 Research Article
Research Article
Single Tooth Implant Case in A Contraindicated Patient
Nilesh R Parmar*
BDS MSc (ImpDent), MSc (ProsthDent) Cert Ortho, Principal of Parmar Dental, UK
Nilesh R Parmar, BDS MSc (ImpDent), MSc (ProsthDent) Cert Ortho, Principal of Parmar Dental, UK.
Received Date: July 20, 2022; Published Date: September 21, 2022
Introduction
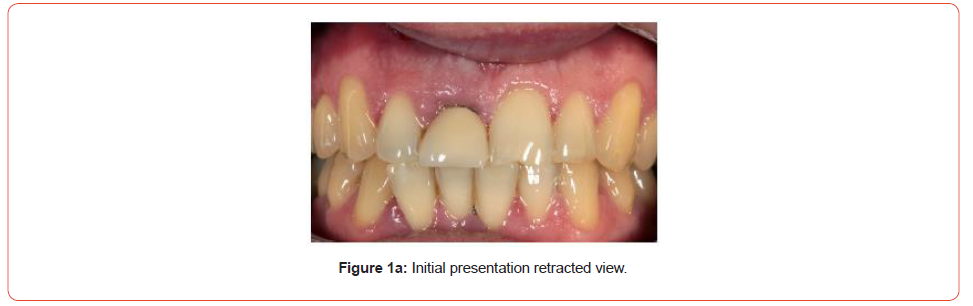
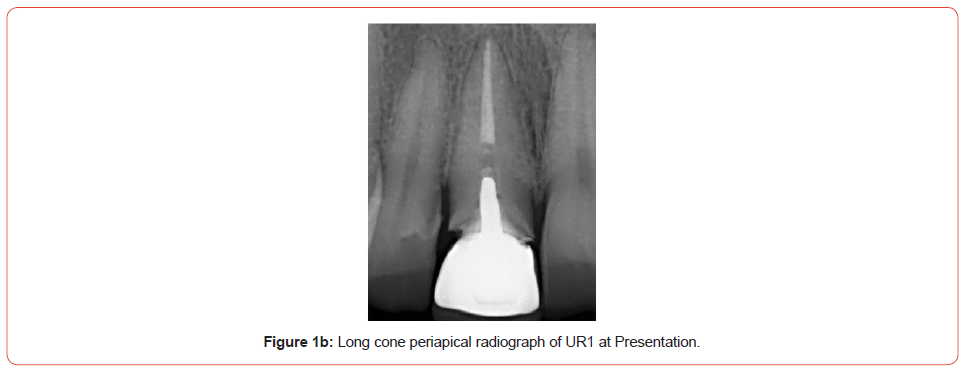
A male patient was referred to me regarding his UR1. The tooth had been root treated and post crowned after the patient suffered trauma over 10 years ago. Since it was done, the post crown would de-bond every few years, and the patient’s dentist would re-cement it. At his last visit, where the crown had come out, the patient’s dentist told him that the root had now appeared to have a fracture line and has a limited long-term lifespan (Figures 1a, 1b). The patient was then referred to me.
For implant cases such as these, I have a 30-minute consultation appointment where we assess and take radiographs and photographs before moving into my consultation area to discuss the patient’s options.
In this patient’s case, he was unhappy about having a loose front tooth. It was stopping him from confidently eating and affecting his social interactions. He also thought it might be affecting his work interactions, as he has had to go to work on occasions without the crown in.
Medically, the patient was fit and well, but has a family history of osteoporosis. He has been taking oral bisphosphonates (OBs) for over five years, which required a lengthy discussion regarding the risks of complications associated with these medications.
Treatment options
As with any situation there are always various options as to how we can proceed. I did consider removing the post crown to assess the root fracture, however a phone call to the referring dentist provided me with the information needed. Her opinion was that restoring the tooth with another post crown would have a very poor prognosis. This is due to a fracture running bucco/lingually down the root.
I try and keep a very open line of communication with my referring dentists. Some love to be kept informed of what is going on, some don’t want to be bothered. This dentist always takes a very keen interest in her patient’s treatment and usually will come to the implant placements if she has the time. If her opinion was that the tooth was unrestorable, then I would accept that and offer alternative options. In this case, the patient had the options of a denture, a conventional bridge, a resin bonded bridge or an implant:
• Partial denture-the patient wasn’t keen on a partial denture long term. He had no issue wearing one whilst the site was being developed but was not interested in having one as a permanent option.
• Conventional bridge-this was disregarded, as preparing the adjacent teeth would have meant removing enamel and would be far too invasive.
