 Research Article
Research Article
Clinical Outcome of Root Analog Dental Zirconia Implants: A Systematic Literature Review
Chin Chen Chong1* and Jacqueline A Pfaff2
1Chong & Partners Dental Clinic, Malaysia
2Polyclinic for Dental Surgery and Implantology, Goethe University Frankfurt, Germany
Chin Chen Chong, Chong & Partners Dental Clinic, Johor, Malaysia.
Received Date: August 24, 2020; Published Date: September 04, 2020
Abstract
Purpose: The purpose of this systematic review is to evaluate the clinical significance and outcome of custom-milled root analog zirconia implants (RAZI) for immediate replacement of an untreatable tooth.
Materials and methods:b> A PubMed search was conducted to acquire the articles which were published between 1st Jan 2000 to 31st July 2019. The topic related to the clinical outcome for root analog zirconia implants. Different combinations of the keywords “dent*, impel*, root, tooth, zirconia, shaped, analog and analogue” were searched.
Results: An initial 284 publications with abstracts were collected. Finally, seven articles meeting our inclusion and exclusion criteria and were selected for full text analysis in this review. This review was able to identify two immediate RAZI hybrid implant studies and five immediate delayed studies on full zirconia RAZIs. Single-rooted as well as two-rooted molar RAZIs were described. All successfully osseointegrated RAZIs had promising primary stability as a precondition. Radiological analysis showed no significant changes of the marginal bone. The representative overall implant survival rate was 91.30 %. Implants with only sand-blasted surface modification failed.
Conclusion:b> From the seven studies showing relative promising data that the individual custom milled RAZI is a predictable and successful method for immediate teeth replacement. In the future, more studies and long term clinical observational data need to be conducted to prove that this novel approach is feasible safe treatment for patients.
Keywords: Root analogue; Zirconia; Implant; Immediate; Clinical outcome
Abbreviations: 3D: Three dimensional visualisation; BID: Twice daily; CAD: Computer-aided design; CAM: Computer-aided manufacturing; CBCT: Cone beam computed tomography; DICOM: Digital imaging and communication in medicine file; DVT: Digital volume tomography; RAZI: Root analog zirconia implant; STL: Standardized triangulation language; TID: Three times daily
Introduction
Historic background
Looking for back in history around 550 BC, human beings used to carve and shape wood, metal, shells or bone to tooth morphology as an implant for replacing their missing teeth [1]. In 1969, Hodosh, et al. [2] was the first to duplicate a custom-made root shaped implant by using auto-polymerized and heat-processed polymethacrylate [1,3-8]. As compared to the conventional implant, the root shaped implant was congruent and tapped into the extraction socket without osteotomy. This customized root shaped implant technique was beneficial regarding any bone and soft tissue resorption but ended up with implant encapsulated by fiber tissue. As such, the customized root shaped implant technique was not used for years until 1992, when Lundgren, et al. [9] introduced the first root shaped implants made of titanium with successful osseointegration of 88 % of the implants [8,9].
A good fit between the implant and the extraction socket was described as an important factor for the success of implantation. In 1996, Kohal, et al. was the first one to use digital manufacturing process, computer-aided manufacturing (CAM) to fabricate root analog implant [7,8] and was constantly improved. He further refined the novel approach of root shaped titanium implants by widening the coronal aspect of the implant to compensate for the lost periodontium, so that the implant have a good congruent with extraction socket [1,3,4,6]. In few cases, the implant insertion fractured the thin buccal wall of the alveolar bone. Experimental studies in monkeys gave favorable results with clear evidence of osseointegration and clinical stability. Since then, studies on rootanalog implants technique showed successful approaches.
Purpose
Since the zirconia root-analog implant is a novel treatment approach clinically, the sufficiency and safety of this treatment procedure is still need to be studied. Hence, the purpose of the present study is to evaluate the clinical significance and outcome of root shaped zirconia implant for immediate replacement of an untreatable tooth.
Metal free implant
The metallic ions released from the oxide layers on the titanium alloy surface were found in tissue close to implants and in regional lymph nodes [10]. This finding is uncertain in the clinical relevance but because of this side effect more and more patients demand for metal-free implantation. Therefore, zirconia implants have several beneficial characteristics compared to titanium implants, which make them a good choice for immediate implantation.
