 Case Report
Case Report
Heterotopic Bone Formation After Alloplastic Temporomandibular Joint Reconstruction-Case Report
Ryuichi Hoshi1*, Paula Marcella Silva Drago2, Daniel Serra Cassano2, Fernanda Barros Silva de Pedreira Barbosa2, Lissa Hoshi3 and Isadora dos Santos Lima1
1UNIFTC-Medicine school, Brazil
2Private Clinic, Brazil
3IAMSPE Hospital, Brazil
Ryuichi Hoshi, UNIFTC-Medicine school, Brazil.
Received Date: September 05, 2023; Published Date: September 13, 2023
Abstract
The term heterotopic ossification (OH) describes the pathological situation in which there is formation of bone tissue outside the skeleton. It is defined as the presence of bone tissue in places where there is normally no bone. The etiology is still unknown, but several factors have been studied as responsible for osteoblastic activation existing in the disease, such as trauma caused by an accident, surgical treatment or genetic disorders. Customized temporomandibular joint (TMJ) prostheses have become an essential option in the treatment of joint reconstructions, proving to be safe, reliable and durable. However, some immediate and long-term complications, among them, heterotopic ossification after its installation, have been reported. This study presents the formation of heterotopic bone after a hemimandibulectomy for tumor treatment, and reconstruction with a customized prosthesis of the temporomandibular joint.
Keywords:Heterotopic ossification; Temporomandibular joint; Joint replacement
Introduction
Heterotopic Ossification (HO) is the presence of bone in nonosseous tissues, or more accurately, formation of ectopic lamelar bone in muscles or joint apparatus. The outcome of such bone formation is limitation of muscular mobility and subsequent joint immobility. HO is most frequently associated with musculoskeletal trauma, amputations, spinal cord injury, tumors, vasculopathies, or central nervous system injury. Three types are described:: myositis ossificans circumscripta, myositis ossificans progressiva and localized traumatic myositis ossificans. Furthermore, genetic disorders such as fibrodysplasia ossificans progressive and progressive osseous heteroplasia have been linked to HO [1, 2]. TMJ prostheses have become an essential treatment option for reconstruction of mandibular joint. They are a safe, reliable, and effective treatment option for selected TMJ disorders. However, long-term complications have been reported, one of them being: heterotopic bone formation [3, 4].
When heterotopic ossification is suspected clinically, radiographic exams may identify the location and extent of disease. Because serum calcium, phosphorus, and alkaline phosphatase levels are not routinely reliable for the diagnosis or prognostic of heterotopic ossification, radiographic imaging and clinical history are of most importance. Plain radiographs are commonly the first imaging study used to detect heterotopic ossification1. The advantages of radiographs are low cost and easily available images. The disadvantage is the difficulty of visualizing the anatomic extent of ectopic bone deposition early in the disease process [5].
The present manuscript describes a case of heterotopic bone formation parallel to a total temporomandibular joint prosthesis that occurred several years after the implant.
Case Report
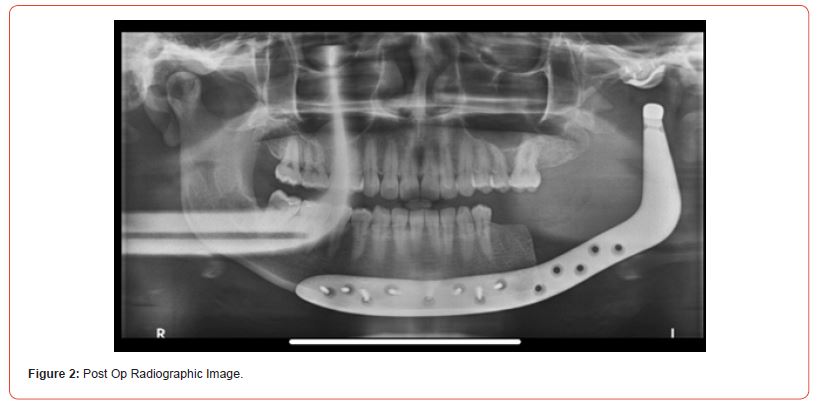
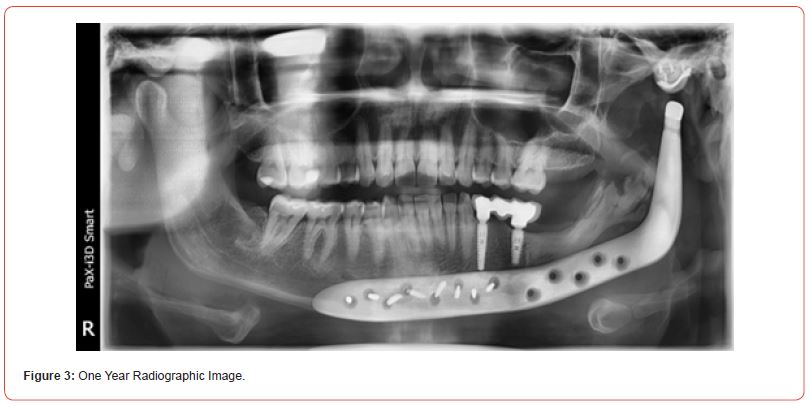
Female patient, presenting an asymptomatic volume increase associated with the dental unit in the left mandibular ramus (Figure 1). Incisional biopsy was performed, with a diagnosis of keratocyst odontogenic tumor. After discussing several treatment options it was decided on the resection of the lesion and replacement of the affected region with a joint prosthesis customized with mandibular extension and implantation of fat graft. The project for the customized mandibular prosthesis was carried out by TMJ Concepts System® (Ventura, CA). The prosthesis was manufactured in wax and later printed in titanium. The surgery did not present complications and the patient followed-up with routine radiographs (Figure 2). After one year, a control panoramic radiography showed bone growth in the region of mandibular resection laterally to prosthesis toward the mandibular condyle (Figure 3), compatible with a diagnosis of heterotopic ossification. The patient is currently undergoing clinical and radiographic follow-up without any symptoms.

