 Research Article
Research Article
A Novel Technique for Orthodontic Gap Closure with Access through the Maxillary Sinus
Brigitte Wendl*, David Innerhofer, Margit Pichelmayer, Barbara Kirnbauer, Michael Payer and Norbert Jakse
Division of Oral Surgery and Orthodontics, Department of Dental Medicine and Oral Health, Medical University of Graz, Austria
Brigitte Wendl, Clinical Department of Oral Surgery and Orthodontics Medical University of Graz, Billrothgasse 4, 8010 Graz, Austria.
Received Date: July 27, 2022; Published Date: August 19, 2022
Abstract
Background: Orthodontic gap closure is an important alternative to prosthetic restorations on implants. However, the presence of bone of sufficient quality and quantity is critical to proper tooth movement in the maxilla, especially in patients with a markedly enlarged maxillary sinus. These two case reports demonstrate a new method to facilitate bodily gap closure through the maxillary sinus with the help of an interdisciplinary surgical approach (sinus lift and bone augmentation).
Material and methods: Two patients requiring orthodontic gap closure in regions with a markedly enlarged maxillary sinus and an area of atrophic bone that needed augmentation were treated with pre-orthodontic sinus lifts using the fully resorbable Guidor easy-graft Classic (Sunstar) augmentation material. Superelastic tension springs and miniscrews were chosen as orthodontic appliances. Target parameters were evaluated preoperatively, directly postoperatively and after the gap closure using CBCT datasets and models.
Results: The maxillary sinus was radiologically inconspicuous in all datasets. 3D evaluation of the tooth movement showed proper translational tooth movement.
Conclusion: Radiological and clinical evaluation of these two orthodontic cases showed successfully translational orthodontic tooth movement through an enlarged sinus supported by bone augmentation using a synthetic augmentation material. There were no significant signs of root resorption.
Keywords: Orthodontic cap closure; Sinus lift; Bone augmentation; Xenogeneic bone substitute; Translational orthodontic tooth movement
Introduction
Orthodontic gap closure is an important alternative to prosthetic restorations on implants. However, the presence of bone of sufficient quality and quantity is critical to proper tooth movement in the maxilla to achieve gap closure without root tipping or root resorption, especially in patients with a markedly enlarged maxillary sinus.
Kilic, et al. [1] showed that the distance between the sinus floor and the root tip was greatest for first premolars and shortest for the buccodistal roots of second molars on both the right and the left sides. Since molar roots are located close to the maxilla, the remaining bone height as well as the osseous elongation of the sinus will affect the available options for tooth movement. Sharan and Madjar [2] reported that the extraction of second molars led to greater expansion than did the extraction of first molars. They also reported that extractions of two or more adjacent posterior teeth caused greater sinus expansion.
Wehrbein, et al. [3, 4] proposed a quantitative description of the degree of tipping and kind of movement as a function of the configuration and extension of the basal maxillary sinus. It has been shown that with a more vertical extension in front of the tooth to be moved, a higher amount of tipping (about 10°) is obviously to be expected than for teeth moved through a more horizontally extended sinus base. A correlation was also found between the depth of the maxillary sinus recess and the amount of tipping: the deeper the maxillary sinus recess, the more pronounced the tipping. Re, et al. [5] showed in a case report that direct remodelling results in a dislocation of the lamina dura and, hence, complete remodelling of the sinus.
Tooth movement in the presence of anatomic limitations can be facilitated by surgical interventions such as corticotomies, which, like dentoalveolar distraction, have been proposed as effective and safe methods to abbreviate orthodontic treatments in adolescent and adult patients [6].
In addition, augmentative techniques can be used to advantage to move teeth more safely and to improve the physical transmission of force. Tooth movement through xenogeneic bone substitute materials has been shown to be successful in animal experiments demonstrating that tooth could be moved into an alveolar ridge area augmented with a biomaterial (Bio-Oss; Geistlich, Wolhusen, Switzerland) three months previously [7]. Furthermore, bone grafting material was also successfully used in moving mandibular front teeth in Class III patients receiving combined orthodontic and surgical treatment [8, 9].
Reichert, et al. [10] showed that orthodontic gap closure in extraction sockets filled with silica matrix-embedded, nanocrystalline hydroxyapatite bone substitute is possible without inflammation or root resorption. Kye-Bok Lee, et al. [11] demonstrated that augmented corticotomy effectively reestablished periodontal soft and hard tissue on the pressure sides after buccal tooth tipping, regardless of the type of grafting material used. The synthetic bone graft group, which had exhibited the greatest changes in angles during tipping, also showed most new bone formation and most intact soft tissue.
At present, no evidence-based protocol can be recommended for moving teeth through the maxillary sinus. According to the systematic review by Sun, et al. [12] the empirical application of constant and light to moderate force (by TAD, segment and multibrackets) to move teeth slowly through or into the maxillary sinus in adults appears to be the most secure way. Bodily movement was accomplished, but teeth appear to be easily tipped initially, potentially resulting in root resorption.
Given the absence of pertinent data in the literature. the question arises whether augmentative techniques might facilitate bodily tooth movement and the transmission of more physical force for gap closure through a markedly enlarged sinus.
Material and Methods
Two patients required orthodontic gap closure in regions with a markedly enlarged maxillary sinus and an area of atrophic bone that needed augmentation.
The bone height in the gap regions was reduced to less than 5mm, with the root tip presenting above the sinus floor in the panoramic radiographs.
