 Case Report
Case Report
Embryonic Yolk Sac Tumor of Mandible: A Rare Entity with Clinicopathological Features and Literature Review
Muhammad Saeed1, Muhammad Athar Khan2*, Muhammad Kashif3, Muhammad Gulzar4, Muhammad Shahzad Ansari5 and Nizam6
1HOD, Oral & Maxillofacial Surgery Department, Bakhtawar Amin Medical College, Multan, Pakistan
2Associate Professor, Oral & Maxillofacial Surgery Department, Bakhtawar Amin Medical College, Multan, Pakistan
3Associate Professor, Oral Pathology , Department, Bakhtawar Amin Medical College, Multan, Pakistan
4Assistant Professor OMFS, BAMDC, Multan, Pakistan
5Assistant Professor, Oral pathology Department, Bakhtawar Amin Medical College, Multan, Pakistan
6Registrar OMFS
Muhammad Athar Khan, Associate Professor, Oral & Maxillofacial Surgery Department, Bakhtawar Amin Medical College, Multan, Pakistan.
Received Date: March 16, 2023; Published Date: March 24, 2023
Abstract
The present case report is about 1 and half year old boy presented with the complaint of aggressively growing swelling on right side of the face. This large tumour was extending from body of the mandible to the ramus of ipsilateral side of the face. Due to difficulty in mouth opening, intraoral examination could not be possible. Considering the aggressive behavior of the tumour, immediate surgery was planned and tumour was excised completely and excised mass had been processed for histopathological examination. Based on clinical, radiographic, histopathological and immunohistochemical findings, the lesion has been diagnosed as embryonic yolk sac tumour. The patient was referred to MINAR for post-operative radiotherapy.
Introduction
Yolk sac tumor (YST) is a rare malignant tumor of germ cells that line the yolk sac of the embryo. These tumors usually grow in gonads while some extra-gonadal counterparts typically target the mediastinum, endometrium, sacrococcygeal areas, cervix and vagina [1]. This neoplasm accounts for 3.5% of all childhood cancers and its usual age of presentation is 15 to 19 [2]. The incidence of malignant yolk sac tumor is less than 1 per million per year while male to female ratio is about 1:2.5 [3].
Gonadal yolk sac tumors that are found in the ovaries or testes usually present as a painless, firm swelling that grows rapidly to the noticeable size. On the other hand extra gonadal yolk sac tumors present as a firm swelling with intermittent pain and fever [4]. Among extra gonadal sites, certain cases of yolk sac tumor have been reported in head and neck area [5].
The exact pathogenesis of YST is still not clear. However, most of the studies propose that these tumors arise from malignant transformation of misplaced primordial germ cells. During the 4-6th week of embryogenesis primordial germ cells migrate along the dorsal mesentery to the genital ridge. Certain germ cells may not complete this journey and retain along the dorsal wall of embryo at areas near the midline [6]. Some extragonadal tumors may arise from totipotential cells that are scattered throughout the body and have the potential for additional growth when suitably stimulated [7].
There are numerous diagnostic modalities which can be used, such as US, CT, magnetic resonance imaging (MRI) and histopathological examination of tumor specimen. Another important diagnostic marker is alpha-fetoprotein (AFP), whose level was found to be elevated in > 90% of yolk sac tumors [4]. Cancer cells secrete human chorionic gonado-protein (HCG) and alpha-fetoprotein (AFP) and their levels are reported to be elevated in these patients [8]. These substances can be used as tumor biomarker for diagnostic and follow up cases.
The best treatment option for YST is surgery for eliminating the primary tumor without severe morbidity [9]. Surgical procedures usually involve the debulking surgery of tumor followed by adjuvant chemotherapy. The national comprehensive cancer network recommend 3-4 cycles of chemotherapy of regimen of BEP (bleomycin, etoposide and cisplatin) [10]. BEP chemotherapeutic treatment is considered to be a gold standard first line protocol in all stages of germ cell tumors [11].
Both gonadal and extragonadal yolk sac tumors exhibit poor prognosis. Because of their rapid spread and metastasis, clinical presentation usually obscures the actual invasion. Minimally invasive surgery, fertility sparing surgery techniques and adjuvant chemotherapy has been proved to have better prognosis [9].
Case Presentation
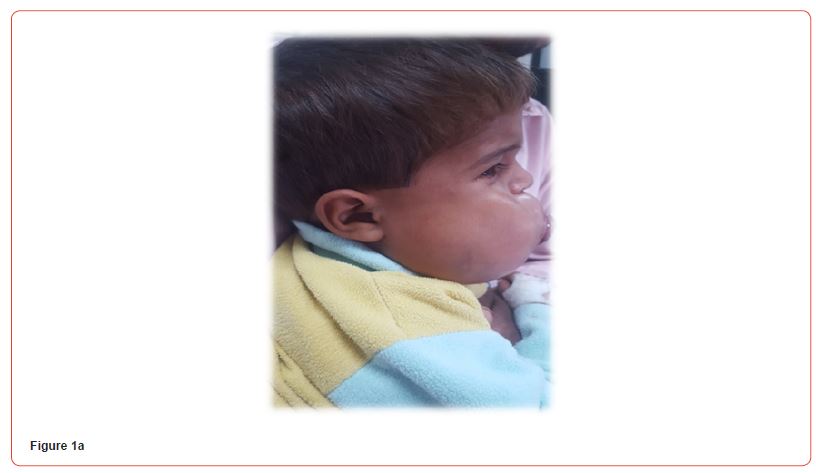
A three years old boy was presented to the Department of Oral and Maxillofcial Surgery, Bakhtawar Amin Dental Hospital Multan with aggressively growing mass with grotesque swelling on right side of the mandible with a history of one and half month only. The parents of the patients noticed a small swelling one and half month back. Initially, they ignored the swelling because it was painless and not causing any discomfort during eating. But the swelling attained a large size by growing aggressively in very short duration with gross facial disfigurement. On clinical examination, the swelling was firm and non tender. Patient’s medical history was non-significant (Figure 1a).