Immediate implantation
Immediate zirconia implantation is essential for patients whose teeth need to be immediately replaced not only functional but also aesthetically. The advantages of immediate implants are less surgical interventions, less dental visits equivalent to increased quality of life and cost effective. Because of early functional loading effect, bone resorption and gingival recession are apparently reduced though limited [1,3-7]. So far, preformed standardized titanium implant are the standard implants used for immediate implantation.
Zirconia implants
Zirconia, a biologically inert materials, has high biocompatibility which facilitates osseointegration [1,3-6,10-13]. The properties of zirconia are not only mechanically favorable for its capability of stress distribution and corrosion resistance but also with the tooth color in shade, making it more acceptable and popular among the patients who show thin mucosa biotype in aesthetic zone and deficiency of the buccal bone. More importantly, due to the low affinity of zirconia to biofilm, there will be less periimplantitis excepted around zirconia implants. The demand for ceramic materials with tooth-like colors and high biocompatibility is increasing at about 12 % per year [12].
Root analog implants
Customised root shaped zirconia implants have one major indication: the immediate replacement of a severely decayed, fractured, endodontically failed or accidentally avulsed tooth. The uprising idea behind root shaped zirconia implants is that the root shaped zirconia implant is congruent to the fresh extraction socket, thus bone and soft tissue are less traumatized and need less healing process. For immediate implant placement, conventional screwed or cylindered type implants are incongruent [1] with the socket at which drilling is necessary to accommodate the shape of the conventional preformed implant causing a traumatised socket with necrosis, thus early resorption of the alveolar bone [1]. There is also the slight risk of down growth of the epithelium or connective tissue between the thin buccal cortical bone [1,3,5,6].
Aim
1. To provide an insight into the techniques of manufacturing root analog zirconia implants (RAZI).
2. To evaluate the survival rate and failure rate of RAZI.
3. To evaluate the primary stability of RAZI.
4. To investigate on the radiological and histological results after implantation of RAZI.
Hypothesis
is hypothesized that the individual true anatomical root analog dental zirconia implant is the best alternative implant with good primary stability, quick and uneventful healing of the bone and soft tissue with high survival rates.
Material and Methods
Pubmed search strategy
A PubMed search was performed to acquire the articles that are related to the title of this literature review: “Clinical Outcome of Root Analog Dental Zirconia Implants”. The keywords used were dent* AND impl* AND a various combination of the words root, tooth, zirconia and shaped. Both keywords in both writing options analog and analogue were included to make sure that no articles were left out in this search.
The Pubmed searches were performed on 31st July 2019 with the following keywords:
dent* AND impl* AND root analogue-27 articles
dent* AND impl* AND root analog-20 articles
dent* AND impl* AND tooth analogue-78 articles
dent* AND impl* AND tooth analog-90 articles
dent* AND impl* AND root AND zirconia-42 articles
dent* AND impl* AND root AND shaped-27 articles
Total-284 articles
After applying the filter “publication date 1st Jan 2000 to 31st July 2019“, the search result was reduced from 284 articles to a total of 257 articles. The results are shown below:
dent* AND impl* AND root analogue-23 articles
dent* AND impl* AND root analog-18 articles
dent* AND impl* AND tooth analogue-72 articles
dent* AND impl* AND tooth analog-85 articlesdent* AND impl* AND root AND zirconia-40 articles
dent* AND impl* AND root AND shaped-19 articles
Total-257 articles
Inclusion criteria
1. Studies in English language.
2. Studies that reported on custom milled root shaped dental zirconia implants.
3. In vivo studies in humans.
4. Publication date 1st Jan 2000 to 31st July 2019.
Exclusion criteria
1. In vitro studies.
2. Animals studies.
3. Non hybrid titanium implants.
4. Those studies done before year of 2000.
Final study inclusion
The titles and abstracts of the 257 potentially relevant articles were screened. With the combination of inclusion and exclusion criteria and the elimination of duplicates, 15 articles were found to be fulfilling the inclusion criteria and were therefore included in this study. The 15 full text articles were studied in detail.
