may include rheumatoid arthritis, steroid use, systemic lupus erythematous, scleroderma, and other vascular collagen diseases [1, 2].
Patients presenting with symptoms such as an acquired and progressing anterior open bite, progressive overjet or Class II malocclusion, mandibular retrognathia, and a “disappearing chin” are characteristic of ICR [1]. Not knowing the etiological origins of this disease, and therefore not having precise diagnostic tools, ICR can go undiagnosed making treatment difficult [3]. Recommended treatment for ICR varies and can include orthodontics, occlusal splints, prosthetic therapy, orthognathic surgery, TMJ surgery, or a combination of therapies, and are often indicated based on the pathologic activity and conditions of the articular disk and condyle [1]. However, in general, ICR management is controversial among providers [1, 5, 6].
The dental and skeletal malocclusions associated with ICR are malocclusions conventionally treated by orthodontists, with or without collaboration with oral and maxillofacial surgeons. However, the orthodontic approach to treating these malocclusions as they are related to the pathological condition of ICR may require alternative treatment methods in order to preserve the function of the temporomandibular joint and maintain retention after treatment. This literature review aims to present the current research and trends in treatment methods for ICR with a focus on orthodontic management.
Literature Inclusion Criteria
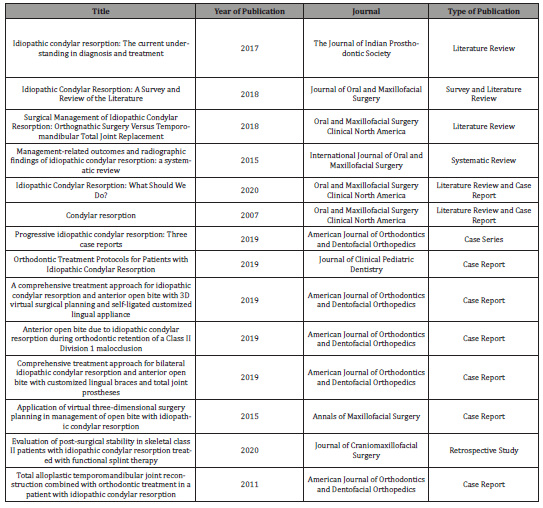
authors conducted a search of MEDLINE via the PubMed database with the following search terms “idiopathic condylar resorption”[tiab] AND orthodont*[tiab]. There were no additional filters applied to the search. The search resulted in 19 articles, and two blinded reviewers assessed the resulting articles separately. Fourteen articles were reviewed based on the inclusion criteria and a discussion from the blinded reviewers. Inclusion criteria included systematic reviews and meta-analyses, randomized clinical trials, cohort studies, case-control studies, case series, and case reports. The search terms and inclusion criteria were based on the goal to present clinical research and trends in orthodontic treatment methods for ICR in order to determine how treatment methods differ based on the pathological cause for malocclusion (Table 1).
Table 1: Literature Search Results.
Discussion
Diagnostic imaging
Early diagnosis of ICR is essential for appropriate management of the condition, and several imaging modalities were reported to be helpful in making a diagnosis. A panoramic radiograph is a common and inexpensive imaging modality and allows for gross evaluation of the condyle [7]. Similarly, a cephalogram radiograph is common in orthodontic treatment and can display shortened posterior facial height, increased anterior facial height, increased overjet, and open bite associated with ICR [7]. Cone-beam computed tomography (CBCT) allows for 3-dimensional evaluation of the condylar features, while magnetic resonance imaging (MRI) is best for evaluating the soft tissues of the TMJ [7]. Nuclear medicine bone scanning with the use of technecium-99 can assess active bony changes, but is not sufficient in assessing the state of stability or remission of bony changes as it relates to active cases of ICR [7]. SICAT jaw motion tracking can also be performed to provide visualization of mandibular movements with predicted condylar position without additional radiation exposure [3]. While panoramic and cephalometric radiographs are commonly taken as diagnostic tools for orthodontic treatment, findings from multiple articles analyzed in this review emphasized the importance of acquiring different images to confirm the presence of ICR, as well as, acquiring images over the course of the disease to determine if resorption is active or inactive [7, 4]. After a diagnosis of ICR, cephalometric radiographs are recommended at 6-month intervals for evaluation of the condylar resorption during the active phase and definitive treatment should only be initiated after the patient has been stable for 6-12 months [2].