Exclusion criteria were: severe general diseases, antiinflammatory medication, allergies to one or more of the materials used, tooth extraction in the gap region less than half a year previously, and insufficient oral hygiene.
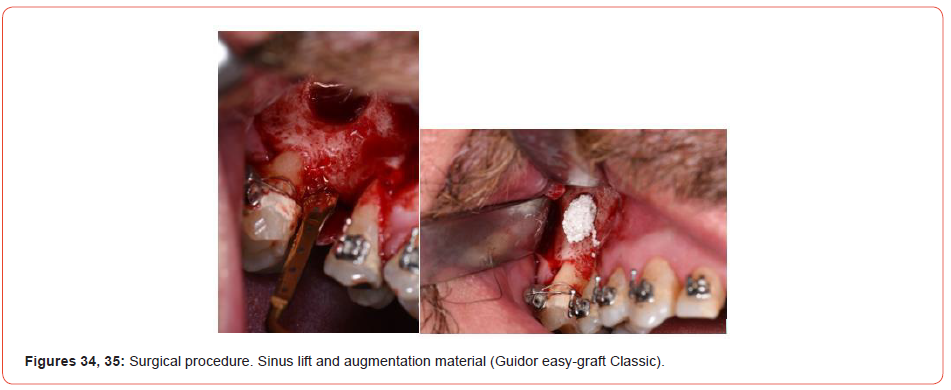
Both patients were treated with pre-orthodontic sinus lifts using the Guidor easy-graft Classic augmentation material (Sunstar, Etoy, Switzerland). This material is fully resorbable and is replaced by autologous bones within months thanks to the phase-pure betatricalcium phosphate (β-TCP) it contains.
The direct sinus lift procedure employed was that described by Oscar Hilt Tatum. After uncovering the lateral wall of the jaw by reflecting a flap, the thin lateral wall of the jaw is weakened circularly with a spherical diamond drill in an area of approximately 1-2 cm². The resulting cover is “lifted” inwards together with the Schneiderian membrane adhering to the inner side, creating a fairly large cavity in which the synthetic bone substitute material is inserted.
Orthodontic appliance
Superelastic tension springs were chosen as orthodontic appliances as these are able to deliver forces of 1.5 Ncm in a standardized manner. Furthermore, lever arms and mini-screws were used for skeletal anchorage.
Bone heights, tooth positions, tooth movements and root resorption were evaluated preoperative, directly postoperatively and after the gap closure using CBCT datasets (Promax 3D Max, 10.0 × 5.9cm, 200 μSv, low dose, 96 kV, 6.3 mA; Planmeca, Helsinki, Finland) and models. Photographic documentation was carried out at the end of the treatment.
Translational tooth movement was verified clinically by way of stone casts and radiologically using two DICOM datasets. An A dataset (obtained postoperative but prior to the orthodontic tooth movement) and a B dataset (obtained at the end of orthodontic treatment) were superimposed using the coDiagnostiX (Dental Wings, Chemnitz, Germany) implant-planning software. The datasets were segmented digitally for a three-dimensional display of the hard-tissue structures, including the maxillary teeth and bones (nasal concha, nasal spine, borders of the upper maxillary sinus, parts of the zygomatic arch, parts of the sphenoid bone). The segmented A datasets was then imported into the B datasets. Their superimposition was performed on the basis of the segmented stable hard-tissue structures listed above and displayed as virtual 3D models. The coDiagnostiX software displayed virtual 3D models three-dimensionally in a separate window and within the axial, coronal and sagittal layers marking the borders of the previously segmented structures (bone and teeth).
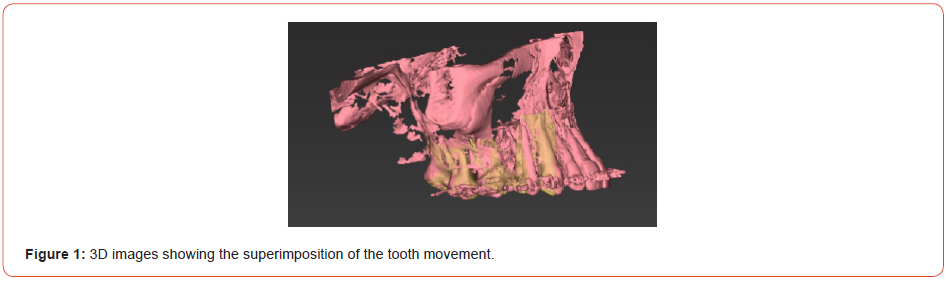
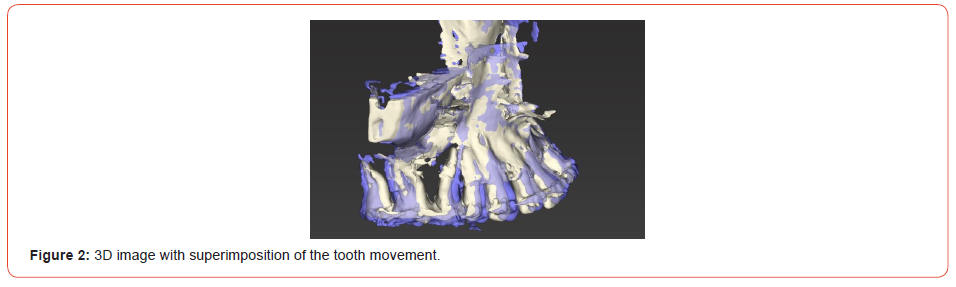
Tooth positions and movements were measured in the axial and sagittal layers. To this end, the axial layer was adjusted to be parallel to the occlusal plane and positioned relative to the position of the alveolar crest. The sagittal layer was positioned to intersect the middle of the second premolar and first molar along the panoramic curve/dental arch. The distances between the positions of the premolar and molar adjacent to the gaps as well as tooth movement were measured at the level of the alveolar crest and of the root tips by superimposing the A and B datasets. Dimensions of augmentation (height, mesiodistal width, buccopalatal width) were measured separately in the A and B datasets (Figures 1, 2 for patients 1 and 2, respectively).