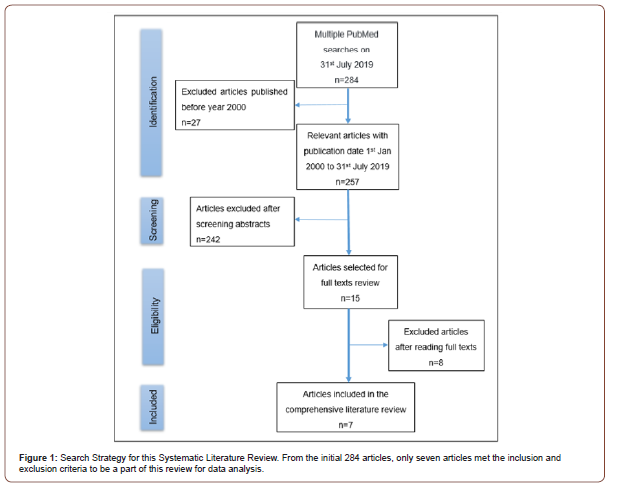
Eight articles were excluded for various reasons due to the inclusion and exclusion criteria. Three articles by German Gómez- Román, et al. [14-16] had to be excluded eventually because the studies were not using customized milled root shaped zirconia implants but root analog stepped implants or ready-made conventional root analog titanium implants. They did not fulfill the prerequisite criterion “custom milled root shaped zirconia implant”. Another article described prefabricated root analog endopore implant by Hi Tech implant system [17]. Three articles were reviews [10-13] and one articles evaluated root shaped zirconia implants not in humans but cadaver specimens [11]. Finally, a total of seven articles met all criteria to be included in this systematic literature review. An overview of this systematic search and exclusion of articles is documented in (Figure 1).
Statistics
Descriptive statistics were performed.
Results
Overview of included articles
Seven studies were included for this systematic literature review. The studies were published in the years 2008 to 2018 in the following journals: The International Journal of Oral and Maxillofacial Implants; Journal of Maxillofacial Oral Surgery; The International Journal of Periodontics and Restorative Dentistry; and International Journal of Oral Maxillofacial Surgery. All of the seven studies were prospective studies and consisted of five clinical case reports, one pilot study and one non-randomised controlled clinical trial. A general descriptive overview of these studies is listed in (Table 1).
A total of 28 patients with 29 RAZIs were involved in this systematic literature review. Of these, the pilot study by Moin et al. contributed data from 5 patients with 6 RAZIs [18] and the non-randomised controlled clinical trial by Picker W and Kocher A involved 18 patients and 18 RAZIs [1]. Each of the five clinical case reports reported on single patients with each one RAZI. Of the seven included studies, six were flapless atraumatic extractions except one which did not provide any extraction detail [6]. As described in (Table 2), there were four studies included, in which the implants were loaded within 12 to 16 weeks after implants placement, while two studies used loading protocols of 24 and 28 weeks and one study utilised a 12-52 weeks loading protocol. Five articles studied placement of single-rooted RAZIs in anterior and premolar region, whereas two included studies involved doublerooted RAZIs inserted in molar region [5,6].
RAZI -Root-analog zirconia implant, n/a-data not accessible, tid-three times daily, bid-twice daily.
The manufacturing techniques of RAZI
Two types of treatment approaches were observed in this review. The first approach is immediate delayed implantation [1,3-6] where the extraction socket is replaced with a root shaped zirconia implant after 1 to 8 days of extraction. Cotton soaked with iodoform was placed in the socket before the replica zirconia root implant was ready. The extracted root was scanned and an analog was designed by computer-aided design (CAD) according to original root shape. Standardized Triangulation Language (STL) file of the extracted tooth was transferred to computer-aided manufacturing (CAM) for milling a final anatomical root shaped zirconia implant. The specific modification of these natural root geometry implants [1,3-6] are paramount conditions to guarantee a success in immediate-delayed implantation as stated in the following:
1. Microretention with sand blasted and acid etched the whole surface of the replica.
2. Macroretention design with standardized protruding bulbs at interdental space.
3. 0.1mm-0.5mm reduction of the labial of the root replica adjacent to the buccal plate of the extraction socket (only described in first approach with CAD/CAM of extracted root).
4. Sterilization of the replica before placing it inside the extraction socket by finger pressure and gently tapping with hammer and mallet.
