 Case Report
Case Report
Foreign Body Penetration into the Infra-Temporal Fossa: A Previously Misdiagnosed Case
Mahmoud Hamasha1, Shatha Al Momani2* and Rana Mohammed3
1Princess Basma Hospital, Department of Oral and Maxillofacial Surgery, Ministry of Health, Irbid Jordan
2Jordan University of Science and Technology, Faculty of Dentistry, Department of Conservative Dentistry, Irbid 22110, Jordan
3Al-Ramtha main health centre, Department of Dentistry, Ministry of Health, Al-Ramtha, Jordan
Shatha Al Momani BDS, MSc(Clin), J Board Lecturer and Dental Specialist Department of Conservative Dentistry Faculty of Dentistry Jordan University of Science and Technology, P.O Box 3030 Irbid 22110, Jordan.
Received Date: June 03, 2023; Published Date: August 09, 2023
Abstract
Cases of foreign bodies penetrating the infratemporal fossa are rare and could be difficult to diagnose or treat. This report describes the diagnosis and surgical management of a previously misdiagnosed foreign body penetrating the infratemporal fossa and discusses the anatomical implications.
Keywords:Infra-temporal fossa; foreign body; IV contrast; CT-scan
Introduction
Injury cases involving foreign bodies penetrating the infratemporal fossa (ITF) are rare and can often be misdiagnosed due to lack of adequate examination, history taking, and appropriate diagnostic imaging techniques. Missed or delayed diagnosis of such cases can lead to life threatening complications, ranging from infection to loss of function [1]. Moreover, surgical retrieval of the foreign bodies can be challenging because of the close proximity to neurovascular structure. Several techniques have been reported for surgical retrieval of foreign bodies from ITF, depending on the location and size of the object [2-4].
In this report, we describe the management of a previously misdiagnosed foreign object (fractured pencil) penetrating the infra temporal fossa superio-lateral to the left orbit and extending to the body of sphenoid bone. The report discusses the clinical strategies applied to identify and retrieve the object, while limiting the potential complications associated with this type of facial injury.
Case Report
A Sixteen years old male presented to the maxillofacial surgery clinic complaining of severe headache and pain on the left side of the head after a fall accident that occurred one month ago.
At the time of the accident, the patient was admitted to the emergency room at Princes Basma teaching hospital due to a fall accident on dirty playground as described by his mother. A small cut wound in the left temporal area behind the orbit was detected. A CT scan was requested to the head with no abnormality detected. The wound was cleaned, irrigated with normal saline and packed. Two weeks later, the patient started experiencing headache, limited mouth opening and tenderness over the wound area, in addition to pus discharge from the wound. Accordingly, the patient visited the primary care center, in which the wound was re-cleaned and the dressing replaced. Antibiotics and additional pain killers were also prescribed.
One month after the fall accident, the patient came to the maxillofacial surgery clinic at Princess Basma hospital complaining of severe headache, trismus, and pus discharge. The headache was described as sever, spontaneous, not relieved by non-steroidal antiinflammatory drugs and radiating from the left periorbital region extending to occipital area of the head. Upon clinical examination, the left peri-orbital area was very tender with localized swelling located lateral and superior to the left orbit in the temporal region. Pus discharge was detected from a sinus tract located 1.5cm superior-lateral to the left orbit. A palpable hard object was felt few millimeters medial to the discharging sinus tract causing tenting and tenderness of the overlying skin.
The inter-incisal distance at maximum mouth opening was 20mm. There was pain in the temporal area on eating. The dental occlusion was normal. The patient was fully conscious, oriented and there was no active bleeding when he came to our clinic. Examination of the sensorimotor function showed no abnormal sensation and the facial nerve function was not affected. Eye examination showed no tenderness, normal visual acuity, no diplopia, and normal eye movement in all directions.