Results
Radiological findings
The A and B datasets showed age-appropriate bone structures
in the maxilla for both patients. Molar roots had intruded into the
maxillary sinus by at least the apical third of their length. No root
resorption was seen in either the A or the B datasets. The maxillary
sinus was radiologically inconspicuous in for both datasets. The
postoperative A datasets showed a regularly positioned, welldemarcated
sinus augmentation, while both B datasets showed a
reduced volume of bone substitute material.
Patient 1
In the A dataset, the bone substitute exhibited a maximum
height of 9.5mm, a maximum mesiodistal width of 8.3mm and
a maximum buccolingual width of 11.0mm. At the end of the
orthodontic treatment, the corresponding dimensions were 6.1mm,
4.7mm and 6.8mm, respectively.
Patient 2
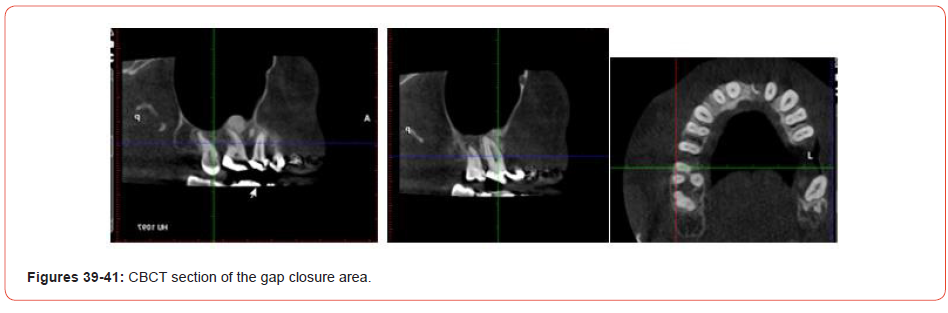
In the A dataset, the bone substitute exhibited a maximum
height of 10.8mm, a maximum mesiodistal width of 9.3mm and
a maximum buccolingual width of 11.2mm. At the end of the
orthodontic treatment, the corresponding dimensions were 6.6mm,
7.2mm and 10.2mm, respectively.
Patient 1
Diagnosis
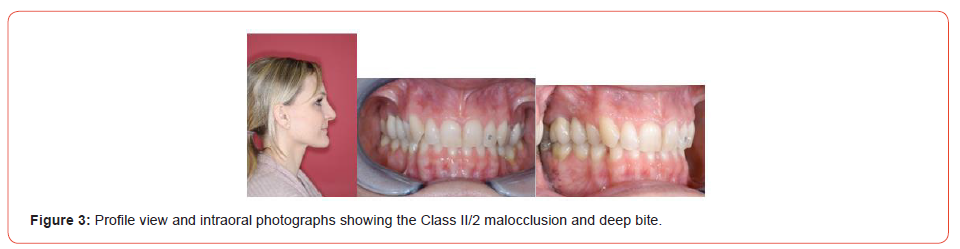
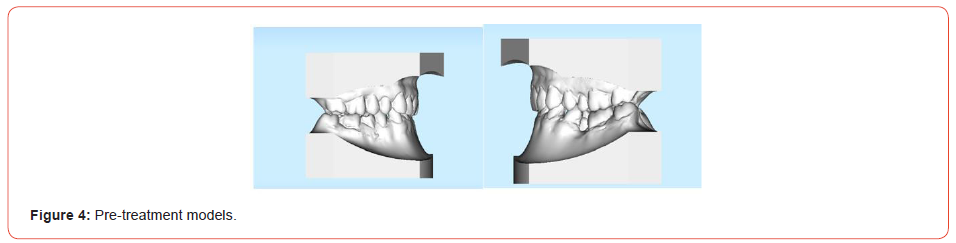
Patient 1 was a 38-year-old woman with a skeletal Class II/2
dysgnathia showing an overjet of 1 mm and an overbite of 6 mm
(Figures 3, 4). The profile appeared concave.
Cephalometric tracing yielded the following results:
SNA angle: 79°
SNB angle: 76.5°
Sum of angles: 387°
Angle of Inclination, upper anteriors: 83°
Angle of Inclination, lower anteriors: 84°
The patient exhibited bilateral half Class II malocclusion.
