 Case Report
Case Report
Clinicopathologic Correlation: Pericoronal Unilocular Radiolucency in the Posterior Mandible
Emily Li1*, James J Closmann2, Oliver H Chang3 and Henry H Rowshan4
1Doctoral Candidate, University of Colorado School of Dental Medicine, Aurora, CO, USA
2Associate Professor of Surgical Dentistry, University of Colorado School of Dental Medicine, Aurora, CO, USA
3Anatomic Pathologist/Dermatopathologist, VA Puget Sound Health Care System, Seattle, WA, USA
4Private practice oral surgeon, The Center for Oral and Maxillofacial Surgery & Implantology, Bellevue, WA, USA
Emily Li, Doctoral Candidate, University of Colorado School of Dental Medicine, Aurora, CO, USA.
Received Date: June 08, 2022; Published Date: July 01, 2022
Abstract
This paper presents the case of a 15-year-old African-American female who presented with a unilocular radiolucency in the posterior mandible. A history of clinical presentation, differential diagnosis, histologic diagnosis, and the surgical procedure are reported. This is followed by a discussion of the recurrence rate of the lesion as well as its surgical management with topical adjuncts.
Clinical Presentation
A 15-year-old African American female was referred to an oral and maxillofacial clinic for evaluation of a radiolucent lesion in the right posterior mandible. The lesion was discovered on a routine panoramic radiograph by her pediatric dentist. The patient and her mother deny a history of fevers, pain, purulence, or discharge from the location of the lesion. There was neither evidence of a family history significant for similar lesions nor nevoid basal cell carcinoma syndrome (NBCCS). The patient presented with a non-contributory health history, no medications, no known drug allergies, and regular and recent menstruation. Patient denied the use of alcohol, tobacco, or recreational drugs.
Upon examination, no asymmetry or expansion of the right posterior mandible was detected. There was no displacement of any erupted mandibular teeth, and no exudate was expressed on palpation. The patient’s occlusion was stable and reproducible with a normal range of motion in the temporomandibular joint (TMJ). The trigeminal nerve did not show any deficiencies, and no cervical lymphadenopathy or palpable masses detected.
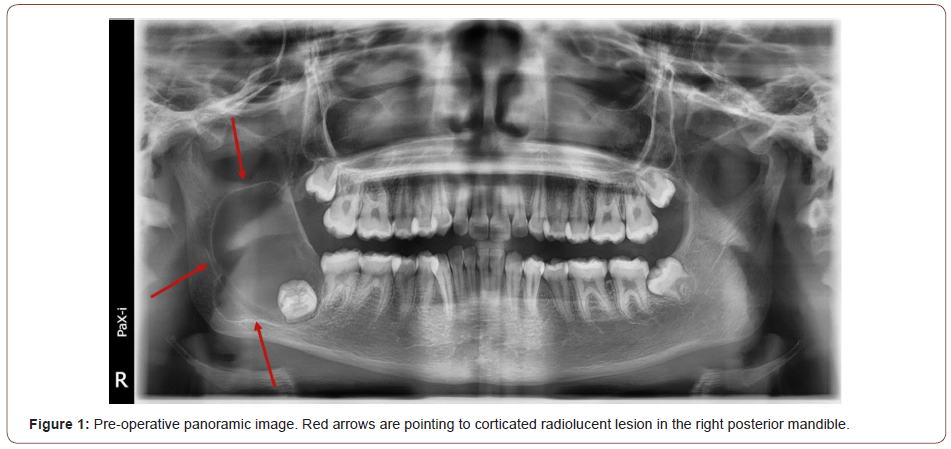
The panoramic radiograph showed a unilocular lesion with well-defined, corticated borders pericoronal to impacted tooth #32. The lesion extended up the right mandibular ramus in a superior and posterior direction, with some displacement of the inferior alveolar canal (Figure 1-pre-op panoramic with red arrows pointing to corticated radiolucent lesion). A CT scan could have more precisely determined the borders of the lesions, but one was not obtained due to the first step of treatment being the same regardless of the findings (i.e. biopsy).
From the location and presentation of the mandibular lesion, a differential diagnosis was derived to include odontogenic keratocyst (OKC), dentigerous cyst, and unicystic ameloblastoma.
