 Case Report
Case Report
Focal Acantholytic Dyskeratosis in Non-Keratinized Tissue: A Case Report
Brianna Ingram1, Richa Vyas1, Andres Flores2 and Iquebal Hasan2 *
1East Carolina University School of Dental Medicine, USA
2Department of Surgical Sciences, East Carolina University School of Dental Medicine, USA
Iquebal Hasan, Department of Surgical Sciences, East Carolina University School of Dental Medicine, USA.
Received Date: November 29, 2021; Published Date: December 13, 2021
Abstract
Focal acantholytic dyskeratosis (FAD) is an uncommon cutaneous lesion with an even rarer presentation in the oral cavity. While the condition is mostly limited to the head and neck region, there have been less than 50 cases reported in the oral cavity. Clinical presentation of the lesion is similar to many other conditions and a biopsy of the lesion can help to identify the condition due to its distinctive histopathological features. The purpose of this case report is to present a new case of focal acantholytic dyskeratosis in an extremely rare location, the right oral vestibule, in a 75-year-old Caucasian woman.
Keywords:Focal acantholytic dyskeratosis; Warty dyskeratoma; Isolated Darier’s disease
Introduction
Focal acantholytic dyskeratosis (FAD), also previously referred to as warty dyskeratoma or isolated Darier’s disease, is a condition characterized by cutaneous lesions, which can rarely present in the oral cavity. “In 1972, Akerman established different subtypes of FAD:
1) Clinically nonsuggestive solitary lesions that showed histopathological areas of FAD,
2) Popular lesions with multiple histopathological areas of FAD,
3) Nodular lesions with only one histopathological area of FAD (warty dyskeratoma) and
4) Systemic disorders with multiple lesions similar to Darier disease [1].
Fewer than 50 cases of focal acantholytic dyskeratosis have been reported in the oral cavity. The reported lesion usually appeared as asymptomatic, solitary, white nodules, papules, or patches on bonebound mucosa, sometimes with a ‘rough surface’ and a depressed center. Males were affected slightly more than females, and the lesions were most common in the fifth to seventh decade of life [2]. FAD has been reported as cutaneous lesions involving the scalp [3], eyelids [4], lip [5], vagina [6], and perianal region [7]. The etiology of the cutaneous presentation is primarly unknown, but it is accepted that it derives from the pilosebaceous unit, which cannot be said for the oral cavity presentation as the oral cavity lacks hair follicles. The data of the current literature revealed that smoking appears to be the most prevalent predisposing factor [2].
Case Presentation
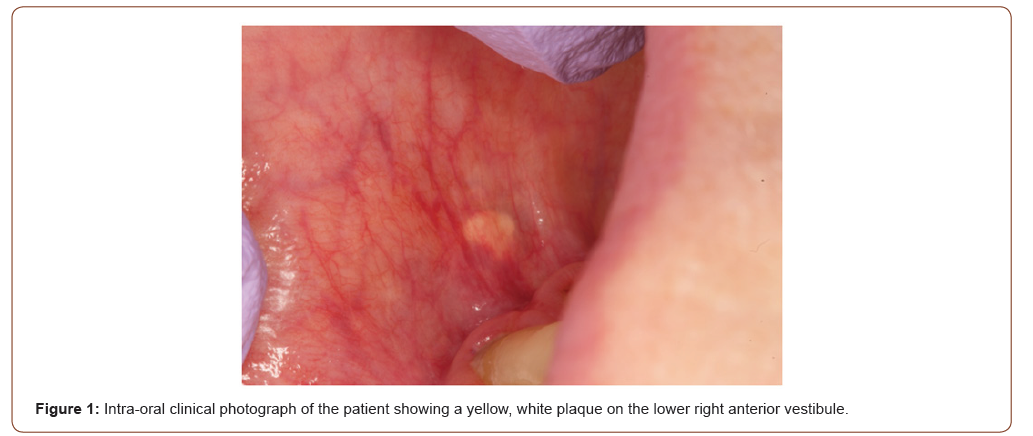
A 75-year-old Caucasian female presented for evaluation of a tender lesion in the lower right vestibule, to the East Carolina School of Dental Medicine. The patient medical history disclosed gastroesophageal reflux disease, diabetes, hypothyroidism, hyperlipidemia, degenerative disc disease, and osteopenia. The patient’s medications include omeprazole, levothyroxine, gemfibrozil, multi-vitamins, and calcium. No significant family or social history was identified. The clinical evaluation revealed a yellowish white plaque-like area in the right mandibular facial vestibule, measuring 2mm x 3mm (Figure 1, 2). Initial treatment of the area included dexamethasone elixir and clobetasol gel. The area was non-responsive to this line of treatment, and corticosteroid injections were given as a second line of treatment. Due to the patient’s previous Lichen Planus diagnosis, multiple low-dose triamcinolone acetonide (Kenalog) corticosteroid injections were administered to the right lower vestibule where the tender yellowish white plaque was located.