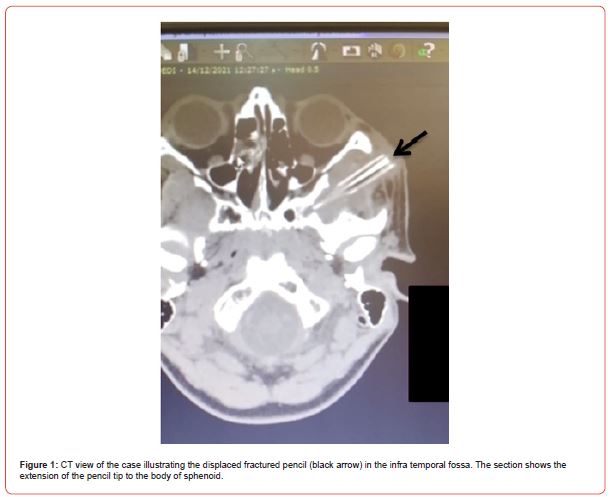
A CT scan with IV contrast was requested since the previous CT scan did not show any abnormalities. The new CT scan detected a foreign body similar in shape to a fractured pencil, with a length of 4.5cm, a diameter of approximately 0.4cm, and a tapered pointed tip. The foreign body was located in the infra temporal fossa extending from a location superior-lateral to the left orbit above the zygomatic arch and reaching the body of sphenoid (Figure 1).
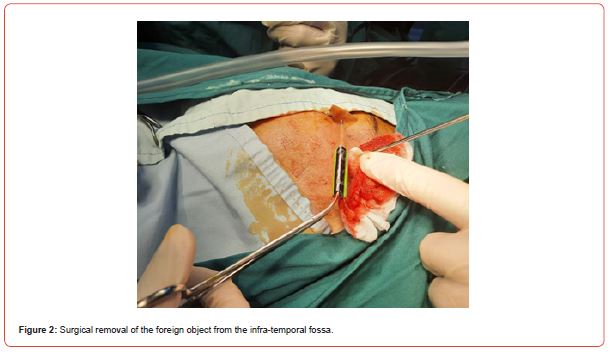
The patient was immediately admitted to the hospital and prepared for surgical removal of the object. Parents’ approval was granted after being informed about the risks of surgery. The treatment plan included attempted removal of the foreign body under general anesthesia and through direct skin incision over the palpable foreign body (Figure 2).
Surgery was conducted while patient in supine position and the head tilted to the opposite side of injury. The skin incision extended 2cm in length over the foreign object, and located 1.5 cm lateral and superior to the lateral orbital wall and parallel to the relaxed skin tension lines for cosmetic considerations. 3% articaine local anesthesia with 1/100000 epinephrine was injected subcutaneously along the planned incision. The incision was applied through the skin and the subcutaneous layer. The foreign body (fractured pencil) became visible and appeared to be loose. The object was carefully released from the surrounding tissue and removed in a direction parallel to its insertion path, without applying pressure and with minimal force in order to ensure one piece removal and to avoid leaving any fragments behind or causing damage to the surrounding structures (Figure 2).
The fractured pencil body was completely removed and the surgical area propped and checked gently confirming no fragments left. The wound was irrigated vigorously with normal saline and hemostasis achieved. The incision was closed in layers, the subcutaneous layer sutured using 3/0 vicryl, while the skin layer sutured using 5/0 nylon. Dressing pack was applied and no drainage indicated.
Patient was checked post-surgery after being fully conscious. The facial nerve examination showed no weakness or impairment. Examination of orbit shows no negative effect on vision or eye movement with normal reflexes. A Neuro-ophthalmology specialist was consulted and reported no abnormalities or complications detected. Post-operative CT scan with IV contrast confirmed no fragments left in the wound.
Post-operative medications were prescribed; paracetamol 500mg i.v as analgesic, ceftriaxone twice daily as antibiotic and dexamethasone 8 mg . Soft diet was recommended for the next few days.
The patient was discharged from the hospital three days postoperation. Sutures were removed five days later and patient reevaluated for any complications. Mouth opening to the normal range was achieved one week after surgery. At one month follow-up, patient showed full recovery with no neurological or ophthalmological complications.
Discussion
The infratemporal fossa is the space between the skull base, lateral pharyngeal wall, and the ramus of mandible [5]. It serves as the passageway for several important neurovascular structures such as the maxillary artery and branches, pterygoid venous plexus, mandibular nerve and branches, chorda tympani nerve, and the posterior superior alveolar nerve [5]. Therefore, delayed diagnosis and treatment of foreign objects penetrating the ITF could lead to life threatening complications.
The density of some foreign objects could be very similar to that of the surrounding soft tissues, which often results in delayed or missed diagnosis [6]. The use of IV contrast greatly improves the accuracy of the examination and assists excluding many life threatening conditions. IV contrast is mainly used to highlight differences between structures which would otherwise look the same. This could explain the misdetection of the wooden pencil fragment in the ITF during the first CT scan in the current case, while clearly detected using a second CT scan with IV contrast (Figure 1).
