 Case Report
Case Report
Oral Pigmentation as a Sign of Addison’s disease
Adel Bouguezzi1,2*, Hela Zouaghi1,2, Sameh Sioud1,2, Hajer Hentati 1,2 and Jamil Selmi1,2
1University of Monastir, Faculty of Dental Medicine of Monastir, Oral Health and Oro-Facial Rehabilitation Laboratory Research (LR12ES11), Tunisia
2Dental Clinic of Monastir, Department of Medicine and Oral Surgery, Tunisia
Adel Bouguezzi, University of Monastir, Faculty of Dental Medicine, 5019, Monastir, Tunisia.
Received Date: May 14, 2020; Published Date: May 26, 2020
Abstract
Addisonian skin hyperpigmentation, an important element of the pathology, is relatively rare, mucosal involvement is even less frequent. Likewise, there is little iconographic documentation of these pathologies. Addison’s disease is a primary adrenal failure caused by infiltrative or autoimmune processes. One of the most important signs of Addison’s disease is cutaneous and mucosal hyperpigmentation’s related to ACTH melanogenesis action. Pigmentation can be homogeneous or blotchy, it does not depend on gender or race. It may involve skin, oral cavity, conjunctiva and genitalia. It is more evident in areas exposed to the sun and under mechanical stimulations. Here, we describe a patient who was affected by brown maculae involving the oral cavity. Treatment with hydrocortisone allowed biological normalization and improvement of the general condition. Currently, the patient no longer has a systemic disorder, however the mucous hyperpigmentation persists.
Keywords: Addison’s disease; Oral pigmentation; Cortisol
Introduction
Careful examination of the mouth may reveal findings indicative of an underlying systemic condition and permit for early diagnosis and treatment. Etiology of acquired hyper pigmentation are many. In some patients it gives a clue to the diagnosis of systemic disorders. Addison’s disease could be a rare endocrine disease during which there’s destruction of the endocrine gland with resultant inadequate secretion of the adrenal cortical hormonescortisol, aldosterone and androgens. Cortisol, the most hormone affected is very important within the body’s ability to deal with stressful situation like infection, hypotension, and surgical procedures [1]. Primary adrenal insufficiency is a life-threatening disorder particularly in stressful situation, since cortisol secretion cannot be increased on demand at all. The prevalence of primary adrenal insufficiency (Addison’s disease) has been reported to be 39 to 60 per million population [2].
Observation
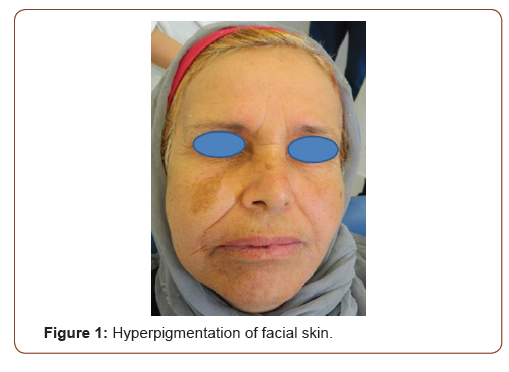
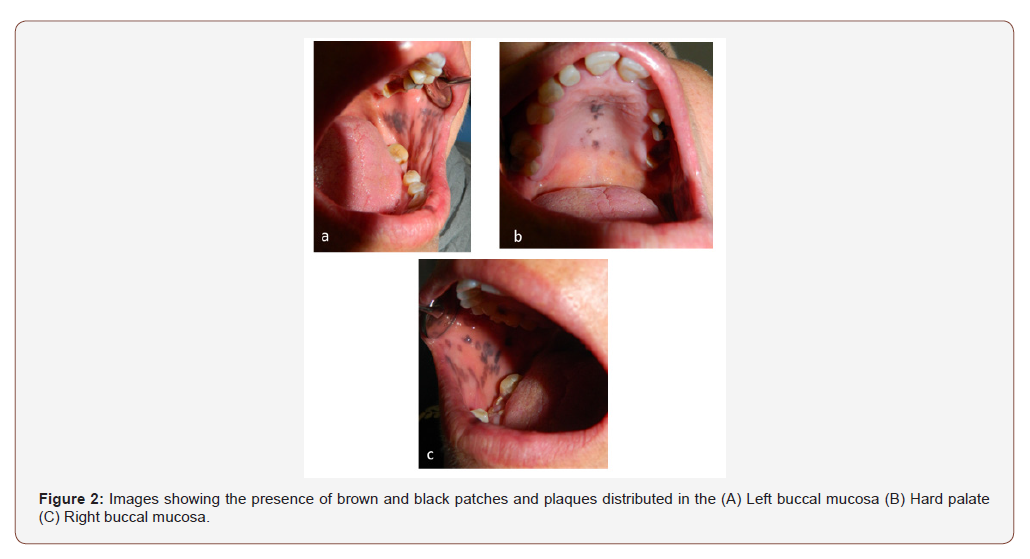
A 53-year-old female patient presented with anorexia, weight loss, hypotension, weakness, abdominal pain and black patches on the face and oral mucosa. During anamnesis, the patient reported that these patches had grown in recent months, the patches had persisted despite treatment with oral fluconazole, which had been prescribed empirically for presumed oral candidiasis. Results of a physical examination revealed scattered, asymptomatic, bluishblack macules these lesions were asymptomatic, had varying sizes with irregular and imprecise limits, and were located on the skin face and buccal mucosa (Figure 1, 2). No cervical lymphadenopathy was noted.