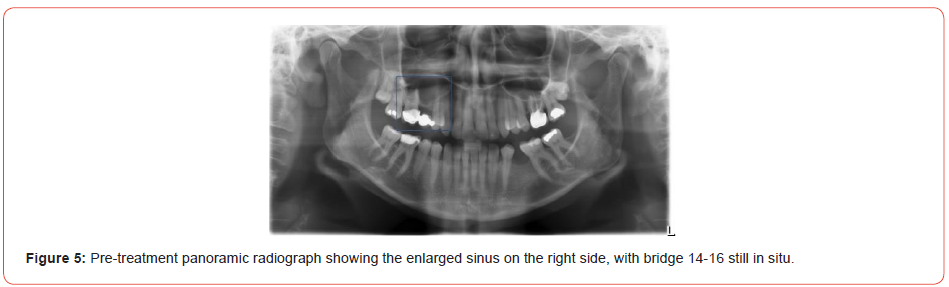
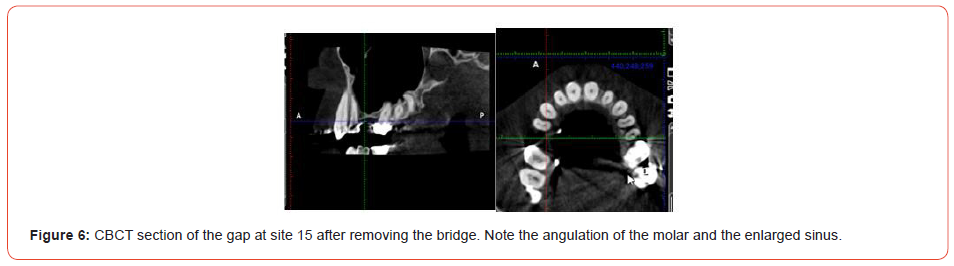
The panoramic radiograph and the CBCT sections showed a
markedly enlarged maxillary sinus and atrophic bone at site 15
(Figures 5-7).
In view of the deep bite and Class II malocclusion, the right
maxillary bridge was removed. The gap was closed by reciprocal
gap closure (facilitated by augmentation by way of a sinus lift). In
the left maxilla, a Class I occlusion was achieved by distalisation.
Treatment objectives and treatment alternatives
1. Periodontal evaluation and professional tooth cleaning
prior to treatment
2. Skeletal discrepancy to be compensated dentally, as
orthognathic surgery was not accepted by the patient
3. Transverse alignment of the maxilla
4. Full Class II molar relationship to be achieved on the right
side by removing the existing maxillary bridge and performing
reciprocal gap closure, and a Class I occlusion to be achieved by
posterior distalisation
5. Correction of the sagittal and vertical overbites
6. Correcting the inclinations and torques of the anterior
teeth
7. Uprighting of the mandibular right molars
8. Implant placement at site 35
9. Midline correction
10. Aesthetics: Broadening the smile and improving the smile
curve
11. Periodontal: Slowing or halting progression of the existing
recessions
12. Achievement of long-term stability
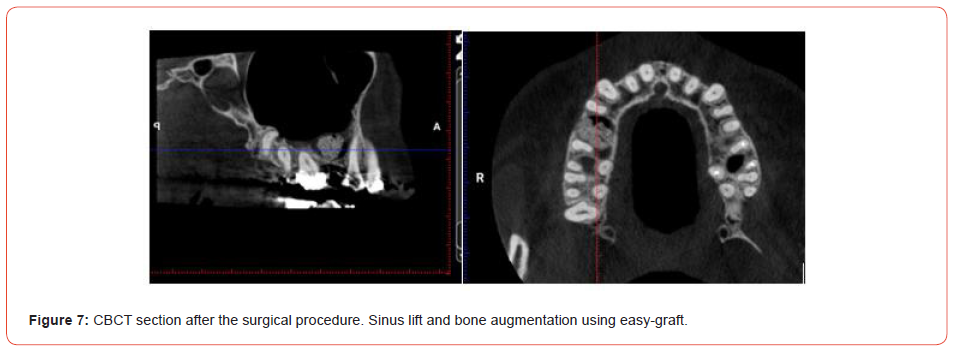
Treatment procedures
The maxilla and mandible were levelled and aligned using wires
of ascending order (0.014-0.016 × 0.022 -0.017 × 0.025). Prior to
gap closure, the sinus lift (Figures 8-12) and bine augmentation
(Guidor easy-graft Classic) was done by an experienced
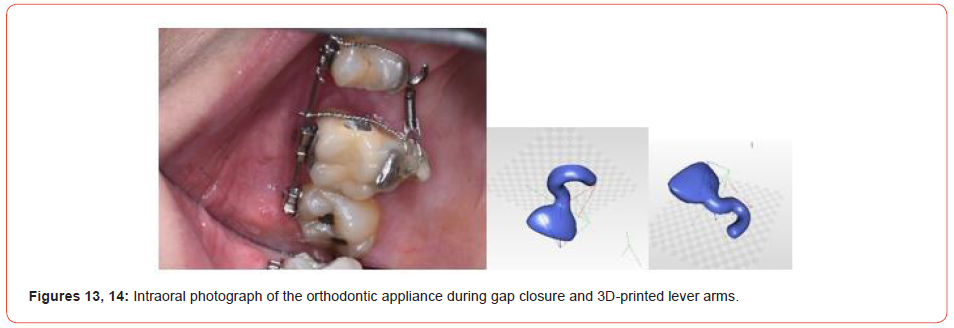
maxillofacial surgeon. To facilitate translational tooth movement,
custom 3D-printed lever arms were bonded to teeth 14 and 16. A
tension coil (150g) on a 0.017 × 0.025 stainless steel wire was used
for gap closure (Figures 13, 14).

