 Research Article
Research Article
Effect of the Implant Macro Design on Primary Stability: A Randomized Clinical Trial
Joseph Zaarour*, Emile Chrabieh, Stephanie Rameh, Antoine Khoury and Ronald Younes
Department of Oral Surgery, Faculty of Dental Medicine, Saint Joseph University of Beirut, Beirut-Lebanon
Joseph Zaarour, Department of Oral Surgery, Faculty of Dental Medicine, Saint Joseph University of Beirut, Beirut-Lebanon.
Received Date: June 30, 2023; Published Date: July 20, 2023
Abstract
Aim of the study: Comparing the impact of two different implant macro-designs on the primary stability.
Material and methods: Patients received implants in the lower posterior jaw (bone type II and III). Two different macro-design implants were inserted randomly in accordance with a conventional drilling protocol, the first one is the hybrid self-tapping implant: Straumann® bone level BL and the second one is tapered self-tapping implant: Straumann® bone level tapered BLT.
16 implants (3.3 and 4.1 mm diameter, length between 8 and 10mm) of each of the two above-mentioned implants were used. Primary stability assessment of each implant design was carried out by using two methods, recording the maximum insertion torque IT (DTA device) and recording the implant stability quotient ISQ using the resonance frequency analysis RFA (with the Osstell device).
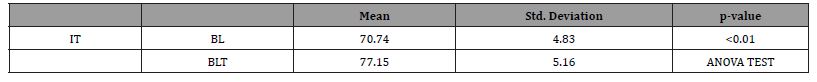
Results: In all bone types, BLT implants showed significantly higher mean insertion torque IT when compared to BL with respectively 46.67±6.85 Ncm and 35.77±6.72 Ncm for (p=0.01 as per the Anova test), and higher mean ISQ with respectively 77.15±5.16 and 70.74±4.83. (p=0.01 as per the Anova test).
Conclusion: In type II and III bone, the tapered self-tapping implant (Straumann® BLT statistically showed better primary stability when compared to hybrid self-tapping implant: Straumann® bone level BL. Within the limitations of the present study, it can be concluded that implant Macro-Design may be considered as a reliable parameter to achieve acceptable primary stability of dental implants in areas with low bone density. In the present study, the two methods used to assess the primary stability of the different macro-designs, torque assessment and the RFA, showed a weak correlation. The macro-geometry is basically made to satisfy the needs in some critical bone situations and in immediate loading protocol.
Keywords:Dental implants; Insertion torque, Primary stability, Implant design, Implant geometry, Implant thread, Resonance frequency analysis
Introduction
Dental implants are the most promising materials currently used for the replacement of lost teeth. They have revolutionized oral rehabilitation by managing partially or fully edentulous patients, achieving success rates beyond 90% on a long term basis [1].
Therefore, immediate implantation and loading procedures have become more and more common in practitioners’ daily clinical practice. The major parameter to successfully implement an immediate loading procedure is adequate primary stability within strict precautions; thus, implant stability at the time of surgery is crucial for the long-term success of dental implants [2]. Primary implant stability can be defined as a function of local bone quality and quantity, the geometry of an implant, the placement and surgical technique used, as well as the precise fit in the bone. Thus, primary implant stability is considered a significant parameter in achieving osseointegration, and the orchestration of the already mentioned elements is crucial for the long-term success of the implant [1].
As a result, several studies were conducted to establish clinical guidelines and assure an optimized high insertion torque, while still taking into consideration the key role of implant design. Design features of implant include: Macro-design and Micro-design features. Macro-design features include thread pitch, geometry, depth, width, and design and implant crestal module, while microdesign essentially refers to surface morphology and coatings [3].
Macro-design features focus on the relationship between osseointegration and mechanical features of implant design engineering, allowing the practitioner to decide which implant to select depending on different clinical situations. Meanwhile, microdesign features include the analysis of the biological aspect of implant design and focus on host response patterns and implant survival [4].
This article aims to evaluate the influence of macro-geometry on primary stability at time 0, and thus, prove the hypothesis that the new Straumann Bone Level Tapered (BLT) implant is more suitable than Straumann Bone Level (BL) in terms of primary stability.
Materials and Methods
The present study is a randomized controlled clinical trial. 16 patients were included and each received 2 to 4 implants in the lower posterior jaw, where two types of Straumann® implants (BL or BLT) were placed with a conventional drilling protocol using a guided surgical kit and a 3D printed surgical guide.