The second approach was an immediate implantation for a single tooth replacement with an individual root analog hybrid implant [7,18]. These were innovative immediate implant cases whereby the exact one-piece anatomical root shaped hybrid implant and the try-in zirconia implant were fabricated prior to the tooth extraction. Three dimensional visualisation (3D) or digital volume tomography (DVT) from cone beam computed tomography (CBCT) and the detailed morphology of the soft and hard tissue surrounding the unrestorable tooth were recorded by intraoral scanner.
Digital imaging and communication in medicine file (DICOM) format from CBCT and STL file from the scanner were superimposed in CAD to attain a 3D envelope data mesh of the tooth with specialised proprietary analysis software (the REPLICATE System, Natural Dental Implants). With this STL data information, the CAM machine with five axis of cutting burs milled two pieces of customized root shaped analog implants, one zirconia implant for try-in and one titanium implant fused with the zirconia abutment for actual restoration. Both immediate implantation studies used a titanium root fused with glass solder matrix. Specifically designed features like macro-retentions (standard-sized protruding bulbs on the mesial and distal aspect) and micro-retentions (sand-blasting and acid-etching) were added for a well-compatible root analog implant.
Survival rate and failure rate
Within 6 to 36 months of observation periods, the survival rates of an immediate placement of custom milled RAZIs ranged from 0 % to 100 % for all the included studies. A 100 % failure rate of RAZIs, however, shall only result when the surface of RAZIs was only sand blasting, as occurred to group A of the study by Pirker and Kocher [1]. The overall survival and failure rate shall be 72.41 % (21/29 RAZIs) and 27.59 %, respectively. However, if we take out this group A of only sand-blasted implants to correct our calculations, the overall implant survival rate should be 91.30 % (21/23 RAZIs) provided that the RAZIs specific design features on the root surface and the topography of the RAZIs are applied (Table 3).
Table 1: Overview of Included Studies.
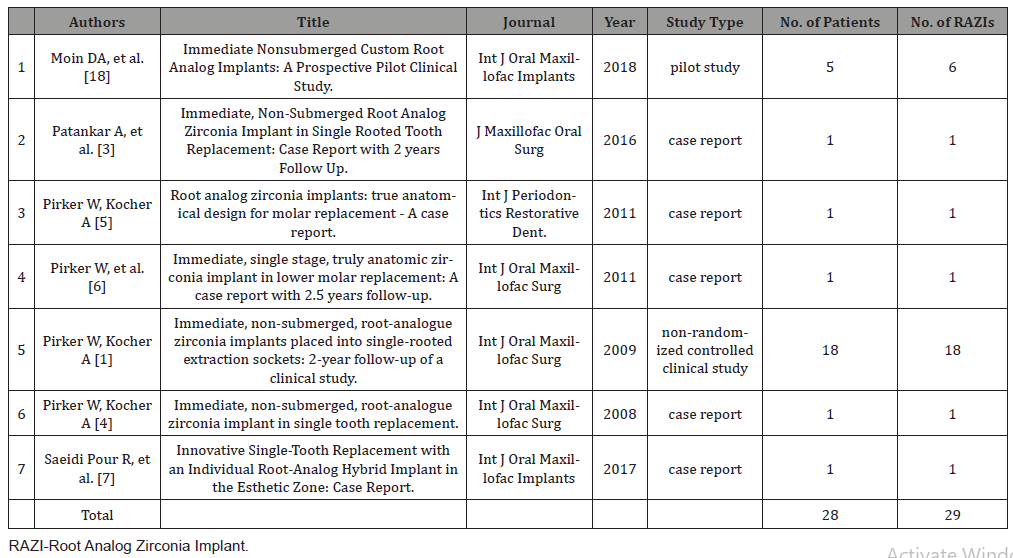
Table 2: Extraction and Loading Protocols of the Included Studies.