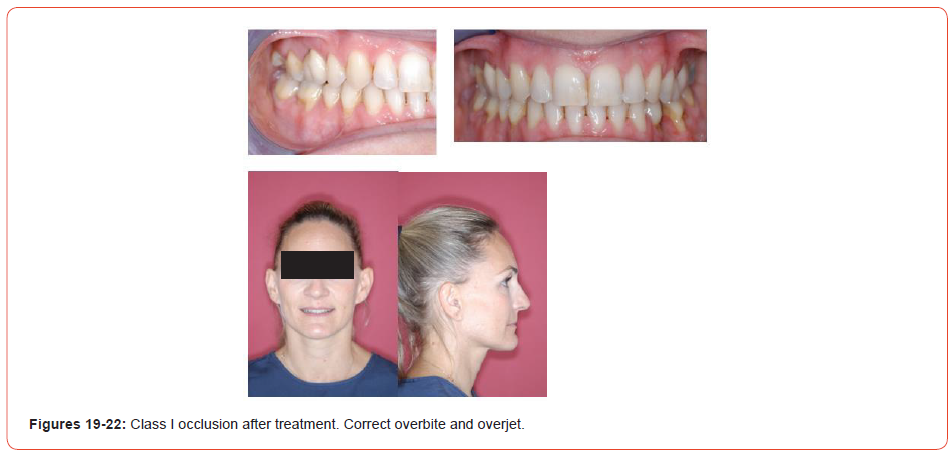
A correction to achieve a Class II relationship on the left side was performed using Class II elastics. To obtain good intercuspation, some vertical elastics were used towards the end of treatment. Orthodontic tooth movements and gap closure were carried out successfully, resulting in uprighted premolars and molars (Figures 15-18).
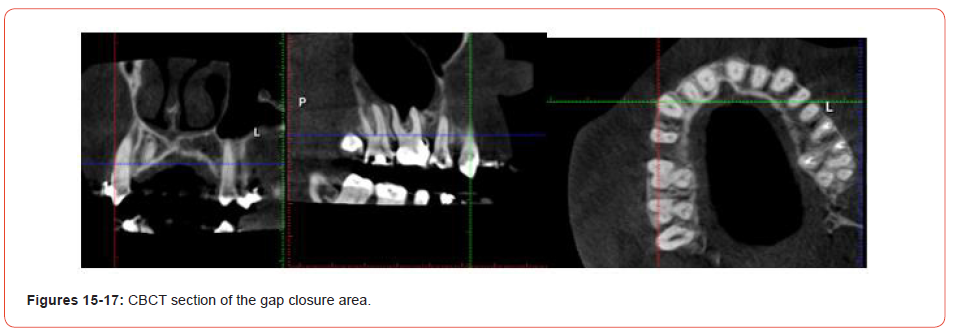
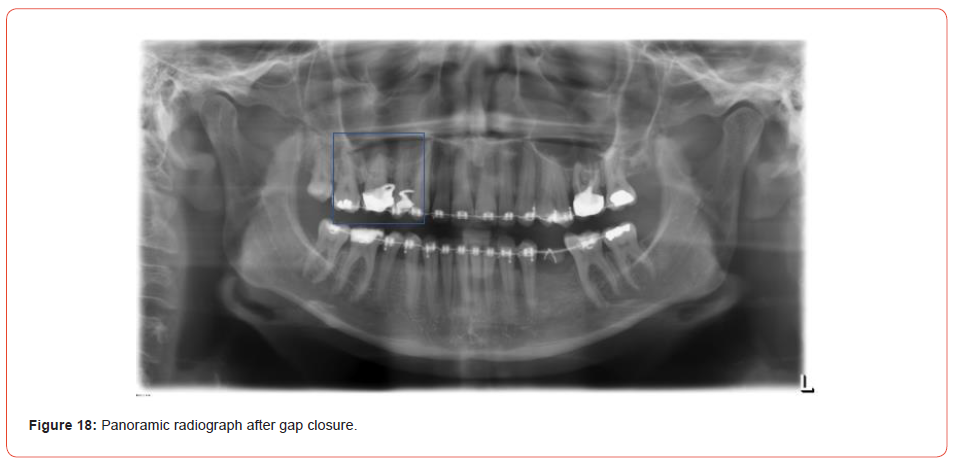
The mandibular teeth were aligned and uprighted, facilitating placement of an implant at site 35. The periodontal situation did not deteriorate. A Class I relationship in the canine region and a correct overbite and overjet were achieved on both sides. The facial profile improved thanks to the uprighting and proper torque of the anterior teeth (Figures 19-22).
Fixed retainers were bonded to the maxillary and mandibular
anteriors.
3D imaging with sagittal and axial superimpositions of
tooth movement proved that bodily tooth movement had been
successfully achieved (Figure 1).
Patient 2
Diagnosis
Patient 2 was a 46-year-old man with a skeletal Class II/1
dysgnathia (Figures 23-28).


Cephalometric tracing yielded the following results:
SNA angle: 87°
SNB angle: 84°
Sum of angles: 376°
Angle of Inclination, upper anteriors: 112°
Angle of Inclination, lower anteriors: 111°
(bialveolar protrusion)
The patient exhibited a full Class II malocclusion on the left side
and a Class II occlusion of one-quarter premolar width on the right
side.
Teeth 21, 16, 26 and 27 were missing. Tooth 45 was lingually
blocked. Tooth 15 exhibited a crossbite. Some periodontal bone loss
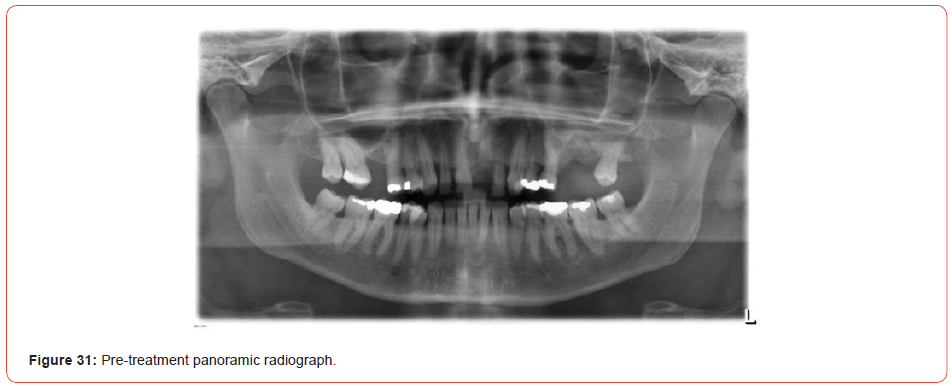
was visible in the radiographs (Figures 29-31).