The Bone Level BL Implant has a hybrid self-tapping macro design mainly cylindrical, non-fluted, rounded apical tip, with a reverse buttress type of threads and 0.8 pitch; while the Bone Level Tapered BLT Implant has a hybrid self-taping tapered macrodesign at its lower half, a bowl cutting flute at the lower part, helicoidal apical tip with a reverse buttress type of threads and 0.8 pitch. Both of the implant macro designs have a single thread. (See Figure 1)
In Total 32 Straumann® implants were placed: 16 BL and 16 BLT. Implant diameters varied between 3.3 and 4.1, and implant length between 8 and 10mm.
Bone quality was assessed by the main investigator following the classification of Lekholm and Zarb 1985 [5]; in the posterior mandibles where implants were placed, bone types II and III were reported.

Patient recruitment
The patients were treated at Saint Joseph University dental clinics. They were recruited based on the following inclusion and
exclusion criteria:
Inclusion criteria:
-Patients aged over 18 years old.
-Edentulous sites in posterior mandibles with no bone grafts.
-Crest width ≥5.5mm and residual bone height above alveolar nerve canal ≥10mm.
-Provision of informed consent.
-Good oral hygiene and no signs of active periodontal disease.
-No compromising medical status.
-<10 cigarettes smoked per day.
Exclusion criteria
-Compromising medical status, head and neck irradiation, heavy smoker.
-Earlier bone grafting in the study area.
-Acute periodontitis or local infection or deficiency.
-Severe Bruxism.
An Institutional Review Board (IRB) approval was sought from the Committee for the Protection of Human Subjects (CPHS).
A consent document was duly signed by each patient. The information presented in the informed consent process was as specific as possible.
Surgical procedure
Participants were randomly allocated to receive one of each type of the following implants: hybrid self-tapping implant: Straumann® bone level BL Roxolid SLA and tapered self-tapping implant: Straumann® bone level tapered BLT Roxolid SLA (Straumann® Implant Co., Ltd, Straumann Holding -Basel Switzerland T).
All patients were treated under local anesthesia (Articaine 40mg/0.01mg epinephrine). Incisions were performed as required according to each situation’s specificity. A full thickness flap was raised if needed.
A conventional drilling protocol was applied through a printed surgical guide and implant placement was performed in a fully digital guided protocol. Implant sites were chosen following bone morphology on a pre-operative CBCT radiographic cuts.
Assessment methods
Two recording methods were used to assess primary stability: maximum insertion torque IT and implant stability quotient ISQ. Measurements were performed at time 0 only as this article aims to evaluate the influence of macro-geometry on initial primary stability without studying the effect of primary stability on implant osteointegration.
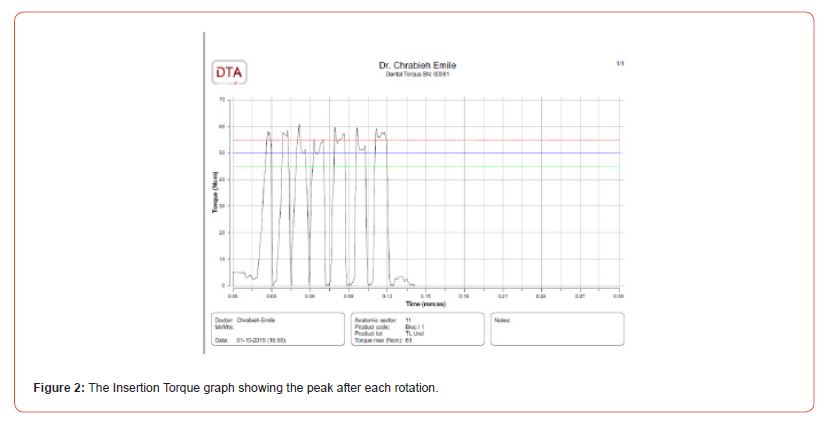
Recording the maximum insertion torque IT (DTA device):
Maximum insertion torque (IT) was assessed by means of a DTA device (by studio AIP Srl). Implant insertion was performed by a ratchet linked to a transducer which is connected to a computer via Bluetooth. A graph shows, on a DT1 2.2 software, IT variation with each rotation, the highest value will be displayed as the maximum insertion torque in Ncm., (Figure 2).