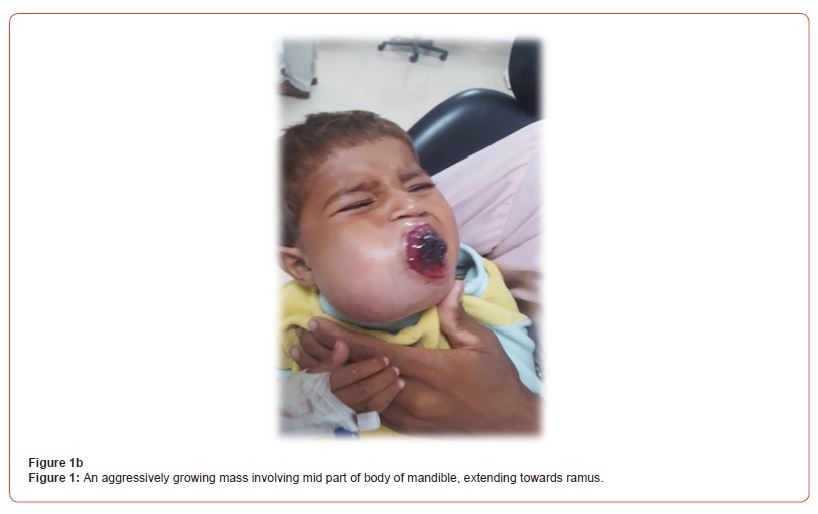
Intraoral examination could not be performed due to limited mouth opening and non-cooperative behavior of the child. The tumour mass was obstructing the oral cavity and a part of tumour was protruding from the mouth opening. Blood clots were visible over the protruding front of the tumour (Figure 1b).
On general physical examination, patients appeared weak, pale with signs of anemia by without any signs of jaundice, clubbing of nails and cyanosis. The pulse rate (85 BPM), respiratory rate (20/ min) and blood pressure (130/80 mmHg) were quite normal in range. There was no abdominal distension or disturbed vision. Radiological and other laboratory investigations were quite normal in range.
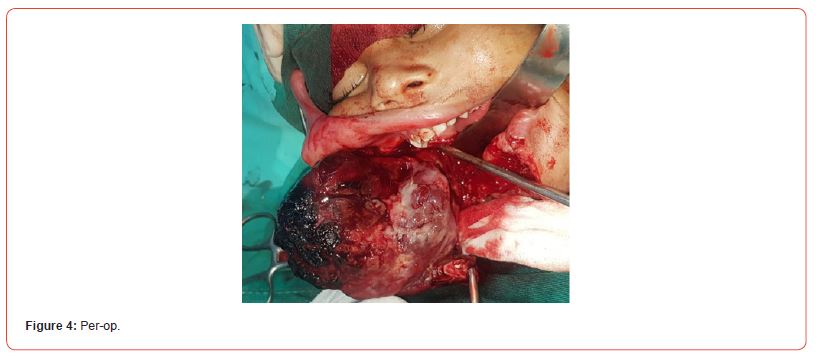
On gross examination the excised specimen size was measured as 7.5x6.5x4. Actual tumour bulk was composed of a large necrotic mass and upon removal of this necrotic area, the remaining tumour bulk was measured as 7.5x3.5x3.5cm.
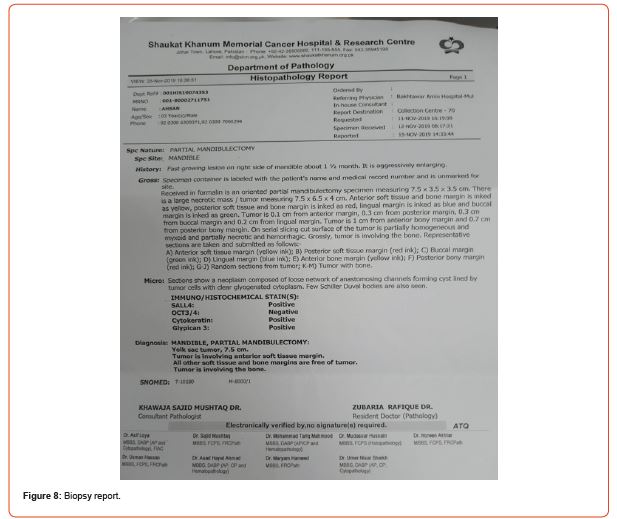
Tumor was 0.1cm from anterior margin, 0.3cm from posterior margin, 0.3cm from buccal margin and 0.2cm from lingual margin. On serial slicing, cut surface of tumor was partially homogenous and myxoid and partially necrotic and hemorrhagic. Grossly tumor is involving the bone. On histopathology, hematoxylin and eosin stained sections showed a neoplasm composed of loose network of anastomosing channels forming cystic cavities lined by tumor cells with clear glycogeneted cytoplasm. Few Schiller Duval bodies were also seen. All the margins of excised mass other than anterior margin were free of tumour cells. On immunohistochemical staining, tumour tissue shows positivity for SALL4, cytokeratins and Glypican-3 and negativity for Oct-3 and Oct-4.