Removal of foreign bodies from the ITF is surgically challenging and fraught with risks [7]. Bleeding complications and infections related to extraction of such foreign bodies following arterial injuries has been reported in the literature [8]. Such injuries can be surgically uncontrollable and therefore potentially fatal [9]. In the present case, the pencil fragment was located on the superior part of the infra-temporal fossa, our surgical approach was to apply a 2cm skin incision directly over the palpable object. The main concern with this approach was the proximity of the fronto-zygomatic branch of facial nerve to the incision line, which could lead to further esthetic and numbness complications. The alternative surgical approach in case of foreign body or fragments removal difficulty was to adopt a hemi-coronal flap incision with wider exploration. This technique involves higher risk of complications including; bleeding, hematoma, larger scar and alopecia along the incision line, in addition to potential facial nerve weakness. The possible migration of the foreign body during attempted removal in the ITF was also considered carefully, as this could jeopardize additional critical structures, such as those within the infraorbital fissure, which could result in visual complications [4].
In the current case, several technical procedures have been followed in order to minimize the potential complications associated with foreign body removal from ITF. The preoperative IV contrast CT scan image ensured accurate foreign body detection and localization. The adequate surgical exposure achieved through 2 cm long incision, in addition to efficient bleeding control, and the avoidance of extensive manual palpation within the ITF ensured minimal complications during or post-surgery.
Early detection of foreign bodies in the infratemporal fossa following facial injury could be achieved by a thorough clinical and radiological examination, limiting the risk of infection and endangering additional critical structures. The use of IV contrast CT scan will enhance early diagnosis of foreign bodies penetrating the ITF.
Funding
None.
Competing interest
None.
Introduction
The authors have no conflicts of interest to disclose.
Ethical approval
Not applicable.
Patient Consent
Written patient consent was obtained to publish the clinical case and photographs.
The manuscript has been read and approved for submission by all authors.
References
- John SS, Rehman TA, John D, Raju RS (2008) Missed diagnosis of a wooden intra-orbital foreign body. Indian J Ophthalmol 56: 322.
- Villarmé A, Savoldelli C, Jean Baptiste E, Guevara N (2018) Multidisciplinary surgical management of an unusual penetrating foreign body of the face. Eur Ann Otorhinolaryngol Head Neck Dis 135: 361-363.
- Lehmann AE, Scangas GA, Jafari A, Metson R (2020) Endoscopic Transoral Image-Guided Retrieval of Infratemporal Fossa Foreign Bodies. OTO open 4: 2473974X20947026.
- Ioanidis K, Rotenberg B (2018) A needle in a haystack: Endoscopic removal of a foreign body from the infratemporal fossa. Allergy Rhinol (Providence) 9: 2152656718764142.
- Casale J, Bordoni B (2021) Anatomy, Head and Neck, Infratemporal Fossa. StatPearls [Internet].
- Myllylä V, Pyhtinen J, Päivänsalo M, Tervonen O, Koskela P (1987) CT detection and location of intraorbital foreign bodies. Experiments with wood and glass. Rofo 146: 639-643.
- Battisti A, Priore P, Giovannetti F, Barber, G, D’alessandro F et al. (2017) Rare complication in third maxillary molar extraction: Dislocation in infratemporal fossa. J Craniofac Surg 28: 1784-1785.
- Wulkan M, Parreira, JG, Botter DA (2005) Epidemiology of facial trauma. Rev Assoc Med Bras 51: 290-295.
- Tan SS, Yeo M, Lee G, Ho M, Ang M, et al. (2016) Penetrating foreign body in the masticator space with injury to the internal maxillary artery: a surgical challenge. Ann R Coll Surg Engl 98: e194-e196.
-
Mahmoud Hamasha , Shatha Al Momani* and Rana Mohammed. Foreign Body Penetration into the Infra-Temporal Fossa: A Previously Misdiagnosed Case. On J Dent & Oral Health. 7(2): 2023. OJDOH.MS.ID.000656.
-
Maxillary artery, Dental occlusion, Periorbital region, Headache, Dentistry, Facial injury, Maxillofacial surgery, CT Scan, Lateral pharyngeal wall
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






