 Editorial
Editorial
Perio Protect Method to Deliver Timed-Release Hydrogen Peroxide to the Salivary Ducts and the Oral Environment for Possible SARS-CoV-2 Protection
Duane C Keller*
Department of Dentist, Keller Professional Group PC, Perio Protect LLC, Bayless Avenue, St. Louis, MO, USA
Duane C Keller, Department of Dentist, Keller Professional Group PC, Perio Protect LLC, Bayless Avenue, St. Louis, MO, USA.
Received Date: April 21, 2020; Published Date: April 29, 2020
Abstract
The world is experiencing the ninth Severe Acute Respiratory Syndrome (SARS)-Coronavirus infection; the pandemic of 2020 cause by the SARSCoV- 2 (SARS-CoV-19) virus. The dental profession, the country and the world are unprepared for this event. This tragedy provides an opportunity to learn the steps that occur between cause and effects. A method is presented here for professional review that demonstrates a way patients may be helped in protecting themselves from these events through delivering and maintaining a 1/7% concentration of hydrogen peroxide (Perio Gel™) in the oral environment at the salivary duct openings using a custom formed FDA cleared medical device (Perio Tray™) [Perio Protect LLC, St Louis, Mo]
Disclaimer: This editorial is a concept for professional review and use if warranted. There are no clinical studies to demonstrate efficacy of SARS-CoV-2 management with the Peril Protect Method™.
Introduction
Some authors state we are lucky that we are experiencing the present SARS event rather than previous infections. Ceccarelli [1] explain that the present SARS-CoV-2 mortality rate is approximately 2.3%, but if this had been the SARS-CoV-MERS (Middle East Respiratory Syndrome) the mortality rate was 9.8%. The CDC report explains the mortality of SARS-CoV-19 is approximately 0.2% in young healthy individuals, but it increases with age and is highest in adults over 80 with other pre-existing conditions. The World Health Organization and Arabi Y [2] explain the mortality rate of the current pandemic for older individuals is about 10%, while the SARS-CoV-2(MERS) had a mortality rate for older individuals approximating 35%.
The coronavirus is spread by two commons means: person to person contact through airborne respiratory droplets and from a hard surface followed by fomite transmission to the host. Anfinrud P [3] explain that speaking produces significantly more droplets than coughing. They further explain why all health providers should therefore wear masks and personal protective equipment (PPE).
There are many reports of how the SARS-CoV-2 enters cells and some suggestions are offered to block entry. Much of the information currently discussed is about the earlier SARS-CoV strains because there is not as much information about the SARS-CoV-2. Hoffman [4] discuss the attachment of the SARS-CoV “spike” protein to the cell angiotensin converting enzyme 2 (ACE-2) and other entities and how the virus replicates within the host cell(s) to be released for further infection. They explain how a protease inhibitor blocks the attachment/entry. Kai Wang [5] discuss how the 2019-n-CoV is found in almost all saliva specimens of infected patients. This may be explained by Liu L [6] in their article evaluating the prior SARS-CoV strain in Rhesus Macaques. They discuss how the SARSCoV targets the cells of the upper respiratory tract specifically the “target” epithelial cells lining the salivary ducts.
Liu [6] place “tagged” virus via the internasal route and analyse all of the cells of the respiratory tract. They repeat their study three times with similar findings. The virus is first found in the epithelial cells of the salivary ducts and this is confirmed by a second RNA probe test. The virus invades the basal layer of the epidermis and the epidermis basement membrane within 48 hours of epithelial assault. They did not find other respiratory tissues infected by the virus labelled cells and there are no positive findings in any of the control animals at 48 hours. The Salivary duct “target” cells provide a possible means of protection from the virus [7-10]. The American Dental Association recommends patients rinse with 1% hydrogen peroxide before their dental visit as 0.5% hydrogen peroxide kills the coronavirus in 1 minute. Oral rinsing is beneficial, but some problems occur. Liquid hydrogen peroxide has a “burst” effect, meaning it loses its potency within 1-2 minutes. This time constraint is problematic with other recommendations.
The Environmental Protection Agency (EPA) recommends hydrogen peroxide for controlling SARS-CoV, but they recommend maintaining contact with the virus for 3 to 5 minutes for 1.5% hydrogen peroxide and up to 15 minutes for 0.5% hydrogen peroxide. The Food and Drug Administration (FDA) present many concepts for SARS-CoV-19, but the FDA has not approved the use of hydrogen peroxide for killing the SARS-CoV-2 [11-14]. The individual practitioner is in a pandemic situation with few options for protection. The following is presented as an editorial comment for professional review and use or avoidance as per the professional’s determination.
Editorial
The Perio Protect Method™ (Perio Protect LLC, St Louis, Mo) uses a 1.7% hydrogen peroxide gel (Perio Gel™) for 15 minutes to treat periodontal disease. In clinical trials 1.7% hydrogen peroxide is released from Perio Gel™ (Perio Protect LLC) at a constant level of 1.7% for over 17 minutes and long-term use of the Perio Protect Method™ without adverse tissue effects are demonstrated. This time of release fulfills the EPA guidelines of contact time with the virus and use of hydrogen peroxide fulfills the ADA recommendations for pre-treatment protection. A reservoir of medication is maintained for 15 minutes by using the Perio Tray™ (Pero Protect LLC), an FDA cleared medical device [15, 16].