It is important to emphasize that the guidance sleeve did not affect IT values, particularly because there was no friction with implant carrier during IT recording.
Recording implant stability quotient ISQ:
Using the resonance frequency analysis RFA (with the Osstell device). Each implant was measured, with a “resonance frequency analysis” system RFA, in “implant stability quotient” ISQ unit using the OsstellTM ISQ device (Osstell, Göteborg, Sweden).
OsstellTM measurements were displayed as ISQ from 1 to 100, where 100 signifies the highest implant stability. The SmartPeg was screwed to each implant and tightened to approximately 5 Ncm following the OsstellTM Guidelines. The transducer probe was oriented at the small magnet on top of the SmartPeg at a distance of 2 to 3mm and held stable during the pulsing time until the instrument beeped and displayed the ISQ value. If two ISQ values were displayed simultaneously, their mean value was recorded. Measurements were taken twice in two perpendicular directions (buccal and Mesial). The mean of all measurements was rounded to the nearest whole number and was regarded as representative of the overall ISQ value.
Statistical analysis
The statistical analyses were performed using a software program (SPSS for Windows version 17.0, USA). Statistical significance of the differences between the groups was determined by the one-factor factorial analysis of variance (ANOVA) or the t-test. The alpha error was set at 0.05.
Values were expressed as means ± standard deviation. Implant design (BL or BLT) was compared with the primary stability values of resonance frequency (ISQ) and insertion torque (Ncm), in the mandible. Normality was checked using the ShapiroWilk test. As the distribution of data was not normal, the Mann-Whitney test was applied. This test uses median values rather than means to perform comparative analysis of quantitative and qualitative variables.
Results
In all bone types combined, BLT implants showed significantly higher mean insertion torque when compared to BL and higher mean IS.
Results Data for the 32 implants tested in the study are expressed in the tables 1 and 2.
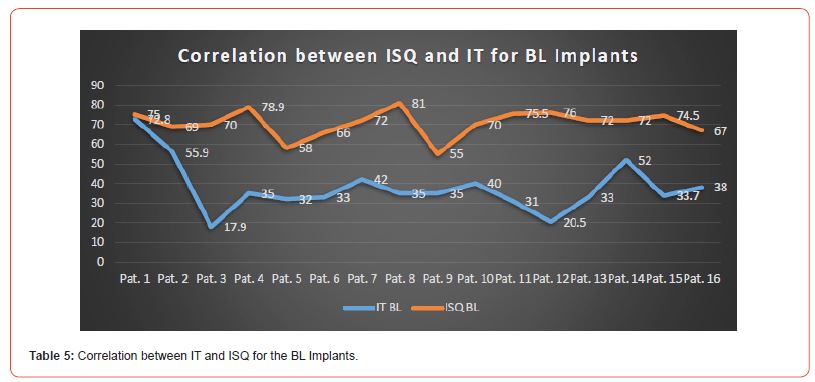
ISQ values were recorded for all implants at time 0, they ranged between 55 and 81 for BL implants and between 65 and 88 for BLT implants.
IT values varied between 17.9 and 72.8 Ncm for BL implants and between 22 and 105 Ncm for BLT implants.
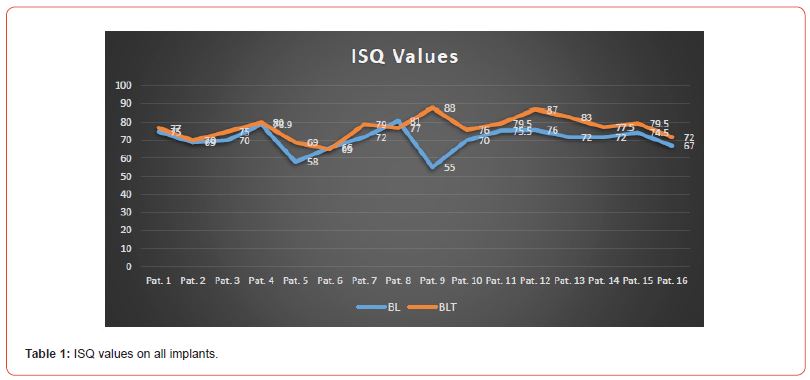
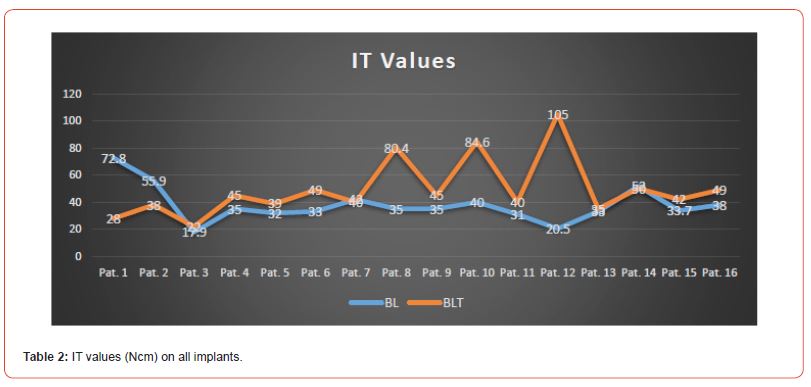
In all bone types combined, BLT implants showed significantly higher mean insertion torque when compared to BL with values of 46.67±6.85 Ncm and 35.77±6.72 Ncm respectively (p=0.01 as per the Anova test). (Table 3 and 4), and higher mean ISQ with respectively 77.15±5.16 and 70.74±4.83. (p=0.01 as per the Anova test).