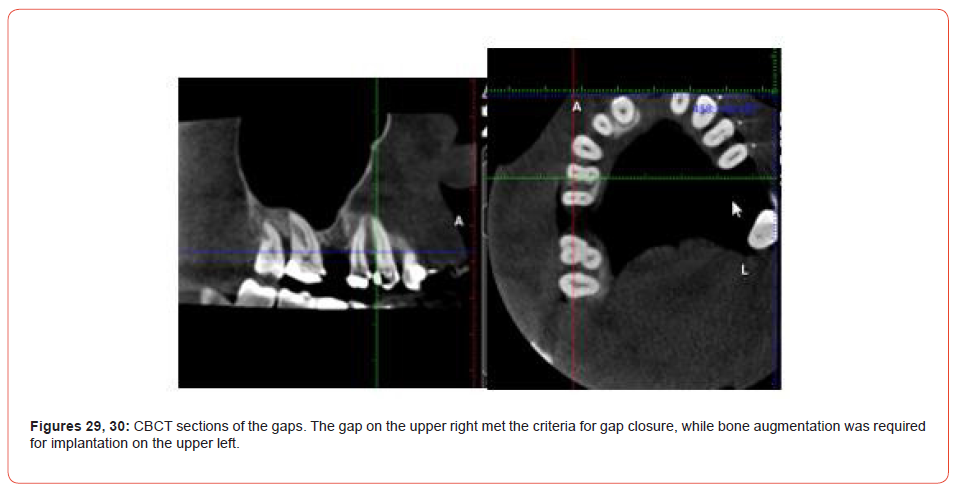
CBCT findings: The right maxillary gap side met the criteria
for gap closure, while the left maxillary gab required bone
augmentation and subsequent implant treatment.
Treatment objectives and treatment alternatives
1. Skeletal discrepancy to be compensated dentally
2. Gap closure on the maxillary right side through
mesialisation of the maxillary second and third molars and
distalisation of the premolars
3. Bone augmentation and implant placement on the
maxillary left side
4. Creation of a Class I occlusion
5. Correction of the sagittal and vertical overbites
6. Correcting the inclinations and torques of the anterior
teeth
7. Midline correction
8. Relieving the crowding and correcting the crossbite at
tooth 15
9. Uprighting of teeth 46 and 47
10. Aesthetics: Broadening the smile and improving the smile
curve
11. Periodontal: Slowing or halting progression of the existing
lesions
12. Achievement of long-term stability
Treatment procedures
Following professional tooth cleaning (sub- and supragingivally),
the teeth were aligned using a typical sequence of NiTi and
stainless-steel wires. To achieve gap closure on the maxillary right
side, custom lever arms were 3D-printed, and a mini-screw was
placed on the palate to provide stable anchorage for mesialisation
(Figures 32, 33). A sinus lift with bone augmentation (Guidor easygraft
Classic) was performed (Figures 8-12, 34, 35).

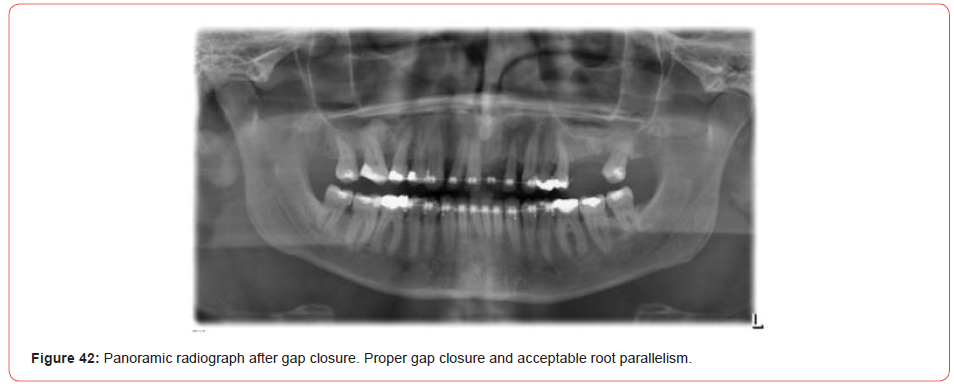
In the mandible, proximal stripping was performed to improve the inclination. Orthodontic tooth movements and gap closure was successfully performed. (Figures 36-38) illustrate the situation immediately after gap closure. The post-treatment radiographs (Figures 2, 39-42) show proper gap closure and acceptable root parallelism. The teeth were well aligned and uprighted. Orthodontic treatment was still in progress at the time of this writing.

Discussion
The floor of the maxillary sinus is similar to cortical bone in that it is a layer of compact bone lined with periosteal tissue. In adults, the size of the maxillary sinus is variable in its extension. Its floor extends between adjacent teeth or individual roots in about half of the population, creating elevations in the antral surface or protrusions of root tips into the sinus [13, 14].