Treatment goals and options
In general, the treatment objectives for ICR are to relieve joint pain, establish ideal joint function, correct the anterior openbite malocclusion, and improve facial esthetics [8]. Consistent among several articles reviewed was the emphasis placed on the importance of waiting to begin invasive treatment until after the active resorption had ceased, unless the purpose of treatment is to halt the progression of ICR [4, 9]. Treatments performed to stop active resorption caused by ICR include the initiation of splint use, removal of the hyperplastic synovium, and condylectomy with a costochondral graft [4]. Treatments performed after active resorption has stopped or when a patient is in the inactive phase of ICR include bilateral sagittal-split osteotomy, pre- and post-surgical orthodontic treatment, prosthodontic treatment, alloplastic TMJ reconstruction, and lifetime post-therapy splint use [4]. While each treatment option has unique pros and cons, long-term success of both nonsurgical and surgical treatment approaches to ICR management ultimately rely on the stability and strength of the pathologically affected local TMJ articular and soft tissue elements [6].
Conservative options presented in case reports included an occlusal splint and pain medication with or without conventional orthodontics to camouflage the esthetic changes and correct the class II malocclusion and anterior overbite [8]. Additionally, nonsteroidal anti-inflammatory drugs, therapeutic exercises, intraarticular space steroid injections, and Vitamin D and calcium supplementation to increase bone density during the active resorption stage may be recommended [2, 10]. Other noninvasive treatment options can include exercise, manual therapy, and relaxation training [9]. While nonsurgical, conservative options aim to achieve pain relief and remission of pathological changes first, orthodontic therapy can provide improvements in occlusion but is limited in its ability to drastically improve facial esthetics [8]. Therefore, orthodontists should be aware of the recommendations for surgical management of ICR and the orthodontic management of pre- and post-surgical treatment.
The ideal surgical management of ICR is still controversial, but it has been stated that the most common surgical treatment options include orthognathic surgery alone or combined TMJ and orthognathic surgery. One systematic review found that postoperative stability in cases of ICR treated with orthognathic surgery alone varied from 57-100% while patients treated with total joint reconstruction had 95-100% postoperative stability with follow-up periods ranging from 3 months to 11 years. Although orthognathic surgery alone for the treatment of ICR is a less invasive surgery, it results in a higher rate of relapse and does not allow for correction of mandibular retrognathism, limiting the capacity for esthetic improvement. While TMJ reconstruction using a costochondral graft is a traditional option, costochondral grafts can undergo remodeling and resorption leading to postoperative instability. In comparison, TMJ reconstruction with a prosthetic total joint replacement can provide improved stability, esthetics, and jaw function without the risk of remodeling or ankylosis. Moreover, an alloplastic prosthesis has been presented as the first choice in surgical treatment because it has increased longevity, increased stability after counterclockwise rotation of the maxillomandibular complex, and eliminates the need for a second surgical site. Counterclockwise rotation of the maxillomandibular complex can lead to improved esthetic outcomes by restoring posterior facial height and increasing mandibular advancement at the B point and pogonion. Thus, reviews suggest that an alloplastic joint replacement combined with orthognathic surgery may be the preferred surgical approach for most patients.
Case reports of conservative treatment approaches
An example of a conservative treatment therapy presented in one case report discussed a patient who presented to an orthodontist with ICR symptoms, including development of an anterior open bite and jaw pain, 10 months following initial orthodontic treatment [9]. In this case, the patient was treated using soft then hard splints and eventually a flat plane stabilization appliance was delivered for the maxillary arch to be worn at night [9]. Subsequently, a mandibular orthopedic repositioning appliance was delivered for daytime use only in order to produce vertical dimensional and horizontal maxillomandibular changes to allow the TMJ to heal and resorption to conclude prior to corrective ICR treatment [9]. This case report displayed splint therapy as a first line treatment of ICR to unload the condyles, prevent progression of the disease, and relieve discomfort and muscle hyperactivity [9]. It also stated that occlusal splints can be used as diagnostic tools to evaluate for cessation of the resorptive process by assessing whether the mandibular incisors are still in contact with the splint or if an open bite has progressed [9].