These higher values for the BLT were very important in bone type II and III. The new implant macro-design, the tapered selftapping implant (Straumann® BLT), showed a better primary stability in all types of bone.
Table 1:IT values (Ncm) on all bone type.
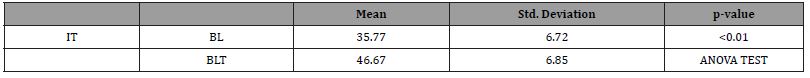
Table 2:ISQ values (Ncm) on all bone types.
Correlation between the two methods of primary stability assessment is revealed to be weak, as expressed in Table 5 and Table 6 for each type of implant design. In the case of BL implants, ISQ values varied between 55 and 81, yet IT values ranged from 17.9 to 72.8 Ncm. For a same IT value of 35 Ncm, ISQ reached its lowest value of 55 (Pat. 9) as well as its highest value of 81 (Pat. 8).
Similarly for BLT implants, as ISQ values varied between 65 and 88, IT values ranged from 22 to 105 Ncm. It is thus important to emphasize that the highest ISQ value of 88 (Pat. 10) did not correspond to the highest IT value of 105 (Pat. 12); instead, it coincided with an average IT value of 45 Ncm. Furthermore, the lowest ISQ value of 65 (Pat. 6) did not correspond with the lowest IT value of 22 (Pat. 3); it instead coincided with an average IT value of 49 Ncm.

Discussion
The current study was conducted in a way to minimize variables, and thus, reduce the bias by concentrating the parameters around the macro-design of different implants.
BLT implants showed significantly higher mean insertion torque when compared to BL implants and higher mean ISQ. Similar results were reported in different bone bloc types in an ex vivo study on bovine ribs [6].
Considering many studies evaluating the effect of the design on primary stability, the hybrid tapered self-tapping implant was expected to achieve better values for the two measurements.
The results of the present study are in accordance with a previous one [7] performed by Chrabieh in 2017 using an ex vivo model congruent with our expectations. This consequently leads the authors of the present study to believe that in clinical use, a hybrid self-tapping implant could also accomplish sufficient primary stability for stable osseointegration with long-term implant success.
Greater these parameters (ISQ and IT) are, the higher primary stability is expected to be. This will be one of the fundamental criteria for the development of successful osseointegration [7]. In the literature, no minimum recommendation for Insertion Torque values in early and late loading protocols is reported (6); while for an immediate restoration/loading (type 1A), an IT of 25 -> 40 N/ cm and/or ISQ>70 is required, as stated in the systematic review performed by the group of Gallucci in 2018 (6th ITI Conference Statement held in Amsterdam) [8].
The efficacy of root formed implants over parallel-sided implants placed in compromised bone sites has been demonstrated [8]. The new designs, which include smooth thread shoulder, can significantly reduce the stress concentration at implant neck.
Studies showed that maximum effective stress decreased as screw pitch decreased and implant length increased [9]. Interestingly, some considered 0.8mm as the optimal thread pitch for achieving primary stability [10].
When primary stability is a concern, as is the case in cancellous bone, increasing implant surface area by using implants with smaller pitch might be beneficial [11].