Wehrbein and Diedrich [3] described a positive correlation between the length of root projection into the maxillary sinus as observed on panoramic radiographs and the amount of pneumatization that occurs after extraction. Sinus expansion following extraction can greatly decrease the amount of bone height available for implant placement. The relationship between the dental roots and the inferior sinus wall is known to influence orthodontic tooth movement, and the intrusion or bodily movement of teeth across the sinus floor that occurs with orthodontic treatment has been shown to cause moderate apical root resorption and a high degree of tipping [15].
The thickness of the inferior wall of the sinus and its relationship with the adjacent teeth is crucial for orthodontic tooth movement [4, 16]. This information provides a basis for the application of appropriate forces in orthodontic tooth movement and predicting the amount of tooth movement through the maxillary sinus. Augmentative techniques can facilitate tooth movement and a physical transmission of force leading to less tipping becomes possible, as illustrated by the cases presented here.
The treatment concept of bone augmentation consists of providing the bone with a stable osteoconductive structure that is gradually incorporated or replaced by the newly formed bone. Autologous bone grafts are considered the gold standard in bone regeneration surgery due to their osteoinductive potency [17, 18]. Synthetic materials consist mostly of β-TCP, a ceramic base that, depending on its surface texture, can have osteoconductive properties. Advantages of synthetic materials include their material characteristics and the reduced risk of allergies when bone augmentation is performed. The xenogeneic materials contain hydroxylapatite (HA) from animal bone or from algae and have a more complex three-dimensional structure offering improved osteoconductivity [19].
Bone augmentation materials should meet the following criteria for clinical use: scaffolding function to facilitate the ingrowth of bone cells from the surrounding graft (osteoconduction); support for growth factors or stem cells; surfaces for the migration, adhesion, differentiation and proliferation of cells; and stability to withstand the pressure of the covering soft tissue. Microporosities of at least 100μm to ensure the growth of blood vessels and pluripotent precursor cells and biocompatibility (not triggering any immune reaction) are important.
Among the most commonly used materials, HA and β-TCP have been successfully used for bone augmentation [20]. HA is considered almost a non-resorbable material and has the advantage that it serves as an osteoconductive scaffold for new bone formation. β-TCP, on the other hand, exhibits much greater biodegradability. To combine the positive aspects of the two calcium phosphates, biphasic materials with different ratios of HA and β-TCP have been developed [21-23].
The material used in the cases discussed here was Guidor easygraft Classic. Suitable for all dental applications requiring bone replacement, it is applied directly from the syringe into the defect, where it hardens and forms a porous but stable bone replacement. The fast-resorbable coating of polylactide ensures injectability, while the liquid Biolinker (N-methyl-2-pyrrolidone solution; Sunstar) promotes the mutual adhesion of the granules. The density of the coating is intended to prevent bacterial growth. The material as applied is characterised by high and interconnective porosity (and thus a haemostatic effect, promoting cell growth and bone formation) and forms a sticky mass. The size of the granules used in the study, of 450-1000μm is right for most medium-sized and large bone defects. The subsequent bone formation occurs simultaneously with the degradation of the filling material.
Roberts, et al. [24, 25] stated that modelling changes the size and shape of bones in response to mechanical loading, whereas remodelling is the turnover of bone that is related to bone maturation and mineral metabolism. Therefore, orthodontic tooth movement occurs as a result of a bone-modelling phenomenon, and the biologic balance of bone structures occurs by bone remodelling as a physiologic process.
Tooth movement through the maxillary sinus is another example of tooth movement through bone. In orthodontically induced tooth movement, the moving root is displaced in the cortical bone by frontal and undermining resorption. In this process, there is a balance between bone resorption and apposition in response to orthodontic forces. The modelling and remodelling mechanisms can readily adapt to changes in the mechanical loading of the alveolar bone.
Root resorption is associated with the removal of the necrotic material from the hyaline zone produced during the orthodontic tooth movement. The process is controlled by inflammation mediators. In this context, a distinction must be made between the treatment technique (type of appliance, duration of treatment, extent and type of tooth movement and size and type of force) and biological factors (innervation, abnormalities in bone density, inflammation, traumas and endodontic pre-treatments [26].
Tooth movement was successfully performed in both the cases presented here. In patient 2, For patient 2, dense structures could be seen in the radiographs, but no root resorption was observed.
The correlation between the topography of the maxillary sinus floor and related root position of posterior teeth using panoramic and cross-sectional computed tomography imaging was shown by Sharan and Madjar [27]. For most roots projecting into the sinus in panoramic radiographs, they report no vertical penetration into the sinus on CT images. Roots that did penetrate into the sinus on CT images exhibited much shorter penetration lengths than was apparent on panoramic radiographs.
Conclusion
Radiological and clinical evaluation of these two orthodontic cases showed successfully translational orthodontic tooth movement through an enlarged sinus supported by bone augmentation using a synthetic augmentation material. There were no significant signs of root resorption.
Acknowledgement
The authors wish to thank the patients for their willingness to publish this report and the company sunstar for providing the bone substitute material.
Conflict of interest
The authors report no conflict of interest.
References
- Kilic C, Kamburoglu K, Yuksel SP, Ozen T (2010) An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent 4(4): 462-467.
- Sharan A, Madjar D (2008) Maxillary sinus pneumatization following extractions: a radiographic study. Int J Oral Maxillofac Implants 23(1): 48-56.
- Wehrbein H, Diedrich P (1992) On the morphological initial situation in a basally pneumatized maxillary sinus - a radiological-histological study in humans [The initial morphological state in the basally pneumatized maxillary sinus--a radiological-histological study in man]. Fortschr Orthodontist 53(5): 254-262. German.