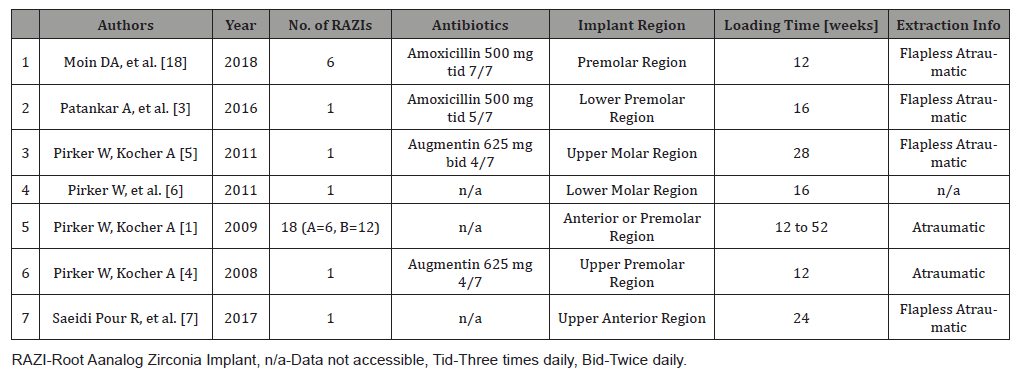
Table 3: Survival and Failure of Root Analog Zirconia Implants.
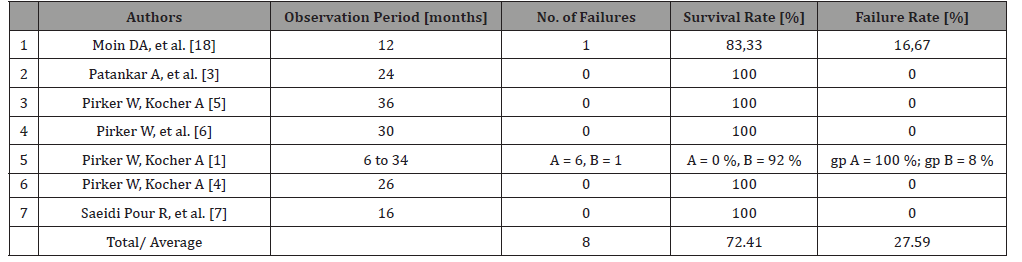
Table 4: Radiological Evaluation and Clinical Evaluation of Primary Stability.
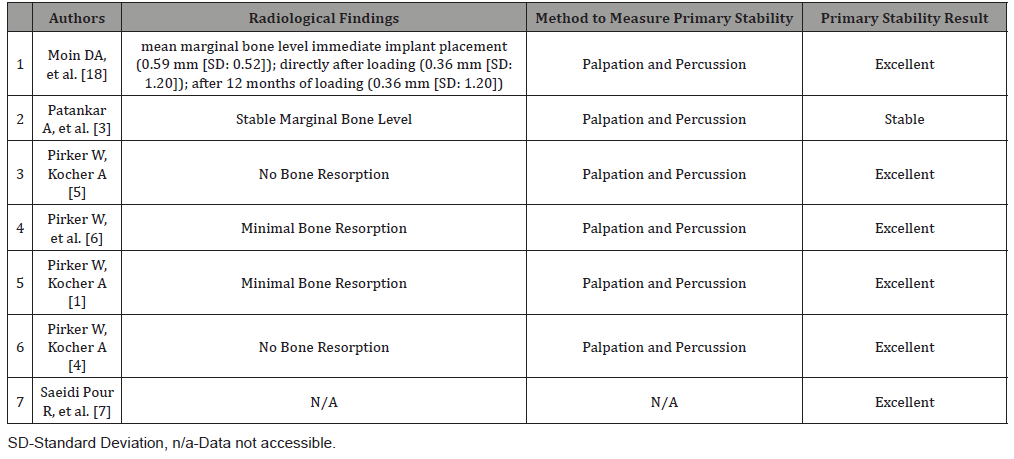
Analysis of primary stability
Seven studies proved that all successfully osseointegrated RAZIs achieved stable or excellent primary stability. Primary stability was clinically evaluated by palpation and percussion. Objective methodologies to measure the primary stability were not mentioned. (Table 4) gives an overview of the clinical evaluation of the primary stability and the radiological findings of the seven included studies (Table 4).
Radiological analysis of marginal bone Level
The seven included studies reported of no significant changes but rather stable marginal bone as can be reviewed in (Table 4). Moin, et al. [18] performed a detailed analysis of the marginal bone at three different time points in six RAZIs [18]. The mean marginal bone level was at 0.59 mm (±0.52 mm) after insertion of the root analog implants, at -0.36 mm (±1.20 mm) after definitive restoration and at -0.31 mm (±0.90 mm) at 12 months after loading. The bone level, which was surrounding the root analog implants, appeared to be stable with a mean value of -0.31 mm (±0.90 mm) and minimal bone resorption after 12 months post function.