According to Chun HJ, et al. the most favorable configuration in terms of implant stability appeared to be the single-threaded configuration [12]. In addition, greater thread depth may be an advantage in areas of softer bone and higher occlusal force because of the higher functional surface area in contact with surrounding bone [13]. Additionally, the use of cutting flutes increases the selftapping ability of the implant tip [14]. The bowl-fluted design has the least flute space to store the squeezed bone chips, so both insertion torque and bending strength were significantly higher [15]. Overall, the conical implant with bowl flutes is the optimal design, with a lower resistance to initial insertion and higher stability, for final instrumentation [15].
It is also important to highlight that, as previous studies show [16], no significant difference in primary stability was found between implants of lengths <11mm and diameters between narrow and regular platform. Thus, implants with 3.3 and 4.1mm in diameter, 8 and 10mm long, equally distributed between both groups of trial, present no direct influence on IT, nor on ISQ.
The ISQ parameter assessed with the The Osstell™ Mentor (Integration Diagnostic Ltd., Goteborg, Sweden) using Resonance Frequency Analysis RFA provides information about the stiffness of the implant-bone junction, while insertion torque value ITV is a mechanical parameter that measures cutting resistance.
The RFA analysis is intended to be used as a continuous monitoring during the osseo-integration process and never as a punctual assessment.
According to these positions, the weak point of this ITV/ISQ relationship rests on the fact that these two methods are completely independent and incomparable in measuring primary implant stability, suggesting that they should be calculated independently because a high torque does not mean high ISQ, and vice versa [17].
In an Ex-Vivo Study, Chrabieh, et al. [6] cited that “The two methods used to assess the primary stability of the different implant macro-designs, the maximum insertion torque and the resonance frequency analysis, showed a weak correlation” [6]. Subsequently, in our current study, a mild correlation between the two methods of assessment RFA and ITV was revealed. For instance, a very high value of RFA could show an implant which is still rotating, ITV < 10Ncm, embedded in a very stiff cortical bone, and on the contrary, a high insertion torque ITV might show a weak RFA in cancellous bone at day 0.
Additionally, in the work of Dos Santos, et al. (2011) [18], the corresponding analysis for ISQ showed no statistically significant difference between conical and cylindrical implants. Those results corroborate data presented in the literature [19].
On the other hand, the results conflict with previous studies that found significant differences between dense and soft bone for RFA [20]. Moreover, according to Meredith and coll. 1998, the use of RFA measurement seems to be appropriate for assessing reliable data on implant stability because variables during the standardized measurements are kept to a minimum.
Contradictions have been reported on the clinical use of the RFA methods of measurements. IT values were more highly correlated with bone volume fraction (BV/TV) than ISQ values. IT values were reportedly also more sensitive in terms of revealing biomechanical properties at the bone-implant interface in comparison with ISQ [21]. Therefore, Makary and coll. in 2011 showed that increasing peak IT values correlated with increasing bone volume.
Histomorphometric evaluation of the bone-implant contact (BIC) could theoretically provide information on implant anchorage, yet this approach has only been used in animal studies.
RFA is a measure of three distinct variables:
1) Stiffness of the proper implant,
2) Rigidity of the implant-tissue interface, and
3) Stiffness of the surrounding bone [22].
That being said, Zhou et al. together with Scarano et al. demonstrated that the BIC was correlated with ISQ values in animals and in retrieved human implants, respectively [23, 24].
Cortical bone seems to have more of a remarkable influence on RFA values variation, since it measures the stiffness of the surrounding bone which does not necessarily reflect a high insertion torque or high primary stability [6].
Initially, bone quality has been investigated with variations in the damping factor, thickness of the cortical bone, and bone stiffness [25]. Whereas, the damping factor had no effect on implant stability, regardless of the level of osseointegration, strong correlation between cortical thickness and implant stability has been found. In different clinical studies, bone type was found to affect primary implant stability as determined by RFA, [26, 27] whereas after healing, bone type exerted only a minor influence.
Bischof M, et al. (2004) [1] revealed that increasing levels of bone loss led to a reduction in implant stability; this is consistent with the results of an in vitro study on RFA measurements of implants with increasing levels of bone loss [1].
The initial implant insertion torque values can be considered as an indicator of a good primary stability. Implant stiffness means a greater bone-to-implant contact percentage, explaining the better prognosis. The design of the implants used also might have helped in obtaining good primary stability because of the unique features [1].