Another case report details conservative treatment using an orthodontic-only treatment approach [10]. In this case, the patient had four premolars, the maxillary first premolars and mandibular second premolars, extracted to resolve the large overjet and maxillary posterior teeth intruded to achieve a counter-clockwise rotation of the mandible [10]. A double transpalatal arch and temporary skeletal anchorage devices (TSADs) were used to resolve the anterior open bite [10]. Two temporary skeletal anchorage devices were placed in the buccal alveolar bone between the roots of the maxillary first and second molars and four were placed in the palatal bone between the first premolars and molars bilaterally [10]. After four months of intrusive forces on the buccal and palatal sides to close the open bite, the patient started full fixed treatment and 0.022 inch preadjusted edgewise orthodontic appliances were bonded [10]. Maxillary extraction spaces were closed with elastomeric chains from the posterior buccal mini-screws to hooks between the lateral incisors and canines.10 The class II molar relationship was corrected using TSADs between the canines and first premolars in the mandibular arch, which were placed on both sides for anchorage. Inter-arch elastics were avoided since change of the condylar position could be harmful for patients with ICR [10]. The orthodontic treatment was completed after 30 months of treatment and class I canine and molar relationships were achieved with ideal overjet and overbite [10]. The treatment produced considerable improvement in the patient’s facial esthetics but did not correct the convex profile due to the retrognathic mandible [10]. The results were stable at 2-year retention [10]. Therefore, this case exemplifies the effectiveness of an orthodontic-only treatment approach to achieve joint pain relief, ideal joint function, and correction of the anterior open-bite malocclusion, while also depicting the limitations in improving overall facial esthetics.
Case report of combined orthodontic and orthognathic surgery treatment
In a case report describing combined orthodontic and orthognathic surgery management, 3-D medical modeling with the surgeon was used to give the clinician and patient a more realistic expectation of soft and hard tissue changes after surgery [11]. In this case report, a 22-year-old Caucasian female with ICR presented for treatment [11]. The comprehensive orthodontic-orthognathic surgery treatment plan selected aimed to correct the anteroposterior, transverse, and vertical discrepancies of the maxilla and mandible, improve esthetics, and reduce TMJ discomfort [11]. Presurgical orthodontic treatment was initiated with ceramic 0.022 MBT prescription brackets and segmented alignment was carried out in three sections with bends to distalize canine roots and mesialize lateral incisor roots [11]. Before the orthognathic procedure, 0.019x0.025 stainless steel wires with surgical hooks were placed [11]. The surgery included a 3-piece Le Fort I osteotomy to intrude molars and increase intermolar width [11]. The mandible was surgically advanced with an inverted L-osteotomy and auto-rotated to close the bite [11]. A genioplasty was also performed to improve facial esthetics [11]. Following surgery, postoperative orthodontic treatment was initiated five weeks after surgery and post-operative splint use and settling was completed through Class II box elastics [11]. Although the report detailed improved esthetics, significant anterior-posterior changes in the mandible, reduced lower third height, and increased ramus length, it was stated that the patient may have benefitted from more maxillary incisor buccal torque and some interproximal enamel reduction [11]. The results were stable at one year following surgery [11]. Overall, this case provides an example of a successful combined orthodontic and orthognathic surgery treatment approach.
Case reports of total temporomandibular joint replacement
The most aggressive treatment approach includes temporomandibular total joint replacement. Arguments in favor of total joint replacement as the first-line surgical therapy for patients with ICR include the elimination of postsurgical remodeling of chostochondral tissue which favors stability and longevity of the prosthesis material. Because TMJ alloplastic prostheses lack growth potential, they do not have the risk of unpredictable growth patterns associated with costochondral grafts, but they also cannot be used on ICR patients until they have reach skeletal maturity.
One case report depicts a more aggressive treatment approach which included pre-surgical orthodontic alignment and leveling of both arches, jaw motion tracking (JMT) to detect mandibular movement, Le Fort 1 3-piece maxillary osteotomies with mandibular reconstruction, bilateral coronoidectomy with condylar replacement with TMJ concept custom fossa, and postsurgical orthodontic correction of the malocclusion [3]. The treatment goals included eliminating mandibular crowding, correcting the open bite, decreasing the high mandibular plane angle, reducing ANB, eradicating TMJ resorption, reconstruction of the condyles, correction of the gummy smile, and improvement of the facial profile [3]. The presurgical orthodontic treatment was performed with the use of custom lingual braces and clear brackets for esthetic purposes [3]. Leveling started with 0.014inch NiTi wires, followed by 0.016x0.022inch, and eventually 0.012x0.025inch wires were used to maintain the open bite to facilitate the surgical procedure [3]. The maxillary teeth were leveled segmentally and the maxillary arch wire was cut between the lateral incisors and canines to facilitate the osteotomies and prevent relapse of the open bite after surgery [3]. A continuous arch wire at the beginning of the postsurgical period aided in better control for final occlusal adjustments [3]. Clear brackets were placed on the facial axis point at the labial and buccal surfaces of both arches to aid in attachment of the occlusal splint and inter-arch elastic band setting [3]. Five months after presurgical orthodontic treatment was initiated, the orthognathic surgery was planned with an oral surgeon with the use of virtual surgical planning, and thirteen months after the initiation of orthodontic treatment, the orthognathic surgery was completed [3]. Final occlusal adjustments were made with 0.014 NiTi wires and setting was performed using elastic bands. The posttreatment records for the patient in this case report display correction of the anterior open bite, normal overjet and overbite, proper leveling and alignment, and acceptable facial esthetics [3]. This case report displays the use of clear custom lingual brackets as an example of esthetic modifications to traditional orthodontics within a complex treatment plan while using advanced technology to create more accurate treatment outcomes.