Histological analysis
None of the seven included articles performed any histological analysis. No data is available at this time.
Discussion
First clinical cases demonstrate that with the combination of the CBCT and CAD/CAM, the fabrication of customized root shaped implants prior to surgery is now a clinical reality, which offers the benefits of an immediate implantation with an individualized anatomically designed zirconia implant. The placement of a truly anatomical root analog (hybrid) zirconia implant can be a very successful technique both as immediate delayed implantation [1,3-6] and as immediate implantation [7,18]. This procedure has numerous benefits: one time surgical intervention, no osteotomy procedure, less visits, shorter time of having a temporary, cost effective, single unit of implant with abutment to avoid any micromovement, beneficial esthetic outcome, no allergic effect to the surrounding tissue and metal-free implantation. This surgical method can be applied even in areas with lack of apical bone [11]. Immediate custom-milled RAZIs are not only able to replace the anterior single-rooted tooth in the aesthetic zone but also the tworooted teeth in the posterior region of the maxilla or mandible [5,6]. In other words, any of the untreatable teeth in the oral cavity of a patient can be replaced immediately. All of these advantages may encourage clinicians and patients to choose custom-milled root identical zirconia implants as a choice of treatment for immediate replacement of an untreatable tooth.
Techniques of manufacturing RAZIs and its design features
The topography of a customized RAZI is a very important factor to ensure the success of an immediate implantation. The nonrandomized controlled clinical study by Picker and Kocher proved that the immediate implantation will fail if the surface of RAZIs was only sand-blasted [1]. The following recommendations of the RAZI design features and modifications are a summary of the seven full texts included in this review [1,3-7,18].
1. Microretention: Sand-blasting and acid-etching of the zirconia surface will enhance the bone-to-implant contact and facilitating osseointegration.
2. Macroretention: Standardized protrusion bulbs at the mesial and distal aspects of the implant in the interdental zone help to accomplish primary stability and osseointegration.
3. Zirconia has higher elastic modulus (at about 240-260 GPa) than cortical bone (10-20 GPa) which can result in stress shielding and peri-implant bone loss [12]. Thus, about 0.1 mm to 0.5 mm reduction of the labial part of the implant will reduce the pressure to the cortical bone and prevent the fracture and resorption of the thin buccal plate of the extraction socket.
However, the mentioned techniques [1,4-6] are not in standardized protocol concerning retentive elements, surface modifications and the design relative to the specific anatomy of the extraction site. Those features were incorporated arbitrarily [11]. Not until Moin, et al. [18] who demonstrated a precise digital extraction and fabrication of a truly anatomical RAZI from CBCT data and CAD/CAM [18].
Survival rate and failure rate of RAZIs
When excluding the group of only sand-blasted implants [1] to correct our calculations, the overall implant survival rate was calculated to be 91.30 % (21/23 RAZIs) provided that the RAZI specific design features on the root surface and the topography of the RAZI were applied. The survival rate of immediate placement of RAZIs was 91.30 %, whereas the survival rates of the “normal” immediate pre-fabricated titanium implants were reported as 99 % [19] and 97.6% [20]. Reports of immediate titanium implants in the molar region resulted in a 5-year cumulative survival rate as low as 89 % [21]. Therefore, the survival rate of immediate RAZIs is acceptable and in accordance with other reviews but still allows for better achievements. Our included studies are primary case reports and first small clinical studies, from which we can assume that RAZI is considered as experimental approach with little experience at hand.
Primary stability of RAZIs
Primary stability is a very important factor for osseointegration of the RAZIs, since the RAZIs are one-piece implants with no option for submerged healing [18]. Historically, most of the RAZI failure cases were due to fracture of the thin buccal cortical plate at the time of implant placement and unable to achieve primary stability, which lead to unsuccessful osseointegration [11]. Therefore, macroretention is one of the prerequisite features in fabricating RAZIs. In order to achieve primary stability, standardized protrusion bulbs were recommended to be added at the mesial and distal aspects of the implant in the interdental zone. The herein included articles measured primary stability of RAZIs arbitrarily by palpation and percussion. No measurement devices such as Periotest were applied. We consider this as one of the shortcomings in study design and encourage future studies to include an objective measurement technique to assess primary stability.