Methods
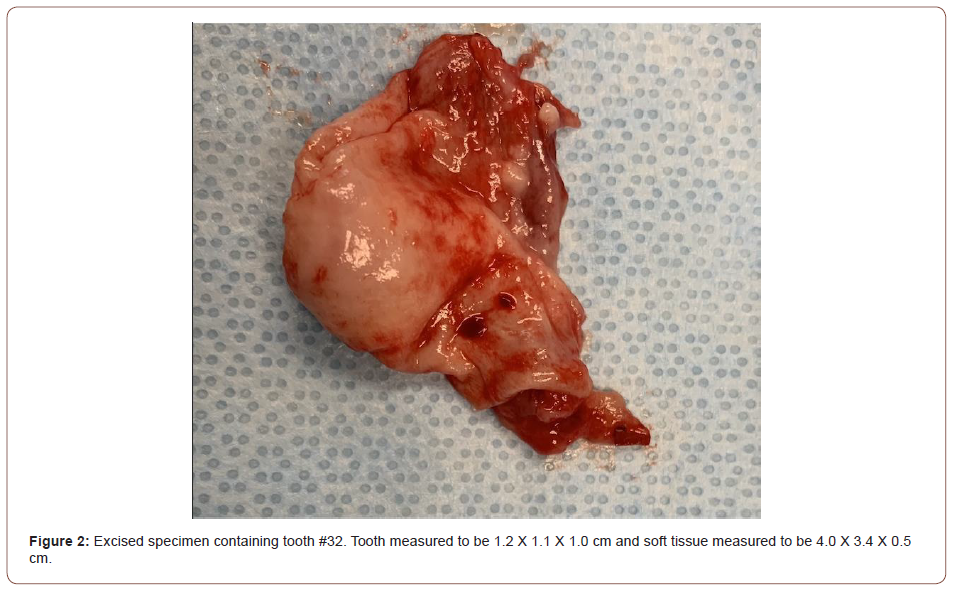
The patient was sedated in the outpatient clinic using intravenous anesthesia. Impacted and malposed teeth #s 1, 16, and 17 were extracted. In the area of #32, a mucoperiosteal flap was reflected and extended up to the middle of the right mandibular ramus and the buccal bone was removed with a round bur. Following an aspiration negative for red blood and an abundance of keratin-like discharge in the surgical field, the lesion was carefully dissected from surrounding bone and removed in one piece (with tooth #32) with an Ellis clamp (Figure 2-excised specimen). A preliminary surgical diagnosis of OKC was made and the specimen was submitted for histologic examination.
Histologic Findings
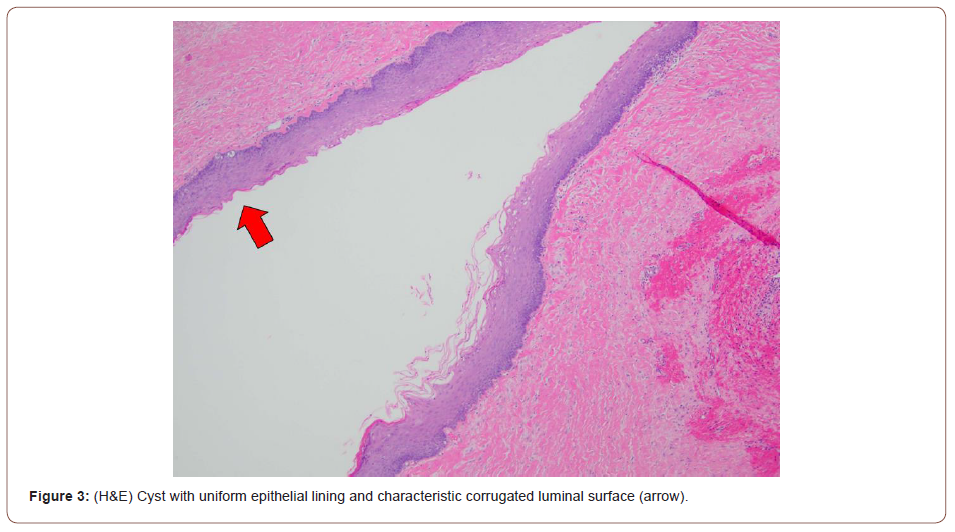
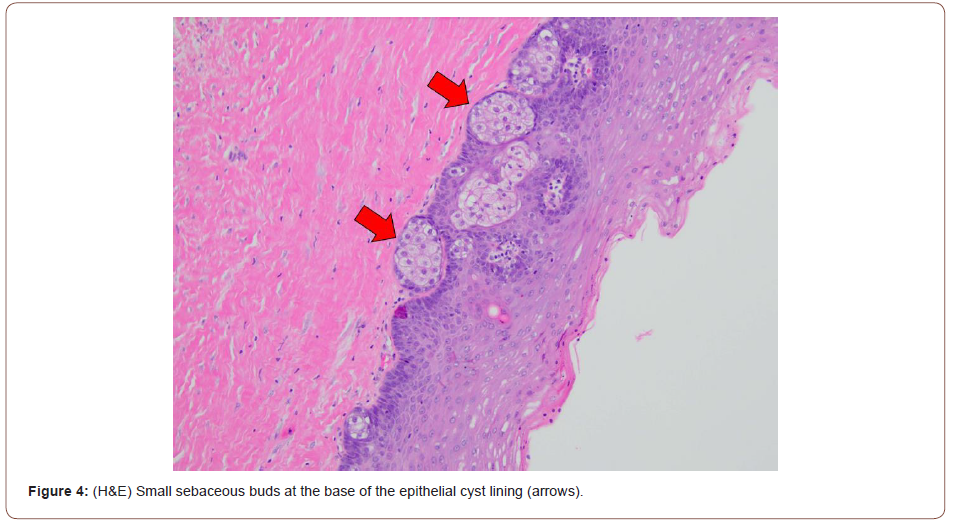
Routine H&E-stained sections contain a cyst with uniform epithelial lining without well-developed rete ridges and a corrugated keratinized luminal surface. Small budding sebaceous glands comprising mature sebocytes are present at the base of the cyst lining. The