• Resin-bonded bridge-we discussed this for a lengthy time; with the risks of osteoradionecrosis of the jaw
(ORNJ) making implants a slightly risky option, a resin-bonded bridge was an attractive solution. It was cheaper and quicker as a bonus. However, what concerned the patient was the likelihood of the bridge debonding. With evidence of parafunction and guidance on the UL1 it was a likelihood. The patient was not keen on swapping a debonding crown with a debonding bridge.
• Implant-out of all the options, this was the most ambitious. Not only did the patient have a medical issue with the bisphosphonates, he had a relatively high smile line, and a pink envelope of gum that was not ideal.
Implants and oral bisphosphonates
OBs potentially have a rare side effect known as MRONJ (medication-related osteoradionecrosis of the jaw). In essence, following on from a tooth extraction the bone does not heal. Instead, exposed bone is left with little or no blood clot. This can be very painful for the patient and difficult to manage. The exact mechanism, and cause of this is not yet fully understood.
Currently in the UK there are two major publications that implant surgeons are following. One is a paper published by the ADI (Suzuki and Lee, 2012) [1], and the other is the Scottish Dental Clinic Effectiveness Programme guidelines published recently (SDCEP, 2017) [2]. The incidence of MRONJ in non-cancer patients is estimated at 0.01-0.1% (SDCEP, 2017).