In a similar case report, a 14-year-old female with ICR presented for orthodontic treatment of ICR [5]. The final treatment plan included maxillary and mandibular arch fixed appliance presurgical orthodontic treatment, Le Fort I maxillary osteotomy to advance the maxilla, bilateral condylectomy and mandibular joint replacement with TMJ implants, and postsurgical orthodontic treatment [5]. The presurgical orthodontic treatment was initiated using customized self-ligating lingual appliances with 0.014inch NiTi wires followed by 0.016x0.022inch NiTi wires [5]. The dental open bite was maintained during mandibular leveling and alignment to facilitate the surgery [5]. Twelve months into presurgical orthodontic treatment, virtual surgical planning allowed for planning of the orthognathic surgery with an oral surgeon [5]. In addition to the use of state-of-the-art technology used in virtual model surgery, medical modeling can be used in stereolithic guide fabrication to be used by the surgeon for a more predictable custom-fitted total joint prostheses [5]. The orthognathic surgery was performed twenty months after initiation of presurgical orthodontic treatment [5]. Orthodontic brackets were placed on the facial axis point on the labial and buccal surfaces of the upper and lower arch to aid in fixation of the occlusal splint and inter arch rubber band setting [5]. Five weeks following surgery, the splint was removed and maxillary and mandibular arch alignment and occlusal adjustments were made using 0.014 inch NiTi wires and setting was completed with elastic bands [5]. The outcome achieved functional and esthetic treatment objectives and the retrognathic mandible and anterior open bite were successfully corrected [5].
Another similar case report depicts a treatment approach which combined total joint replacement with mandibular advancement and genioplasty orthognathic surgery with orthodontics [8]. In that case, 0.022 inch preadjusted edgewise brackets were bonded to all teeth and a precision transpalatal arch with a 0.032x0.032- inch beta-titanium alloy wire was placed for correction of the upper first molar rotation and mild arch expansion [8]. A compensating curve was added to the arch wire in the initial stages of treatment to improve maxillary incisor torque and mandibular first premolars were extracted to allow for the maximum amount of mandibular advcancement [8]. In order to make the most esthetic improvements, counterclockwise rotation with ANS impactions, canting correction of the maxilla, and advancement genioplasty were planned along with the mandibular advancement [8]. After 14 months of preorthodontic treatment, surgical treatment, including Le Fort 1 osteotomy, geneioplasty, and total joint reconstruction, was completed. The occlusion was corrected to Angle Class I molar and canine relationships with ideal overjet and overbite [8]. Following the primary healing period after surgery, physical therapy was recommended 3 weeks postoperatively and postsurgical orthodontics was implemented. Intermaxillary elastics were using for final detailing and the brackets were debonded after a total treatment time of 24 months. The case report stated that the patient remained stable at 1 year of retention [8]. These cases outlined successful treatment of ICR cases which resulted in elimination of TMJ pathology and provided an improved esthetic and functional outcome while emphasizing the importance of combined surgical and orthodontic treatment for ideal ICR management [3].