More recently, Miyamoto, et al. [28] reported a significant correlation between the ISQ and the thickness of cortical bone. In addition Nkenke, et al. in a human cadaver study, found that resonance frequency analysis did correlate with the surface of bone-to-implant contact [29]. Ostman, et al. (2006) [27] found a significant correlation between bone density and ISQ. Overall, there is a substantial body of evidence in support of the correlation between ISQ and bone density [30, 19, 16].
The real value in taking multiple ISQ measurements of an implant over time is being able to track the dynamic changes occurring around an implant after placement and after restoration. This information can be used to aid in clinical decision-making such as whether or not to immediately load an implant or when to transition from a provisional to a definitive restoration. After the transient decrease in implant stability, a healthy implant with an initially low ISQ value will tend to display a marked increase in ISQ over time as osseointegration increases. A healthy implant with an initially high ISQ will tend to experience either a slight increase in ISQ or persistence of the initial ISQ value [20, 31, 32, 1]. Lower or decreasing ISQ values may be a sign of developing instability, in a late healing stages.
On the whole, the body of available literature supports the use of RFA as a clinical tool in implant dentistry capable of providing a non-invasive, quantitative assessment of the stiffness of the boneimplant interface (i.e., bone support). However, it is important to understand its limitations. The real value in RFA lies in having multiple (minimum of two) measurements that can be compared over time [18]. A single reading at any time-point, whether it is at the time of implant placement, the time of the osseointegration, or after the implant is restored, is of little value and can potentially be misleading. ISQ measurements cannot be standardized between different implants but rather for the same implant over an observation period [33].
Also, this measurement should not be used in isolation but rather as a supplement to other methods of implant assessment.
Numerous studies confirm that insertion torque undoubtedly plays an important role in primary stability and successful osseointegration of implants [9]. In addition , no correlation between insertion torques and implant failure above 35 Ncm [32].
Moreover, Makary, et al. [34] found that high IT does not seem to alter the osseointegration process. Results from their meta-analysis on the effect of high implant insertion torque value on marginal bone resorption also show no statistically significant differences between high and conventional torque values in terms of effects on peri-implant bone loss.
A more recent study demonstrates no negative impact on the biological process of osseointegration in implants inserted with high torque (50 Ncm) with respect to the low torque group (10 Ncm) [35].
In contrast, other studies have suggested that high insertion torque values produce strong compressive forces onto the peri-implant bone, an altered mechanical strain environment and the potential induction of deleterious effects on the local microcirculation and bone cellular responses, which may lead to bone necrosis and ultimately to a delayed or compromised implant osseointegration [35].
Different implant macro-designs show improved results in primary stability without any evident bone loss around the implant, while for the same values of implant stability, other systems with specific macro-design show a total loss of bone mass [36]. This evidence confirms the hypothesis that there is a difference in primary stability with different macro-designs, but the goal is to show when and where to use these implants in a safe manner and adequate indication.
The literature shows a tremendous number of publications regarding immediate loading procedures. Data from Gallucci and colleagues deduced from the 5th ITI Consensus [37] Conference showed the high predictability of early loading protocols when compared to conventional healing times.
Also, the same data showed no differences regarding implant survival rates, marginal bone loss, and aesthetic results. These inferences also provided clinical recommendations for implant loading protocols in the case of single implants in partially edentulous patients and fixed prostheses in complete edentulous cases [37].
In the case of immediate loading of single-implant crowns, the recommendations provide an ITV>35 to 45Ncm and ISQ>80 to 85 [38].
While in full-arch rehabilitation of totally edentulous patients, an ITV>30 N/cm, ISQ>60, and minimal implant length>10mm are recommended [38, 39].
Conclusion
In type II and III bone, the tapered self-tapping implant Straumann® BLT statistically showed better primary stability when compared to hybrid self-tapping implant: Straumann® bone level BL.
Within the limitations of the present study, it can be concluded that BLT implant might be considered a reliable parameter to achieve acceptable dental implant primary stability in areas with low bone density.
In the present study, the two methods used to assess the primary stability of the different macro-designs, torque assessment and resonance frequency analysis RFA, showed a weak correlation.
Funding
This research was funded by STRAUMANN International Headquarters Holding AG Peter Merian-Weg 12 4002 Basel, Switzerland.