I have treated several patients on OBs and to this date not had any complications. I have however declined one patient who has had IV bisphosphonate medication for cancer. In the current case, I spent time going through the research and giving the patient copies of the ADI and the SCDEP guidelines. Helpfully, both these publications have addendums that are written for patients to read.
As the patient had already had extractions without complications whilst taking OBs, he was happy to accept the risk and proceed with implant placement. We also decided to use PRGF as the carrier method for bone regeneration, as recent research shows this has a positive effect on reducing the risk of MRONJ (Pelaz et al, 2014) [3]. The patient attended with an unsatisfactory cosmetic appearance in his opinion. The UR1 has a poor emergence compared to the UL1 resulting in asymmetry. There is darkening at the margin due to the underlying metal core along with some passive eruption of the UR1.
Treatment planning
Once we had decided on an implant solution, there were some options available as to how best to proceed.
Conventional implant modality would be removal of the tooth, allow three to four months to heal, then implant placement with guided bone regeneration (GBR).
However, in this case, due to the abundant palatal bone and excess labial tissue, I was keen on an immediate implant solution. This would allow me to maintain the soft tissue utilising the gingiva and push it back with a screw retained temporary crown if needed. The diagnostic phase involved impressions, a collimated CBCT, fabrication of a labial stent, surgical planning and immediate denture fabrication (Figures 2-4).