Discussion
The odontogenic keratocyst (OKC) is a common cystic lesion of the jaw. Its management, however, is highly debated with no consensus on the best treatment option. Clinicians base their approach on treatment efficacy and associated morbidity. There is no consensus on the best method to remove these cysts. With a broad spectrum of treatment modalities, clinicians base their choice on the treatment’s efficacy in comparison with its morbidity in a patient-specific manner. Complete or partial resection has the lowest recurrence (less than 2%) but is associated with major morbidity. Radical resection remains the best option for obtaining the lowest recurrence rates with OKC [6].
The etiological mechanisms at molecular and cellular level leading to HO are not well understood. However, recent studies suggest that the innate immune system, central and peripheral nervous systems, and inflammation trigger the development of HO. Classically, the clinical signs and symptoms of HO, such as pain with joint move-ment and restricted joint mobility and function, develop 3-12 weeks after trauma or joint replacement surgery. Since the early signs and symptoms of HO are relatively non-specific, diagnosis can be difficult. The diagnosis of HO is primarily based on imaging. Conventional imaging techniques (plain films, computed tomography (CT), and magnetic resonance imaging (MRI)) and three-phase bone scanning demonstrate bone formation and confirm the diagnosis [7, 8].
Mandible segmental defects caused by resection surgery can lead to disfiguring and disabling conditions. Restoring facial function and esthetics become a challenge in mandibular reconstruction, especially when the temporomandibular joint (TMJ) is involved [4].
TMJ resection, together with mandibular segment, results in malocclusion, mastication difficulty, trismus, and posterior mandibular height loss; its reconstruction is a great challenge1. Reestablishing an adequate posterior mandibular height and a functional joint that allows maintenance of a range of motion is quite difficult using only bone grafts/flaps. Customized prosthetic devices are a great tool for joint reconstruction, and the best choice to obtain results as close as possible to the desired result, since an ideal reconstruction includes mobility without interferences, while the full support of the masticatory muscles is desired and offering a better facial contour. Virtual planning technological advances have allowed the manufacturing of customized three-dimensional prostheses, enabling better adaptation [9].
Conclusion
The present report describes a case of heterotopic bone formation laterally to a total alloplastic prosthesis of the temporomandibular joint. Although this adverse event has sometimes been described in the literature, growth through the remaining mandibular ramus has yet to be reported.
Patient Consent
Written patient consent was obtained to publish the clinical case and photographs
Acknowledgements
None.
Conflict of Interest
No Conflict of interest.
Ethical Approval
Not applicable.
Funding
Not applicable.
References
- Bossch L Vanden, Vanderstraeten G (2005) Heterotopic ossification: A review. J Rehabil Med 37(3): 129-136.
- Ranganathan K, Loder S, Agarwal S, Wong VW, Forsberg J, et al. (2014) Heterotopic ossification: Basic-science principles and clinical correlates. J Bone Joint Surg Am 97(13): 1101-1111.
- Jihad Salman N, dos Santos Trento G, Henrique de Azambuja Carvalho P, Aparecida Cabrini Gabrielli M, Francisco Real Gabrielli M, et al. (2021) Heterotopic Ossification Around Temporomandibular Joint Prosthesis: Case Report and a Scoping Review.
- Lee YW, You HJ, Jung JA, Kim DW (2018) Mandibular reconstruction using customized three-dimensional titanium implant. Arch Craniofac Surg 19(2): 152-156.
- Ringold S, Thapa M, Shaw EA, Wallace CA (2011) Heterotopic ossification of the temporomandibular joint in juvenile idiopathic arthritis. J Rheumatol 38(7): 1423-1428.
- Al Moraissi EA, Dahan AA, Alwadeai MS, Oginni, FO, Al Jamali, JM, et al. (2017) What surgical treatment has the lowest recurrence rate following the management of keratocystic odontogenic tumor?: A large systematic review and meta-analysis. Journal of Cranio-Maxillofacial Surgery 45(1): 131-144.
- Guarda Nardini L, Manfredini D, Olivo M, Ferronato G (2014) Long-Term Symptoms Onset and Heterotopic Bone Formation around a Total Temporomandibular Joint Prosthesis: a Case Report. J Oral Maxillofac Res 5(1).
- Selbong U, Rashidi R, Sidebottom A (2016) Management of recurrent heterotopic ossification around total alloplastic temporomandibular joint replacement. Int J Oral Maxillofac Surg 45(10): 1234-1236.
- Qassemyar Q, Assouly N, Temam S, Kolb F (2017) Use of a three-dimensional custom-made porous titanium prosthesis for mandibular body reconstruction. Int J Oral Maxillofac Surg 46(10): 1248-1251.
-
Ryuichi Hoshi*, Paula Marcella Silva Drago, Daniel Serra Cassano, Fernanda Barros Silva de Pedreira Barbosa, Lissa Hoshi and Isadora dos Santos Lima. Heterotopic Bone Formation After Alloplastic Temporomandibular Joint Reconstruction-Case Report. On J Dent & Oral Health. 7(2): 2023. OJDOH.MS.ID.000658.
-
TMJ disorders, Odontogenic tumor, Jaw, Reconstruction, Heterotopic ossification, Genetic disorders, Joint reconstructions, Spinal cord injury, Calcium, Implant
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