background tissue is fibrotic with scattered mild inflammation and hemorrhage. The overall findings are consistent with odontogenic keratocyst with sebaceous differentiation.
Figure 3 - (H&E) Cyst with uniform epithelial lining and characteristic corrugated luminal surface (arrow).
Figure 4 - (H&E) Small sebaceous buds at the base of the epithelial cyst lining (arrows).
Post-Operative Management, Port Removal, and 5-FU Treatment
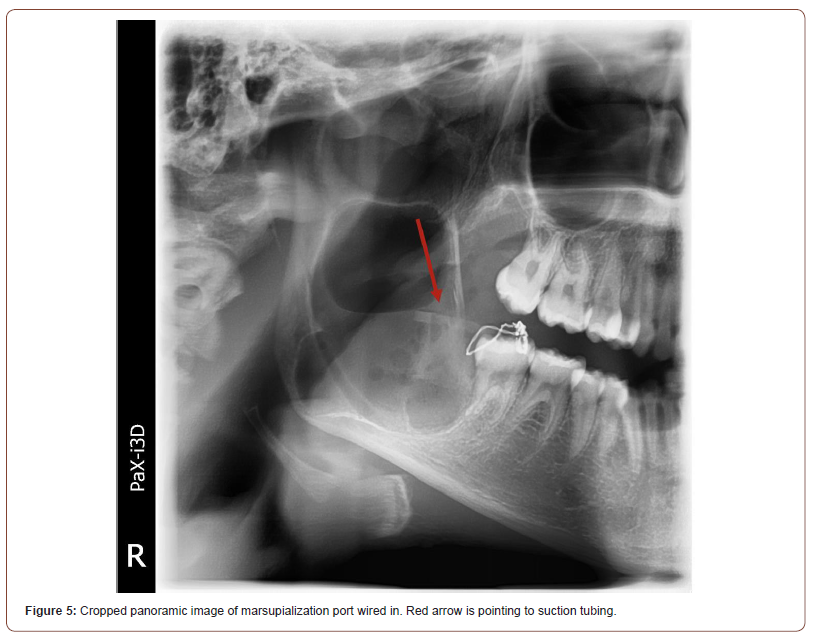
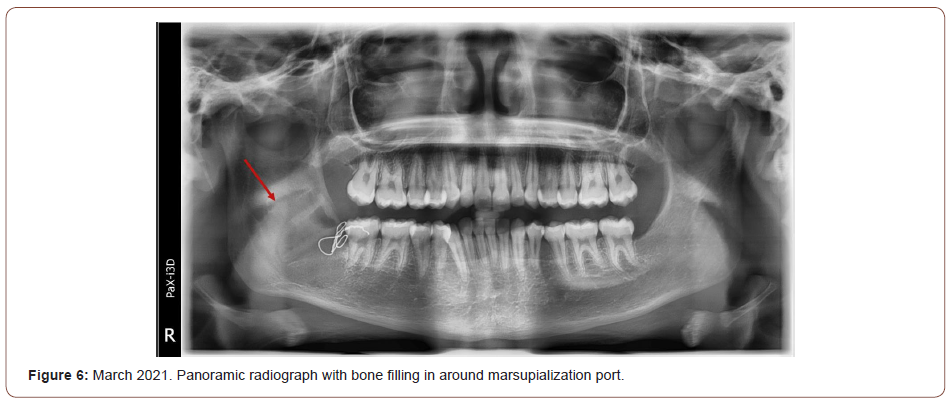
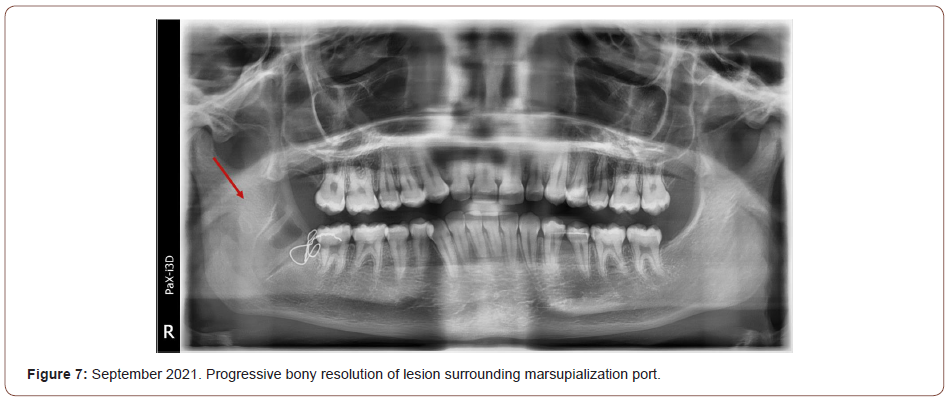
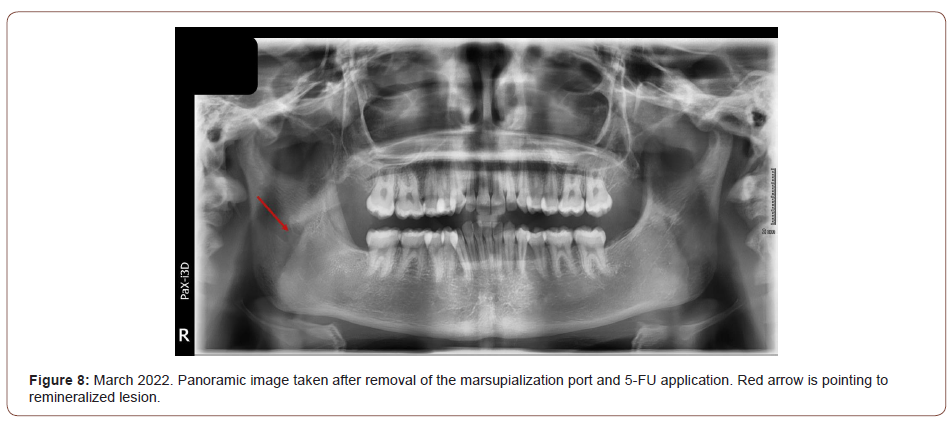
A marsupialization port was placed at the time of surgical biopsy to avoid a second surgery (Figure 5 – cropped panoramic of port wired in with red arrow pointing to suction tubing). A 21 gauge wire was used to secure a section of suction tubing to the alveolar bone using a transalveolar technique and the remaining soft tissue was sutured around the port head and alveolar bone. The patient recovered without any gross complications and with mild to moderate edema persisting for 7-10 days. The patient was prescribed peridex rinses and oral amoxicillin to be taken 500mg, three times a day. The patient was instructed to irrigate the marsupialization port 2-3 times a day with warm salt water. Panoramic images taken at follow-up appointments indicated the lesion was healing and the cavity was becoming remineralized (Figures 6, 7 -March and September, 2021, respectively. Panoramic radiographs with bone filling in around port). The patient was compliant with port management and there was no development of subsequent infections. Approximately 12 months after the initial surgery, the port was removed under intravenous sedation. 5-fluorouracil (FU) cream was packed, then removed after 24 hours. Radiographs from three months after removal of the port shows complete resolution of the lesion and bony regeneration (Figure 8-March, 2022 panoramic with red arrow pointing to remineralized lesion). Due to the known high recurrence rates of OKCs, a longer follow-up period and subsequent panoramic image is required to determine the efficacy of the treatment.