Our major diagnostic doubt was between diagnosing diffuse oral maculae because of melanosis or more serious systemic diseases associated to oral diffuse pigmentation like Peutz-Jeghers syndrome or Addison’s disease. Colonoscopy didn’t reveal intestinal polyps. Additionally, to low pressure level (110/60 mmHg), blood chemistry tests revealed low plasma cortisol associated to hyponatremia (120 mEq/l) and hyperkaliemia (6 mEq/l). Furthermore, a brief synacthen test (short corticotrophin test) was requested to verify adrenal insufficiency, during which impaired response to adrenocorticotropin hormone was found (240 pg/ ml; normal values = 6-60 pg/ml). Ultrasonography and MRI of the adrenal glands showed absence of any masses or swellings that would mimic a neoplasm producing ACTH or hemorrhages.
As a result of the above findings, a diagnosis of Addison’s disease was made. The patient was then addressed to the endocrinology division where she was managed for an accurate therapy of the disease. Treatment with hydrocortisone allowed biological normalization and improvement of the general condition. Currently, the patient no longer has a systemic disorder (clinical or biological), however the mucous hyperpigmentation persists.
Discussion
Hyperpigmentation of the oral mucosa (i.e., Addison disease) is the primary manifestation of primary adrenal insufficiency. However, diffuse melanin pigmentation of the oral mucosa could be a nonspecific finding, and diverse other conditions are also considered within the medical diagnosis (e.g., ethnic pigmentation, tobacco-related pigmentation, medication-related pigmentation, neurofibromatosis [3], McCune-Albright syndrome, Peutz-Jeghers syndrome). Primary adrenal insufficiency may occur in association with the autoimmune poly endocrino pathy candidiasisectodermal dystrophy syndrome, during this condition, chronic mucocutaneous candidiasis develops in childhood in conjunction with hypoparathyroidism and other findings ,within the mouth, candidiasis can present as pseudomembranous (white plaques that may be wiped away), hyperplastic (white plaques that can’t be wiped away), or erythematous. Skin and tissue layer hyperpigmentation is present in 95% of patients with primary adrenal insufficiency [4].
It’s considered a tell-tale sign of Addison’s disease, thus differentiating it from secondary and tertiary hypoadrenalism. This often precedes other manifestations by months to years, and therefore the patient can present with the sole complaint of getting darker. Moreover, with other systemic manifestations, it’s a high predictive value for Addison’s disease. It results from the stimulatory effect of ACTH on melanocytes. Other commonly involved areas are nail bed, palmar creases, buccal tissue layer, perianal and vaginal mucosa [5].
Diagnoses which will mimic the oral pigmentation of Addison disease include oral “black tongue” candidiasis, ethnic pigmentation, and reactions to certain drugs. Black furry tongue and hairy tongue candidiasis are disorders believed to be caused by candida and infrequently Aspergillus species. These conditions are related to long run use of antibiotics. Characterized by dense, black, bluish-black, or brown “matted” areas of the dorsal surface of the tongue, hairy tongue candidiasis is successfully eliminated by discontinuation or minimization of antibiotics, gentle brushing of the tongue surface, and use of an oral antifungal agent [6] the foremost common pattern of ethnic or racial pigmentation could be a band of pigment at the junction of attached and alveolar mucosa. In contrast to Addison disease, pigmentation on the tongue of these with skin of color is often localized to isolated groups of filiform papillae [7]. Such pigmentation, usually found only in persons with dark skin, can also be found as isolated pigmented patches in 5% of Caucasians. Drug-induced pigmentation can range from brown (seen with oral contraceptives, cytotoxic agents, and a few anticonvulsants) to yellow or blue-black (as seen with the antimalarial drugs quinacrine, chloroquine, and hydroxychloroquine) [8]. Long-term use of minocycline has been related to a blue-gray staining of the tongue, gingival margins, palate, and pretibial surfaces [9].
Acknowledgement
None.
No conflict of interest.
No conflict of interest.
References
- Wolfgang O (1996) Adrenal insufficiency. N Engl J Med 335: 1206-1212.
- May M E, Vaughn ED, Carey RM (1989) Adrenocortical insufficiency-clinical aspects. In: Vaughan ED, Carey RM (Eds). Adrenal disorders. 171-189, New York, USA.
- Shah SS, Oh CH, Coffin SE (2005) Addisonian pigmentation of the oral mucosa. Cutis 76(2): 97-99.
- Zargar AH, Laway BA, Masoodi SR (2001) A critical evaluation of signs and symptoms in the diagnosis of Addison’s disease. J Assoc Physicians India 49: 523-526.
- Chakera AJ, Vaidya B (2010) Addison’s Disease in Adults: Diagnosis and Management. Am J Med 123: 409-413.
- Wolf IJ (1970) Black tongue moniliasis. Pediatrics 46: 164-165.
- Leston JM, Santos AA, Varela Centelles PI (2002) Oral mucosa: variations from normalcy, part II. Cutis 69: 215-217.
- Kleinegger CL, Hammond HL, Finkelstein MW (2000) Oral mucosal hyperpigmentation secondary to antimalarial drug therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90: 189-194.
- Strakosch CR, Gordon RD (1978) Early diagnosis of Addison’s disease; pigmentation as sole symptom. Australian and New Zealand Journal of Medicine 8(2): 189-190.
-
Adel Bouguezzi, Hela Zouaghi. Oral Pigmentation as a Sign of Addison’s disease. On J Dent & Oral Health. 3(1): 2020. OJDOH. MS.ID.000551.
-
Etiology, Hormones cortisol, Hyper pigmentation, Systemic disorders, Oral mucosa, Abdominal pain, Tongue, Tobacco pigmentation, Dystrophy syndrome.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