Based on clinical, radiographic, histopathological and immunohistochemical findings, the lesion has been diagnosed as embryonic yolk sac tumour. The patient was referred to MINAR for post-operative radiotherapy.
Discussion
Yolk sac tumors (YSTs) are a type of malignant germ cell tumor that usually grow in the gonads. They are difficult to recognize at other sites outside the gonads, and very few cases have been reported involving the head and neck region (Chen et al. 2017). However, between 10 and 15% of YST occur in the midline structures of the mediastinum, retroperitoneum and sacrococcygeal areas. Certain cases have been reported in other location such as in the pineal region and head and neck [3-5].
In the rare case discussed in the present study the diagnosis was established by histological and immunohistochemical examinations. The major pathologic characteristics of YSTs include a reticular pattern, a solid pattern, a hepatoid pattern with hyaline globules, a festoon pattern, enteric differentiation, Schiller- Duval bodies, the presence of a granulomatous tissue reaction and a polyvesicular vitelline pattern [6, 7]. Schiller-Duval bodies have been reported as a common feature to extragonadal YSTs, as observed in large quantities in a previous study [8]. Typical Schiller-Duval bodies comprise cuboidal or low columnar-shaped tumor cells surrounding the capillaries of a thin-walled sinus [9, 10]. Immunostaining plays very important role in diagnosing this tumour. Staining for alphafetoprotein by immunoperoxidase techniques is usually positive in this tumour [11] (Figures 2-9).






Acknowledgement
None.
Conflict of Interest
None.
References
- Lightfoot MA, Bilgutay AN, Kirsch AJ (2018) A rare case of pediatric vaginal yolk sac tumor. Urology: 119: 137-139.
- Bernstein L, Smith MA, Liu L, Deapen D, Friedman DL (1975) Germ cell, trophoblastic and other gonadal neoplasms. Cancer incidence and survival among children and adolescents: United States SEER Program 125-138.
- Altman RP, Randolph JG, Lilly JR (1974) Sacrococcygeal teratoma: American Academy of Pediatrics surgical section survey-1973. J Pediatr Surg 9(3): 389-398.
- Chen LH, Yip KC, Wu HJ, Yong SB(2019) Yolk sac tumor in an eight-year-old girl: A case report and literature review. Front Pediatr 7: 169.
- Devaney KO, Ferlito A, Rinaldo A (2003) Endodermal sinus tumor (yolk sac tumor) of the temporal bone: an exotic disease for otorhinolaryngologists and head and neck surgeons. Acta Otolaryngol 123(6): 747.
- Jin X, Han C, Sun H (2011) Primary yolk sac tumor in floor of mouth in a child. J Oral Maxillofac Surg 69(7): 1973-1977.
- Brown N (1976) Teratomas and yolk-sac tumours. Journal of clinical pathology, 29(11): 1021.
- Andersson G (2003) Tinnitus loudness matchings in relation to annoyance and grading of severity. Auris Nasus Larynx 30(2): 129-133.
- Guida M, Pignata S, Palumbo AR, Miele G, Marra ML, et al. (2013) Laparoscopic treatment of a Yolk Sac Tumor: case report and literature review. Translational Medicine UniSa 7: 1-5.
- Eddaoualline H, Sami H, Rais H, Belbaraka R, El Omrani A, et al.(2018) Ovarian Yolk sac tumor: a case report and literature review. Clin Case Rep Int 2: 1057.
- Williams S, Blessing JA, Liao SY, Ball H, Hanjani P (1994) Adjuvant therapy of ovarian germ cell tumors with cisplatin, etoposide, and bleomycin: a trial of the Gynecologic Oncology Group. J Clin Oncol 12(4): 701-706.
-
Muhammad Saeed, Muhammad Athar Khan*, Muhammad Kashif, Muhammad Gulzar, Muhammad Shahzad Ansari and Nizam. Embryonic Yolk Sac Tumor of Mandible: A Rare Entity with Clinicopathological Features and Literature Review. On J Dent & Oral Health. 6(5): 2023. OJDOH.MS.ID.000650.
-
Large tumour, Tumor of mandible, Sacrococcygeal areas, Head and neck area, Primordial germ cells, Extragonadal tumors, Yolk sac tumors, Swelling, Oral cavity, Grossly tumor.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