Presurgical splint therapy use
It has been suggested that splints may alleviate TMJ loading, preventing acceleration of ICR [4]. Hard acrylic splints have been recommended instead of vacuform materials in order to have a thick enough material to fill the open bite and bring all teeth into occlusion [4]. In a retrospective study performed, it was suggested that postsurgical mandibular relapse is most likely to be caused by an unstable condylar position in the glenoid fossa, which poses challenges for clinicians determining the amount of mandibular advancement [12]. By deprogramming the masticatory muscles using pre-surgery splint therapy, clinicians were able to develop a more accurate surgical [12]. In a clinical trial evaluating 16 female patients treated with functional splint therapy prior to combined orthognathic and orthodontic treatment, 13 presented with a stable mandibular position with less than 2mm of mandibular change while 3 patients presented with a mandibular relapse [12]. Although the sample size is small, this study suggests that functional splint therapy prior to orthognathic surgery for mandibular advancement may be a good adjunctive treatment for ICR patients in order to improve postsurgical skeletal stability [12]. Since presurgical orthodontic therapy may also be initiated in the year prior to orthognathic surgery for ICR, implementation of presurgical functional splint therapy may coincide with the orthodontic treatment. Similarly, post-therapy occlusal splint is recommended for lifetime use and may need to be fabricated by an orthodontist once a patient enters the retention phase.
Orthodontic treatment without icr diagnosis
While development of ICR during orthodontic treatment is rare, pain and longer orthodontic treatment times may be the only signs of the condition and ICR may remain undetected and undiagnosed until a patient develops an anterior open bite after orthodontic treatment is completed [4]. Therefore, if it is suspected that a patient may have developed ICR during orthodontic treatment, then mid-treatment imaging should be performed [4]. One case series depicted cases where patients received orthodontic treatment without a diagnosis of ICR at the onset of treatment [7].
One such case reviewed outlines a 19 year old female presenting for an orthodontic consultation with complaints of “crooked teeth” and TMJ pain [7]. The patient reported TMJ pain problems beginning at age 16 and a multitude of therapies were conducted including occlusal appliance therapy, physiotherapy, muscle relaxants, NSAID use, disc injections, bilateral TMJ arthrocentesis, 200 U Botox injections, and Decadron injections [7]. Imaging displayed a flattened anterosuperior surface of the left condyle with Class III subdivision left dental relationship and a right deviation of the lower midline [7]. Her initial treatment included extraction of the 4 first premolars and a functional genioplasty to obtain lip competency and normal anterior facial height [7]. Bilateral disc repositioning was performed 18 months into orthodontic treatment and TMJ pain increased throughout treatment [7]. A CBCT taken displayed a decrease in articular disc space , significant right condyle resorption, reduced interarticular space, flattening of the articular eminence, and progressive flattening of the anterosuperior surface of the left condyle [7]. The orthodontic treatment was complete at 40 months, but the patient developed an anterior open bite four months after debonding [7]. Ultimately, total joint replacement was deems the only treatment option and a bilateral alloplastic total joint replacement was performed using Zimmer Biomet functional prostheses [7]. Follow-up records for this case displayed establishment of functional occlusion and improved facial esthetics with a lack of lateral movement of the jaw [7]. While development of ICR during orthodontic treatment is rare, this case exemplifies how ICR may present during active orthodontic treatment. Orthodontists are in a position to recognize and diagnose the condition and may need to stop active treatment or alter the existing treatment plan in order to address the pathology leading to occlusal and skeletal changes.
A similar case reports a female patient who presented for orthodontic treatment with a Class II Division I malocclusion and anterior open bite [7]. The patient had been followed by her dentist for TMJ pain for the past 7 years and had undergone orthodontic treatment 12 years earlier [7]. In the time between her debonding appointment seven years prior and her consultation, the patient had developed significant TMJ pain and sleep apnea symptoms [7]. The patient had been made 3 occlusal splints over the course of the 7 years and multiple imaging modalities taken over time displayed severe bilateral condylar resorption, decreased posterior facial height, short mandibular ramus, high mandibular plane angle, anterior open bite, a retrognathic mandible, and reduced airway shadow [7]. The best management option was deemed to be bilateral alloplastic total joint replacement with Zimmer Biomet custom prostheses [7]. Fifteen days following surgery, the patient displayed Class I functional occlusion, improved profile esthetics, increased airway profile, and normal overbite and overjet [7]. The patient was prescribed physiotherapy and no additional orthodontic therapy [7]. Even though this patient did not have ICR symptoms at the time of original orthodontic treatment, the signs and symptoms of the condition that developed in the years after treatment characterize ICR. Because of the skeletal and dental changes that occur as a result of ICR, orthodontists have an important role in recognizing the clinical presentation of the condition and recommending treatment which addresses the pathological cause of these facial changes.