Radiological results after implantation of RAZIs
No to minimal bone changes were shown in the radiographs resulting in rather stable bone conditions in the herein included studies. Multiple factors contribute to the stability of the bone margin in RAZIs. The non-submerged, one piece of implantabutment has the benefit that micro-movements, which will cause early bone resorption, can be avoided. Also, the single surgical procedure will not require any healing cap or removal of an abutment. In fact, the steps of removing the healing cap and abutment is unfavorable to connective tissue and gingiva, which may lead to tissue irritation and periodontitis [7], which may progress in bone resorption. Another reason for frequent bone resorption and gingival recession in cylinder or cone shaped conventional implants is that the recipient site has to be prepared by a special bur to accommodate the implant. In RAZI situations, no augmentation of bone particulates and connective tissue or membrane barrier is needed to prevent the possibility of down growth of the epithelium or connective tissue [1,3,5,6].
The congruency of the individual root analog zirconia implant to the contour of the extraction socket will not only create a condition for natural remodeling but also maintain the stress distribution in the hard and soft tissue surrounding the implant. This design can lead to minimal bone resorption due to stress shielding associated to peri-implant inflammatory reactions [12]. The stability of the bone level and the gingival margin of the implant restoration are the main contributing factors to positive radiological results. However, the stress distribution surrounding the implant is still high due to lack of periodontal ligament.
Histological results after implantation of RAZIs
Our review specifically included human in vivo studies only. Histological evaluations could not be identified in this review, since the included studies were performed in humans and not animals, which would be sacrificed later. The observation period was 6 to 36 months. Only few implants failed which could have served for histological evaluation and interpretation. At this moment, data is lacking. There are no histological evaluations of successfully integrated RAZIs in humans.
Shortcomings of this study
This review was able to identify two immediate RAZI hybrid implant studies [7,18] and five immediate delayed studies on full zirconia RAZIs [1,3-6]. Until today, there have been no studies reporting on immediate implantation of full zirconia custom milled RAZIs. These seven included studies resulted in a heterogeneous pool of studies. Also, the data of only sand-blasted RAZIs does not represent the overall survival and may also differ in other criteria, which resulted in a heterogeneous data [1].
Future outlook
Altogether, only few clinical reports on single implants and only two studies with small patient numbers are available on the matter of RAZIs. Due to the promising data of these first reports, we would like to encourage investigators to perform larger-sized clinical trials, which would provide sufficient statistical data.
Conclusion
Immediate placement of a truly custom milled RAZI has significant benefits over a conventional titanium implant. Although the studies of the immediate placement of the RAZIs are limited, the high survival rates, the stability of bone level and good primary stability of the RAZI are promising clinical outcomes appraised in this review. Including the patients with the correct indication for immediate implantation as well as following the specific design features during RAZI manufacturing are important criteria, which help to reach successful implantation. Further research and more studies are essential to warrantee the feasibility and long-term success of this novel approach in the future.
Acknowledgement
Many thanks go to the lecturers from the Master of Oral Implantology, Goethe University, Frankfurt, Germany for their enthusiasm and dedication.
Conflict of Interest
There are no conflicts of interest relating to this study.
References
- Pirker W, Kocher A (2009) Immediate, non-submerged, root-analogue zirconia implants placed into single-rooted extraction sockets: 2-year follow-up of a clinical study. Int J Oral Maxillofac Surg 38(11): 1127-1132.
- Hodosh M, Povar M, Shklar G (1969) The dental polymer implant concept. The Journal of Prosthetic Dentistry 22(3): 371-380.
- Patankar A, Kshirsagar R, Patankar S, Pawar S (2016) Immediate, Non-Submerged Root Analog Zirconia Implant in Single Rooted Tooth Replacement: Case Report with 2 years Follow Up. J Maxillofac Oral Surg 15(Suppl 2): 270-273.
- Pirker W, Kocher A (2008) Immediate, non-submerged, root-analogue zirconia implant in single tooth replacement. Int J Oral Maxillofac Surg 37(3): 293-295.
- Pirker W, Kocher A (2011) Root analog zirconia implants: true anatomical design for molar replacement--a case report. Int J Periodontics Restorative Dent 31(6): 663-668.