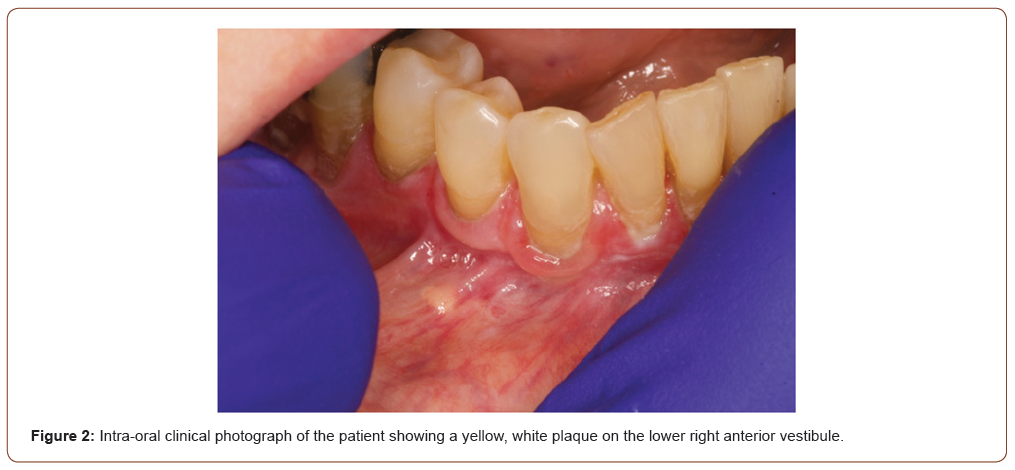
At the subsequent re-evaluation, the previously noted yellowish white plaque-like area in the mandibular right facial vestibule was noted as tender and measured 4mm x 2mm. The lesion was determined unresponsive to corticosteroid treatment and demonstrated a 1mm increase in size. At the time, the clinical differential diagnoses included Fordyce granules, verruciform xanthoma, lipoma. An excisional biopsy was performed under local anesthesia, and a Vicryl 4’0’ suture was placed on the surgical site. At the postsurgical follow-up appointment, the patient was asymptomatic, and the lesion was completed excised.
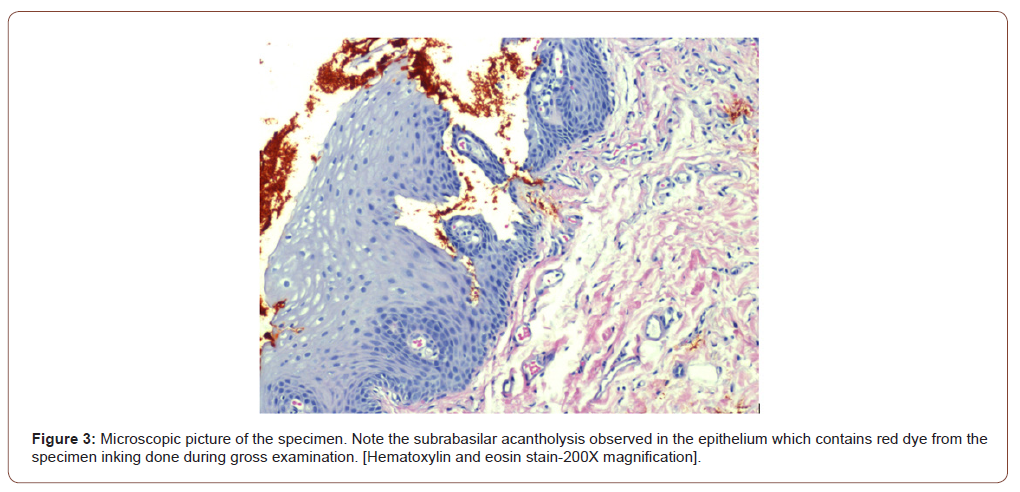
Microscopic examination revealed an elevated fragment of oral mucosa surfaced by hyperkeratotic and acanthotic stratified squamous epithelium, characterized by subrabasilar acantholytic clefts on the basal cell layer. The supporting stroma contained a mild inflammatory cell infiltrate mainly composed of lymphocytes underlying the covering tissue (Figure 3). The submitted specimen contained microscopic features consistent with focal acantholytic dyskeratosis. Biopsy results gave a final diagnosis of focal acantholytic dyskeratosis (Warty Dyskeratoma).