Discussion
Although benign, odontogenic keratocysts (OKCs) are aggressive lesions that can cause significant morbidity and are difficult to manage due to the high recurrence rates. While they can occur in both the maxilla and mandible, they are much more often found in the mandible [1, 2]. OKCs have been previously classified as keratocystic odontogenic tumor (KOT) and there is an ongoing debate between whether to classify the lesion as a cyst or tumor. The lesion is lined by odontogenic epithelium, often associated with unerupted teeth. But the aggressive clinical presentation with the high recurrence rate has led to past tumor classification [3].
Recurrence rates have been reported to be anywhere between 10-60% [2]. A systematic review conducted by Kaczmarzyk, et al. [4] found that recurrence rates can vary widely between different treatment modalities. Treatment for OKCs include enucleation, curettage, marsupialization, resection, and combinations of the aforementioned techniques with cryotherapy or Carnoy’s solution [1, 3, 4]. More radical treatment modalities such as resection are thought to have lower recurrence rates, but they certainly cause higher morbidity and the quality of evidence due to the lengths of follow-up does not support any particular treatment modality over others [4]. In the same systematic review, three cases of resection with a mean follow-up period of 5.25 years found zero cases of recurrence, but the length of follow-up is a major point of weakness [4]. Similarly, Tabrizi, et al. [2] followed 13 patients for 60 months following treatment of OKC by marsupialization and saw total resolution in 10 patients. But again, the length of follow-up is too short for adequate evaluation.
An adjunct to surgical treatment that shows promise in minimizing recurrence of OKC is the topical use of 5-fluorouracil (5-FU). The molecular genetics behind the theory behind the use of 5-FU is that the lesions grow due to mutations in the patched homolog (PTCH) tumor suppressor gene. The mutated gene leads to smoothened (SMO) activation, which leads to sonic hedgehog (SHH) signaling and unregulated cell proliferation. 5-FU has been shown to induce apoptosis in hepatocellular carcinoma cells via its inactivation of SHH in the PTCH tumor suppressor gene pathway and thus, has been shown to be effective in decreasing the risk of recurrence of OKC [1].
While in the case presented, full bony healing of the lesion was achieved following marsupialization and topical application of 5-FU, the three-month follow-up period is a limitation that is repeatedly seen in many studies and case reports. Recurrence of OKC have been reported decades after the initial surgical management, even with a case recurring 41 years later [4]. Thus, claims of successful treatment of OKC must be carefully evaluated and long-term followup is essential to monitor for recurrence.
Acknowledgement
None.
Conflict of interest
No conflict of interest.
References
- Ledderhof NJ, Caminiti MF, Bradley G, Lam DK (2017) Topical 5-Fluorouracil is a Novel Targeted Therapy for the Keratocystic Odontogenic Tumor. J Oral Maxillofac Surg 75(3): 514-524.
- Tabrizi R, Özkan BT, Dehgani A, Langner NJ (2012) Marsupialization as a treatment option for the odontogenic keratocyst. J Craniofac Surg 23(5): e459-e461.
- Singh AK, Khanal N, Chaulagain R, Bhujel N, Singh RP (2022) How effective is 5-Fluorouracil as an adjuvant in the management of odontogenic keratocyst? A systematic review and meta-analysis. Br J Oral Maxillofac Surg S0266-4356(22)00065-1.
- Kaczmarzyk T, Mojsa I, Stypulkowska J (2012) A systematic review of the recurrence rate for keratocystic odontogenic tumour in relation to treatment modalities. Int J Oral Maxillofac Surg 41(6): 756-767.
-
Emily Li, James J Closmann, Oliver H Chang, Henry H Rowshan. Clinicopathologic Correlation: Pericoronal Unilocular Radiolucency in the Posterior Mandible. On J Dent & Oral Health. 5(5): 2022. OJDOH.MS.ID.000623. DOI: 10.33552/OJDOH.2022.05.000623.
-
Keratocystic odontogenic tumor, Teeth, Cavity, Oral amoxicillin, Pediatric dentist, Oral and maxillofacial clinic, Temporomandibular joint, Inferior alveolar canal, Tooth, Odontogenic keratocysts
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