- Pirker W, Wiedemann D, Lidauer A, Kocher AA (2011) Immediate, single stage, truly anatomic zirconia implant in lower molar replacement: a case report with 2.5 years follow-up. Int J Oral Maxillofac Surg 40(2): 212-216.
- Saeidi Pour R, Randelzhofer P, Edelhoff D, Prandtner O, Rafael CF, et al. (2017) Innovative Single-Tooth Replacement with an Individual Root-Analog Hybrid Implant in the Esthetic Zone: Case Report. Int J Oral Maxillofac Implants 32(3): e153-e60.
- Saeidi Pour R, Freitas Rafael C, Engler M, Edelhoff D, Klaus G, et al. (2019) Historical development of root analogue implants: a review of published papers. British Journal of Oral and Maxillofacial Surgery 57(6): 496-504.
- Lundgren D, Rylander H, Andersson M, Johansson C, Albrektsson T (1992) Healing of root analogue titanium implants placed in extraction sockets. An experimental study in the beagle dog. Clin Oral Implants Res 3(3): 136-143.
- Van Dooren E, Calamita M, Calgaro M, Coachman C, Ferencz JL et al (2012) Mechanical, biological and clinical aspects of zirconia implants. Eur J Esthet Dent 7(4): 396-417.
- Evans ZP, Renne WG, Bacro TR, Mennito AS, Ludlow ME et al (2018) Anatomic Customization of Root-Analog Dental Implants with Cone-Beam CT and CAD/CAM Fabrication: A Cadaver-Based Pilot Evaluation. J Oral Implantol 44(1): 15-26.
- Pessanha-Andrade M, Sordi MB, Henriques B, Silva FS, Teughels W, et al (2018) Custom-made root-analogue zirconia implants: A scoping review on mechanical and biological benefits. J Biomed Mater Res B Appl Biomater 106(8): 2888-2900.
- Regish KM, Sharma D, Prithviraj DR (2013) An overview of immediate root analogue zirconia implants. J Oral Implantol 39(2): 225-233.
- German Gómez-Román, Stefan Rombach (2017) Vertical and Horizontal Crestal Bone Levels in Root-Analog Stepped Implants-A 10-Year Prospective Study. Implant Dent 26(4): 5245-5231.
- German Gomez-Roman, Steffen Launer (2016) Peri-implant bone changes in immediate and non-immediate root-analog stepped implants-a matched comparative prospective study up to 10 years. Int J Implant Dent 2(1): 15.
- German Gomez-Roman, Kruppenbacher M, Weber H, Schulte W (2001) Immediate postextraction implant placement with root-analog stepped implants: surgical procedure and statistical outcome after 6 years. Int J Oral Maxillofac Implants 16(4): 503-513.
- Nair A, Prithviraj DR, Regish KM, Prithvi S (2013) Custom milled zirconia implant supporting an ceramic zirconia restoration: a clinical report. Kathmandu Univ Med J (KUMJ) 11(44): 328-331.
- Moin DA, Hassan B, Wismeijer D (2018) Immediate Nonsubmerged Custom Root Analog Implants: A Prospective Pilot Clinical Study. Int J Oral Maxillofac Implants 33(2): e37-e44.
- Atieh MA, Payne AG, Duncan WJ, de Silva RK, Cullinan MP (2010) Immediate placement or immediate restoration/ loading of single implants for molar tooth replacement: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 25(2): 401-415.
- Sethi A, Kaus T (2017) Immediate replacement of single teeth with immediately loaded Implants retrospective analysis of a clinical case series. Implant Dentistry 26(1): 30-36.
- Schwartz-Arad D, Grossman Y, Chaushu G (2000) The clinical effectiveness of implants placed immediately into fresh extraction sites of molar teeth. J Periodontol 71(5): 839-844.
-
Chin Chen Chong, Jacqueline A Pfaff. Clinical Outcome of Root Analog Dental Zirconia Implants: A Systematic Literature Review. On J Dent & Oral Health. 3(3): 2020. OJDOH.MS.ID.000564.
-
Oral hygiene, Periodontal health, Tooth brushing, Dental surgeons, Orthodontic, Periodontal assessment, Dental plaque, Healthy periodontium, Dental floss, Oral irrigators.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