Discussion
Focal acantholytic dyskeratosis (FAD) is a rare benign lesion that typically presents as white plaque or papule usually <5cm in size. In our literature review, we found that FAD oral lesions are most prevalent within the fifth to seventh decades of life with a slight male predominance [2]. The case presented is a 75-yearold Caucasian female with a yellowish white plaque on the right lower vestibule. The location of our FAD nodule was unique as most lesions presented from a few weeks up to a year and existed on keratinized mucosa of the palate, alveolar ridge, and gingiva [2]. The patient’s FAD was present on the right lower vestibule, a non-keratinized tissue, giving a particular case of FAD an even rarer clinical presentation. The histopathological differential diagnoses of oral FAD include several entities with a subrabasilar acantholytic pattern, such as acantholytic acanthoma, Hailey-Hailey disease, pemphigus vulgaris, and Darier disease [8]. There is some history of successful treatment of Darier disease with corticosteroids [8]; however, diagnostic excisional biopsy appears to be curative [9]. The literature reviewed for this report does not indicate cases associated with malignant transformation or recurrence after an excisional biopsy [9].
While the etiology of FAD is unknown some of the suspected etiologic factors include tobacco usage, alcohol usage, benign trauma, immunosuppression, ill-fitting dentures, and cheek biting. The data currently present to us suggests that 60% of the 41 reported lesions appear in smokers [2]. While our patient does not have a history of smoking, we suspect trauma or immunosuppression to have a supporting role in the development of FAD. It has also been proposed that the oral form of FAD is a sort of immune response as autoantibodies were found in the serum of one reported case [2]. Current literature suggests that drug-induced immunosuppression can lead to the development of different benign and malignant skin neoplasms [10]. With this report, we propose to extend this consideration to focal acantholytic dyskeratosis of the oral mucosa, as our patient was on immunosuppressive agents to manage her arthritis and hypothyroidism. Our patient’s specific risk factors for oral FAD presentation included an immunosuppressive regimen consisting of dexamethasone and levothyroxine. To the best of our knowledge, this is the first report of an oral focal acantholytic dyskeratosis within non-keratinized tissue associated with these predisposing conditions.
Conclusion
As focal acantholytic dyskeratosis has only been reported in the oral cavity in less than 50 instances, this case report allows for an increase in current understanding of an uncommon oral lesion. This report can add to the knowledge base of FAD lesions in the oral cavity, which are not commonplace and regularly encountered by oral cavity healthcare providers. Allon and Buschner’s published comprehensive review of oral FAD is the only review of its kind, with the remaining published information coming from case reports. This case serves as another source of information regarding FAD in the oral cavity and can advance the knowledge of this rare condition. Dentists should be familiar with FAD in the oral cavity, its identification, diagnosis, and management.
Acknowledgement
The authors would like to acknowledge and thank Jamie Bloss for her contributions to this manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Ackerman AB (1972) Focal acantholytic dyskeratosis. Arch Dermatol 106(5): 702.
- Allon I, Buchner A (2011) Warty dyskeratoma/focal acantholytic dyskeratosis-an update on a rare oral lesion. J Oral Pathol Med 41(3): 261-267.
- Zhao Q, Zhou H, Geng S (2019) Multiple warty dyskeratoma on the scalp. An Bras Dermatol 94(5): 630-631.
- Phelps PO, Hinshaw MA, Potter HD (2015) Warty dyskeratoma of the eyelid. Ophthalmology 122(7): 1282.
- OʼConnell BM, Nickoloff BJ (1987) Solitary labial PAPULAR Acantholytic dyskeratoma in an Immunocompromised Host. Am J Dermatopathol 9(4): 339-342.
- Kerr PE, Murphy MJ (2017) Warty (follicular) dyskeratoma on the mons pubis. Int J Womens Dermatol 3(3): 154-156.
- Warkel RL, Jager RM (1986) Focal Acantholytic dyskeratosis of the anal canal. Am J Dermatopathol (4): 362.
- Lafuente‐Ibáñez de Mendoza I, Mosqueda‐Taylor A, Aguirre‐Urizar JM (2020) Focal acantholytic dyskeratosis: A multifocal verrucous presentation in the oral cavity. Int J Dermatol 60(1): 107-109.
- Zunt Susanl, Tomich Charlese (1990) Oral focal acantholytic dyskeratosis. J Dermatol Surg Oncol 16(6): 510-515.
- Pezzolo E, Colato C, Del Giglio M, Tessari G, Girolomoni G (2013) Acantholytic dyskeratotic acanthoma in an immunosuppressed patient: a case report with review of the literature.
-
Brianna Ingram, Richa Vyas, Andres Flores, Iquebal Hasan. Focal Acantholytic Dyskeratosis in Non-Keratinized Tissue: A Case Report. On J Dent & Oral Health. 5(2): 2021. OJDOH.MS.ID.000609.
-
Oral cavity, Gingiva, Inflammatory cell, Final diagnosis, Local anesthesia, Non-Keratinized Tissue, Right oral vestibule, Oral mucosa, Oral lesion.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