Acknowledgement
None.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Nedir R, Bischof M, Szmukler Moncler S, Bernard JP, Samson J (2004) Predicting osseointegration by means of implant primary stability. Clin Oral Implants Res 15: 520-528.
- Bayarchimeg, Dorjpalam (2013) Evaluation of the correlation between insertion torque and primary stability of dental implants using a block bone test. J Periodontal Implant Sci 43: 30-36.
- Marcio Vivan Cardoso, Katleen Vandamme (2015) Dental Implant Macro-Design Features Can Impact the Dynamics of Osseointegratio. Clin Implant Dent Relat Res 17(4): 639-645 .
- Gurzawska K (2012) Nanocoating of titanium implant surfaces with organic molecules Polysaccharides including glycosaminoglycans. J Biomed Nanotechnol 8(6): 1012-1024.
- Lekholm U, Zarb GA (1985) Patient selection and preparation. Tissue integrated prostheses: osseointegration in clinical dentistry. Quintessence Publishing Company, Chicago, USA, pp. 199-209.
- Chrabieh Emile (2017) Effect of the implant macro-design on the primary stability, review of the literature and an ex-vivo model study. JAJD 8.
- Takeshi Toyoshima (2011) Primary Stability of a Hybrid Self‐Tapping Implant Compared to a Cylindrical Non‐Self‐Tapping Implant with Respect to Drilling Protocols in an Ex Vivo Model. Clin Implant Dent Relat Res 13(1): 71-78.
- Gallucci GO, Hamilton A, Zhou W, Buser D, Chen S (2018) Implant placement and loading protocols in partially edentulous patients: A systematic review. Clin Oral Impl Res 29(16) :106-134.
- Chun HJ, Cheong SY, Han JH, Heo SJ, Chung JP, et al. (2002) Evaluation of design parameters of osseointegrated dental implants using finite element analysis. J Oral Rehabil 29: 565-574.
- Kong L, Liu BL, Hu KJ, Li DH, Song YL, et al. )2006) Optimized thread pitch design and stress analysis of the cylinder screwed dental implant. Hua Xi Kou Qiang Yi Xue Za Zhi 2(24): 509-512, 515.
- Ester Orsini, Gianluca Giavaresi, Alessandra Trirè, Vittoria Ottani, Stefano Salgarello (2012) Dental Implant Thread Pitch and Its Influence on the Osseointegration Process: An In Vivo Comparison Study. Int J Oral Maxillofac Implants 27: 383-392.
- Ma P, Liu HC, Li DH, Lin S, Shi Z, et al. (2007) Influence of helix angle and density on primary stability of immediately loaded dental implants: Three-dimensional finite element analysis. Zhonghua Kou Qiang Yi Xue Za Zhi 42: 618-621.
- Misch CE, Strong T, Bidez MW (2008) Scientific rationale for dental implant design. Contemporary Implant Dentistry (3rd), St Louis: Mosby, pp. 200-229.
- O’Sullivan D, Sennerby L, Meredith N (2000) Measurements comparing the initial stability of five designs of dental implants. Clin Implant Dent Relat Res 2: 85-92.
- Shu Wei Wu, Chia Ching Lee, Ping Yuen Fu, Shang Chih Lin (2011) The effects of flute shape and thread profile on the insertion torque and primary stability of dental implants. Med Eng Phys.
- Ostman PO, Hellman M, Wendelhag I, Sennerby L (2006) Resonance frequency analysis measurements of implants at placement surgery. Int J Prosthodont 19(1): 77-83.
- FS Lages, DW Douglas-de Oliveira, F O Costa (2018) Relationship between implant stability measurements obtained by insertion torque and resonance frequency analysis: a systematic review. Clinical Implant Dentistry and Related Research 20(1): 26-33.
- Dos Santos M, Elias C, Lima J (2011) The Effects of Superficial Roughness and Design on the Primary Stability of Dental Implants. Clin Implant Dent Relat Res 13(3): 215-223.
- Huang HM, Chiu CL, Yeh CY, Lee SY (2003) Factor influencing the resonance frequency of dental implants. J Oral Maxillofac Surg 61: 1184-1188.
- Friberg B, Sennerby L, Meredith N, Lekholm U (1999) Comparison between cutting torque and resonance frequency measurements of maxillary implants. A 20-month clinical study. Int J Oral Maxillofac Surg 28: 297-303.