Conclusion
It has been reported that orthodontists see an incidence of ICR in roughly 1 in 5000 patients while orthognathic surgeons report an incidence of 2-5% of patients [9, 10]. Due to the rarity of the condition, published research conducted on ICR is limited and no standard treatment protocol exists. Overarching themes from the sources reviewed confirmed the need for further investigation on diagnostic tools and treatment planning, comparing outcomes between surgical, nonsurgical, and pharmacological management of ICR, and randomized clinical trials with longer follow-up periods [13]. In a systematic review of the management-related outcomes and radiographic findings of idiopathic condylar resorption published in 2015, the 17 studies that met the eligibility criteria were all case reports, indicating a large need for future research, including randomized clinical trials, on the subject [13]. Furthermore, there is a lack of consistency in the preferred methods of treatment of ICR demonstrating a need for a more structured universal treatment approach [13]. Although ICR is a relatively uncommon condition, orthodontists must be able to recognize the symptoms and presentation and be prepared to diagnose ICR and develop treatment plans in conjunction with oral and maxillofacial surgeons and other dental specialists in order to best meet the needs of the patients.
References
- Papadaki ME, Tayebaty F, Kaban LB, Troulis MJ (2007) Condylar resorption. Oral Maxillofac Surg Clin North Am 19(2): 223-vii.
- Mercuri LG, Handelman CS (2020) Idiopathic Condylar Resorption: What Should We Do? Oral Maxillofac Surg Clin North Am 32(1): 105-116.
- Rahman F, Celebi AA, Louis PJ, Kau CH (2019) A comprehensive treatment approach for idiopathic condylar resorption and anterior open bite with 3D virtual surgical planning and self-ligated customized lingual appliance. Am J Orthod Dentofacial Orthop 155(4): 560-571.
- Young A (2017) Idiopathic condylar resorption: The current understanding in diagnosis and treatment. J Indian Prosthodont Soc 17(2): 128-135.
- Wang J, Veiszenbacher E, Waite PD, Kau CH (2019) Comprehensive treatment approach for bilateral idiopathic condylar resorption and anterior open bite with customized lingual braces and total joint prostheses. Am J Orthod Dentofacial Orthop 156(1): 125-136.
- Alsabban L, Amarista FJ, Mercuri LG, Perez D (2018) Idiopathic Condylar Resorption: A Survey and Review of the Literature. J Oral Maxillofac Surg 76(11): 2316.e1-2316.e13.
- Chamberland S (2019) Progressive idiopathic condylar resorption: Three case reports. Am J Orthod Dentofacial Orthop 156(4): 531-544.
- Chung CJ, Choi YJ, Kim IS, Huh JK, Kim HG, Kim KH (2011) Total alloplastic temporomandibular joint reconstruction combined with orthodontic treatment in a patient with idiopathic condylar resorption. Am J Orthod Dentofacial Orthop 140(3): 404-417.
- Park JH, Park JJ, Papademetriou M, Suri S (2019) Anterior open bite due to idiopathic condylar resorption during orthodontic retention of a Class II Division 1 malocclusion. Am J Orthod Dentofacial Orthop 156(4): 555-565.
- Lee GH, Park JH, Lee SM, Moon DN (2019) Orthodontic Treatment Protocols for Patients with Idiopathic Condylar Resorption. J Clin Pediatr Dent 43(4): 292-303.
- Kau CH, Bejemir MP (2015) Application of virtual three-dimensional surgery planning in management of open bite with idiopathic condylar resorption. Ann Maxillofac Surg 5(2): 249-254.
- Ha N, Hong Y, Qu L (2020) Evaluation of post-surgical stability in skeletal class II patients with idiopathic condylar resorption treated with functional splint therapy. J Craniomaxillofac Surg 48(3): 203-210.
- Sansare K, Raghav M, Mallya SM, Karjodkar F (2015) Management-related outcomes and radiographic findings of idiopathic condylar resorption: a systematic review. Int J Oral Maxillofac Surg 44(2): 209-216.
-
Amna Hasan, Emory Byrd, V Wallace McCarlie, Jamie Bloss, Iquebal Hasan. The Role of Orthodontics in Idiopathic Condylar Resorption: A Literature Review. On J Dent & Oral Health. 5(1): 2021. OJDOH.MS.ID.000605.
-
Idiopathic Condylar Resorption, Orthodontic management, Orthodontics, Oral and maxillofacial surgeons, Orthodontic treatment, Facial esthetics, Prosthodontic treatment, Reconstruction, TMJ surgery.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