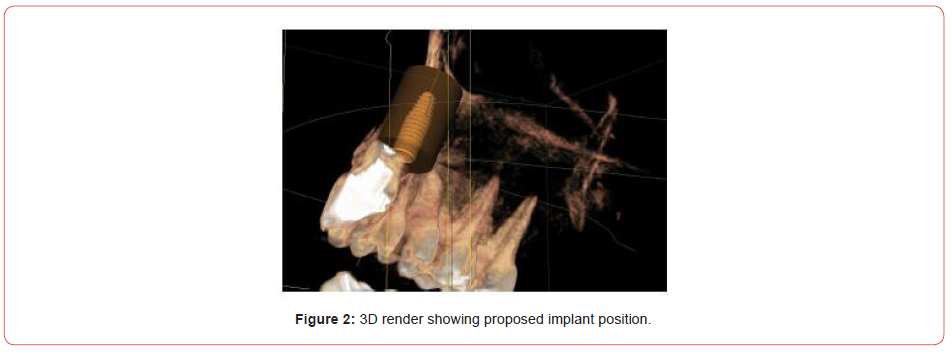
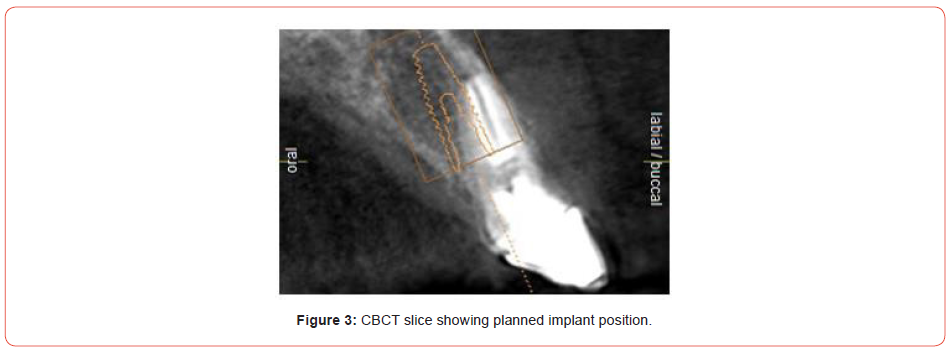
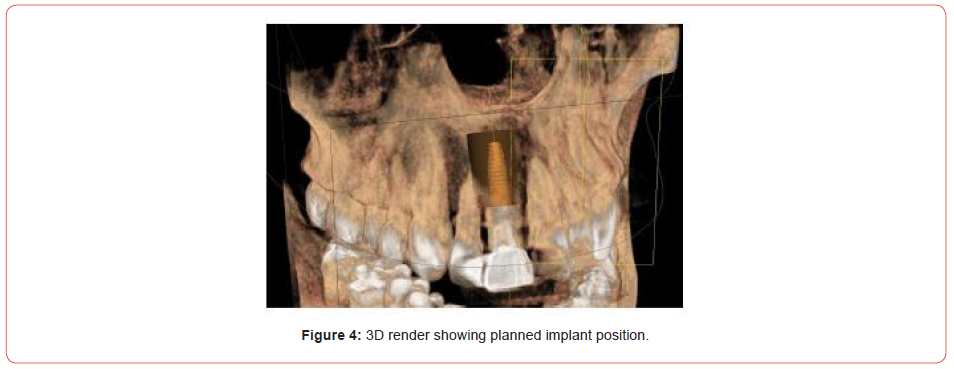
Consent is especially important in implant cases; once the exact treatment is decided upon, patients are brought in for a step-by-step outline of how the work will be completed. This is then presented in a treatment plan that the patient signs. It became apparent, that due to the proclination of the UR1, and the bulk of available palatal bone, that a screw retained final restoration would be possible.
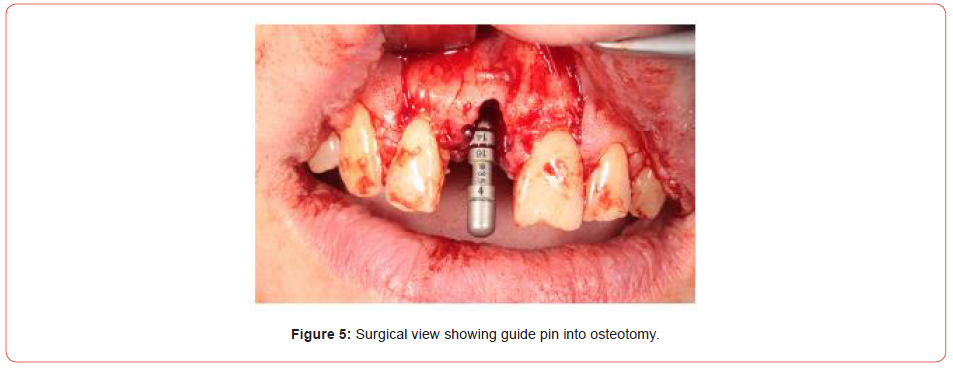
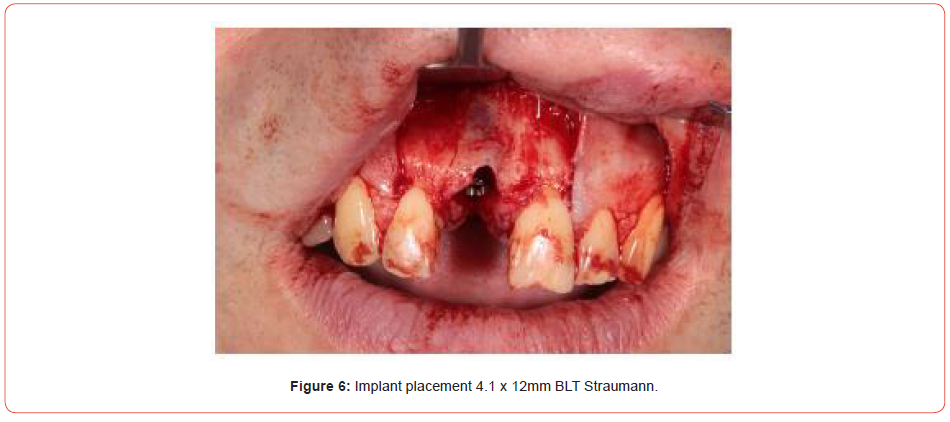
Implant placement
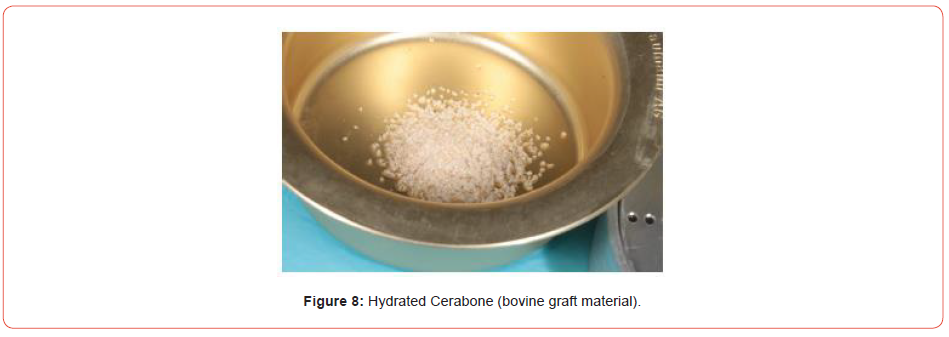
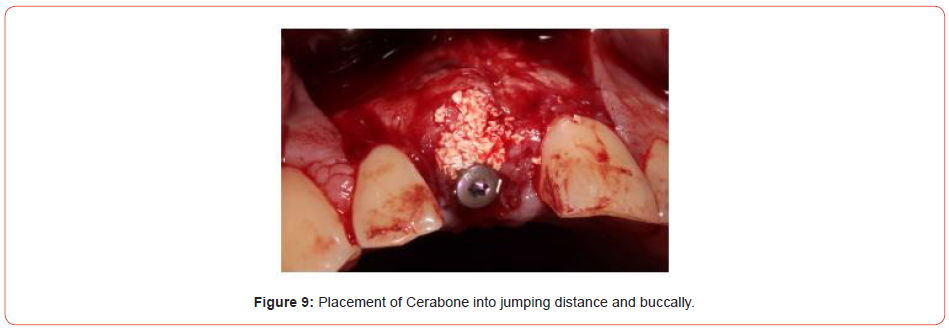
Extraction of the UR1 was conducted, with immediate implant placement with simultaneous bone grafting using a bovine graft material (Figures 5-9). This was then covered using a plasma membrane using PRGF (plasma rich in growth factors) (Figure 10).
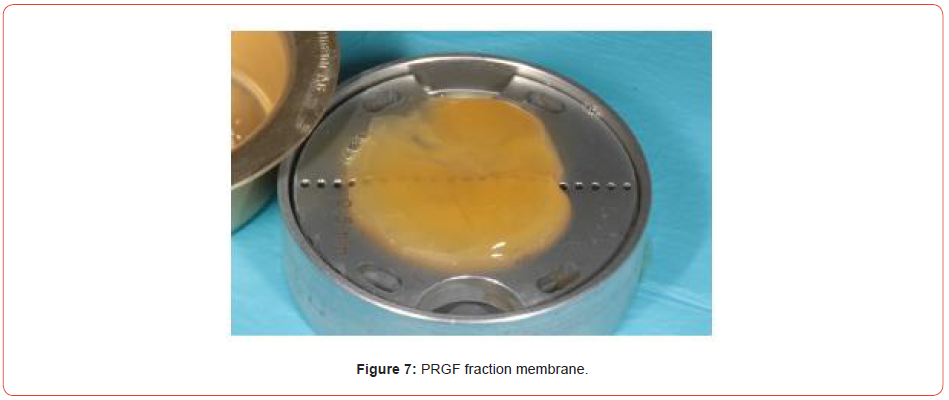
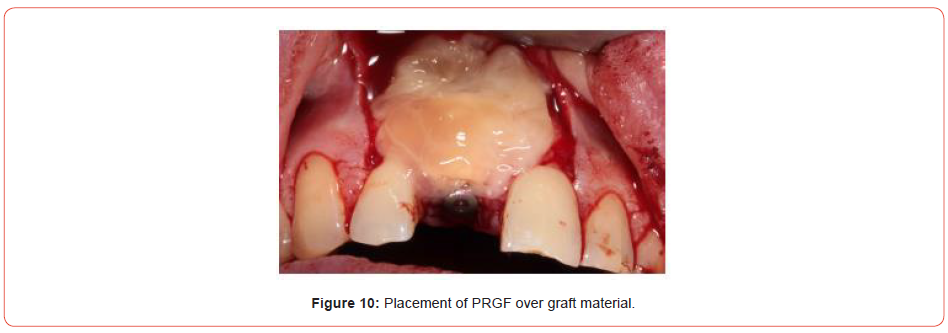
This is made by taking four vials of blood from the patient prior to implant placement, spinning the blood up in a centrifuge for eight minutes and then removing the necessary fractions. Addition of calcium chloride and placement in an oven allows the fractions to set and can be easily handled in the oral cavity.