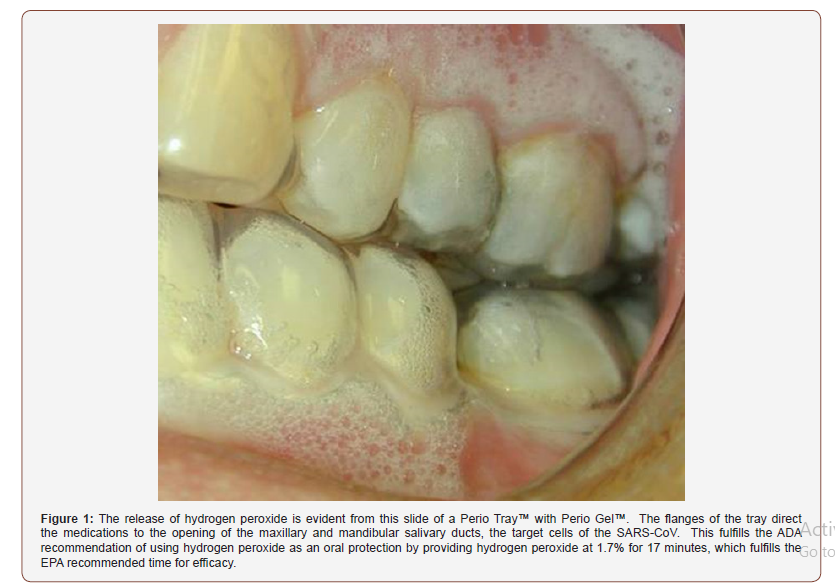
Liu [6] shows the SARS-CoV “target” cells for invasion are the epithelial cells of the salivary ducts. Use of the Perio Tray (Figure 1) applies a consistent presence of 1.7% hydrogen peroxide at the salivary duct openings for over 17 minutes. This use complies with the ADA and EPA recommendations. Prevention of infection may be enhanced by placing the Perio Tray™ with Perio Gel™ in the mouth and wearing a mask, but future studies are required [17-19].
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- M Ceccarelli, M Berretta, E Venanzi Rullo, G Nunnari, B Cacopardo (2020) Differences and similarities between Severe Acute Respiratory Syndrome (SARS)-Corona Virus (CoV) and SARS-CoV-2. Would a rose by another name smell as sweet? Eur Rev Med and Pharmacol Sci 24(5): 2781-2783.
- Arabi YM, Arifi AA, Balkhy HH, Hani Najm, Abdulaziz S Aldawood, et al. (2014) Clinical Course and outcomes of critically ill patients with Middle East Respiratory Syndrome coronavirus infection. Ann Intern Med 160: 389-397
- Anfinrud P, Bax C, Valentyn S, et al. Could SARS-Co-V be transmitted via speech droplets?
- Hoffmann M, Kleine Weber H, Schroeder S, Nadine Krüger, Tanja Herrler, et al. (2020) SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181(2): 271-280.e8
- Kai Wang K, Tak Yin Tsang O, Chik Yan Yip C, Kwok Hung Chan, Tak Chiu Wu, et al. Consistent detection of 2019 coronavirus in saliva. Clin Infect Dis.
- Liu L, Wei Q, Alvarez X, Haibo Wang, Yanhua Du, et al. (2011) Epithelial cells lining salivary gland ducts are early target cells of Severe Acute Respiratory Syndrome coronavirus infection in the upper respiratory tracts of Rhesus Macaques. J Virol 85(8): 4025-4030.
- (2020) The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The Epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19), China CDC Weekly 2: 113- 122.
- (2002) World Health Organization. Summary table of SARS cases by country.
- https://www.cdc.gov/coronavirus/2019-nCoV/index.html
- https://www.ada.org/en/publications/ada-news/2020-archive/march/ada-adds-frequently-asked-questions-from-dentists-to-coronavirus-resources
- https://www.cdc.gov/infectioncontrol/guidelines/disinfection/disinfection-methods/chemical.html
- Peng X, Xu X, Li Y, Lei Cheng, Xuedong Zhou, et al. (2020) Transmission routes for 20109-nCoV and controls in dental practice. Int J Oral Sci 12(1): 1-9.
- https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2
- https://www.fda.gov/media/136533/download
- Dunlap T, Keller DC, Marshall M (2011) Subgingival delivery or oral deb riding agents: a proof of concept. J Clin Dent 22(5): 149-158.
- Putt ibid
- Keller D, Buechel M Direct medications delivery modifies the periodontal biofilm.
- https://www.accessdata.fda.gov/cdrh_docs/pdf3/K031809.pdf
- Putt M, Malatt M, Messmann L, Howard M Proskin (2014) A 6-month clinical investigation of custom tray application of peroxide gel with and without doxycycline as adjuncts to scaling and root planning for treatment of periodontitis. Am J Dent 27(5): 273-284.
-
Duane C Keller. Perio Protect Method to Deliver Timed-Release Hydrogen Peroxide to the Salivary Ducts and the Oral Environment for Possible SARS-CoV-2 Protection. On J Dent & Oral Health. 2(5): 2020. OJDOH.MS.ID.000550.
-
Immature tooth, Necrotic teeth, Endodontic procedure , Apexification, Root resorption, Apical periodontitis , Root canal, Permanent teeth, Necrotic pulp.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