- Akkocaoglu M, Uysal S, Tekdemir I, Akca K, Cehreli MC (2005) Implant design and intraosseous stability of immediately placed implants a human cadaver study. Clin Oral Implants Res 16: 202-209.
- L Sennerby, N Meredith (2008) Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontology 2000 47(1): 51-66.
- Y Zhou, T Jiang, M Qian (2008) Roles of bone scintigraphy and resonance frequency analysis in evaluating osseointegration of endosseous implant. Biomaterials 29(4): 461-474.
- A Scarano, M Degidi, G Iezzi, G Petrone, A Piattelli (2006) Correlation between implant stability quotient and boneimplant contact: a retrospective histological and histomorphometrical study of seven titanium implants retrieved from humans. Clin Implant Dent Relat Res 8(4): 218-222.
- Steigenga J, Al-Shammari K, Misch C, Nociti FH, Wang HL (2004) Effects of implant thread geometry on percentage of osseointegration and resistance to reverse torque in the tibia of rabbits. J Periodontol 75: 1233-1241.
- Mark Bisch, Rabah Nedir, Serge Szmukler Moncler, Jean‐Pierre Bernard, Jacky Samson (2004) Implant stability measurement of delayed and immediately loaded implants during healing 15(5): 529-539.
- Ostman PO, Hellman M, Wendelhag I, Sennerby L (2006) Resonance frequency analysis measurements of implants at placement surgery. Int J Prosthodont 19(1): 77-78.
- Miyamoto I, Tsuboi Y, Wada E, Suwa H, Iizuka T (2005) Influence of cortical bone thickness and implant length on implant stability at the time of surgery: Clinical, prospective, biomechanical, and imaging study. Bone 37: 776-780.
- Nkenke E, Fenner M (2006) Immediate loading of implants and implant success. Clin Oral Implants Res 17: 19-34.
- Mariana Marquezan (2001) Does bone mineral density influence the primary stability of dental implants? A systematic review. Clinical Oral research 23.
- Barewal, Reva M, (2003) Resonance Frequency Measurement of Implant Stability In Vivo on Implants with a Sandblasted and Acid-Etched Surface. Int J Oral Maxillofac Implants 18: 641-651.
- Rizkallah Nadia, Fischer Scott, Kraut Richard A (2013) Correlation Between Insertion Torque and Survival Rates in Immediately Loaded Implants in the Maxilla: A Retrospective Study. Implant Dentistry 22: 250-254.
- Makary C , Rebaudi A, Sammartino G, Naaman N (2012) Implant primary stability determined by resonance frequency analysis: Correlation with insertion torque, histologic bone volume, and torsional stability at 6 weeks. Implant Dent 21: 474-480.
- Makary C, Rebaudi A, Sammartino G, Naaman N (2012) Implant Primary Stability Determined by Resonance Frequency Analysis: Correlation With Insertion Torque, Histologic Bone Volume, and Torsional Stability at 6 Weeks. Implant Dent 21(6): 474-490.
- Duyck J, Roesems R, Cardoso MV (2015) Effect of insertion torque on titanium implant osseointegration: An animal experimental study. Clin Oral Implants Res 26: 191-196.
- P Papaspyridakos, CJ Chen, SK Chuang, HP Weber (2014) Implant loading protocols for edentulous patients with fixed prostheses: a systematic review and metaanalysis. The International Journal of Oral & Maxillofacial Implants 29: 256-270.
- GO Gallucci, GI Benic, S E Eckert (2013) Consensus statements and clinical recommendations for implant loading protocols. Int J Oral Maxillofac Implants 29: 287-290.
- GI Benic, J Mir Mari, C Hammerle (2014) Loading protocols for single-implant crowns: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 29: 222-238.
- Amilcar C Freitas Júnior, Erika O Almeida, Estevam A Bonfante, Nelson R F A Silva, Paulo G Coelho (2010) Reliability and failure modes of internal conical dental implant connections. Clin Oral Implants Res 24: :197-202.
-
Joseph Zaarour*, Emile Chrabieh, Stephanie Rameh, Antoine Khoury and Ronald Younes. Effect of the Implant Macro Design on Primary Stability: A Randomized Clinical Trial. On J Dent & Oral Health. 7(1): 2023. OJDOH.MS.ID.000655.
-
Implants, Lost teeth, Dental implants, Biological aspect, Surgical guide, Implant stability quotient, BLT implants, Osseointegration, Healing.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