The Straumann 4.1 BLT x 12mm implant achieved adequate stability and the site was fully closed. A cover screw was placed over the implant and was allowed to heal for three months. The site healed uneventfully and was exposed with a mid-crestal incision.
Due to the patient’s medication, he was reviewed on a weekly basis for the first month. This was to assess for symptoms to MRONJ. Due to his work commitments, the patient was seen at the end of the clinical sessions, so he could attend the clinic without having to take time off work. Thankfully, he healed without incident (Figure 11).

Implant restoration
A fixture level Impregum impression was taken and sent to my lab technician, Richard Green of Implant Design Solutions. In this case, the patient went to see Richard for a shade match, along with the photographs taken by myself and a shade overlay made using the Vita Easy Shade.
A screw-retained temporary crown was initially part of the patient’s treatment plan, but due to financial restraints this part of the treatment was not executed. Instead, we moved directly to the final screw retained restoration.
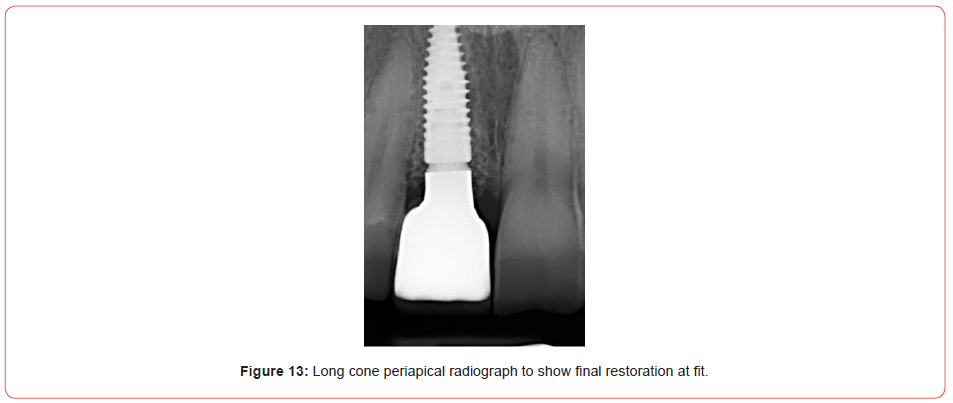
The restoration chosen was a screw-retained solution. This allowed for easy retrievability of the implant restoration should there be any issues in the future. It also cancels the need for cement and the risk of cement induced peri-implantitis. The implant crown was screwed directly into the fixture and a torque of 35Ncm obtained. A sterile PTFE plug and A1 composite was used to block out the access cavity (Figures 12, 13).

Maintenance phase
All implant patients are seen by my in-house hygiene team to show patients how to clean around their dental implants. We also encourage them to take ownership of their work, and understand that implants are not forever and need regular assessment and maintenance.
As visible from the photographs, the patient does exhibit some parafunction. Therefore, a nocturnal splint was manufactured at the end of treatment and the UR1 implant crown made clear of heavy protrusive movements.
Prognosis
The patient has now been restored for six months. In that time, he has attended all his appointments and is diligent with his maintenance and aftercare.
He has also been wearing his splint and I feel that he has a very good long-term outlook for his implant restoration.
Acknowledgement
None.
Conflict of interest
No Conflict of Interest.
References
- Suzuki J, Lee C (2012) ADI 2012 white paper on antiresprptive therapy and osteonecrosis of the jaws (ARONJ).
- Scottish Dental Clinical Effectiveness Programme (2017) Oral health management of patients at risk of medicationrelated osteonecrosis of the jaw-dental clinical guidance.
- Pelaz A, Junquera L, Gallego L, García Consuegra L, Junquera S, et al. (2014) Alternative treatments for oral bisphosphonate-related osteonecrosis of the jaws: a pilot study comparing fibrin rich in growth factors and teriparatide. Med Oral Patol Oral Cir Buccal 19(4): e320-e326.
-
Nilesh R Parmar*. Single Tooth Implant Case in A Contraindicated Patient. On J Dent & Oral Health. 6(2): 2022. OJDOH.MS.ID.000634. DOI: 10.33552/OJDOH.2022.06.000634.
-
Tooth, Dentist, Partial denture, Oral cavity, Implant restoration, Periodontitis, Peri-implantitis, Single tooth, Front tooth, Oral bisphosphonates
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