- Wehrbein H, Bauer W, Wessing G, Diedrich P (1990) The influence of the maxillary sinus floor on orthodontic tooth movement [The effect of the maxillary sinus floor on orthodontic tooth movement]. Advanced orthodontics 51(6): 345-351. German.
- Re S, Cardaropoli D, Corrente G, Abundo R (2001) Bodily tooth movement through the maxillary sinus with implant anchorage for single tooth replacement. Clin Orthod Res 4(3): 177-181.
- Hoogeveen EJ, Jansma J, Ren Y (2014) Surgically facilitated orthodontic treatment: a systematic review. Am J Orthod Dentofacial Orthop 145(4 Suppl): S51-64.
- Araújo MG, Carmagnola D, Berglundh T, Thilander B, Lindhe J (2001) Orthodontic movement in bone defects augmented with Bio-Oss. An experimental study in dogs. J Clin Periodontol 28(1): 73-80.
- Ahn HW, Lee DY, Park YG, Kim SH, Chung KR, et al. (2012) Accelerated decompensation of mandibular incisors in surgical skeletal class III patients by using augmented corticotomy: a preliminary study. Am J Orthod Dentofacial Orthop 142(2): 199-206.
- Coscia G, Coscia V, Peluso V, Addabbo F (2013) Augmented corticotomy combined with accelerated orthodontic forces in class III orthognathic patients: morphologic aspects of the mandibular anterior ridge with cone-beam computed tomography. J Oral Maxillofac Surg 71(10): 1760.e1-9.
- Reichert C, Wenghöfer M, Götz W, Jäger A (2011) Pilot study on orthodontic gap closure after guided bone regeneration. J Orofac Orthop 72(1): 45-50.
- Lee KB, Lee DY, Ahn HW, Kim SH, Kim EC, Roitman I (2014) Tooth movement out of the bony wall using augmented corticotomy with nonautogenous graft materials for bone regeneration. Biomed Res Int 2014: 347508.
- Sun W, Xia K, Huang X, Cen X, Liu Q, et al. (2018) Knowledge of orthodontic tooth movement through the maxillary sinus: a systematic review. BMC Oral Health 18(1): 91.
- Waite DE (1971) Maxillary sinus. Dent Clin North Am 15(2): 349-368.
- Hauman CH, Chandler NP, Tong DC (2002) Endodontic implications of the maxillary sinus: a review. Int Endod J 35(2): 127-141.
- Hallman M, Thor A (2008) Bone substitutes and growth factors as an alternative/complement to autogenous bone for grafting in implant dentistry. Periodontol 2000 47: 172-192.
- Kwak HH, Park HD, Yoon HR, Kang MK, Koh KS, et al. (2004) Topographic anatomy of the inferior wall of the maxillary sinus in Koreans. Int J Oral Maxillofac Surg 33(4): 382-388.
- Dumitrescu AL (2011) Chemicals in Surgical Periodontal Therapy. Chapter 2: Bone grafts and bone graft substitutes in periodontal therapy. Berlin and Heidelberg: Springer 73-144.
- Tonelli P, Duvina M, Barbato L, Biondi E, Nuti N, et al. (2011) Bone regeneration in dentistry. Clin Cases Miner Bone Metab 8(3): 24-28.
- Wildburger A, Payer M, Jakse N, Strunk D, Etchard-Liechtenstein N, Sauerbier S (2014) Impact of autogenous concentrated bone marrow aspirate on bone regeneration after sinus floor augmentation with a bovine bone substitute--a split-mouth pilot study. Clin Oral Implants Res 25(10): 1175-1181.
- Kurkcu M, Benlidayi ME, Cam B, Sertdemir Y (2012) Anorganic bovine-derived hydroxyapatite vs β-tricalcium phosphate in sinus augmentation: a comparative histomorphometric study. J Oral Implantol 38 Spec No: 519-526.
- Zhou AJ, Peel SA, Clokie CM (2007) An evaluation of hydroxyapatite and biphasic calcium phosphate in combination with Pluronic F127 and BMP on bone repair. J Craniofac Surg 18(6): 1264-1275.
- Leventis MD, Fairbairn P, Kakar A, Leventis AD, Margaritis V, et al. (2016) Minimally Invasive Alveolar Ridge Preservation Utilizing an In Situ Hardening β-Tricalcium Phosphate Bone Substitute: A Multicenter Case Series. Int J Dent 2016: 5406736.
- Spassova E, Gintenreiter S, Halwax E, Moser D, Schopper C, et al. (2007) Chemistry, ultrastructure and porosity of monophasic and biphasic bone forming materials derived from marine algae. Materials Science and Engineering 38(12): 1027-1034.
- Roberts WE, Huja S, Roberts JA (2004) Bone modelling: biomechanics, molecular mechanisms, and clinical perspectives. Seminars in Orthodontics 10: 123-161.
- Roberts WE (2006) Bone physiology of tooth movement, ankylosis, and osseointegration. Seminars in Orthodontics 6: 173-182.
- Reitan K (1967) Clinical and histologic observations on tooth movement during and after orthodontic treatment. Am J Orthod 53(10): 721-745.
- Sharan A, Madjar D (2006) Correlation between maxillary sinus floor topography and related root position of posterior teeth using panoramic and cross-sectional computed tomography imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102(3): 375-381.
-
Brigitte Wendl*, David Innerhofer, Margit Pichelmayer, Barbara Kirnbauer, Michael Payer and Norbert Jakse. A Novel Technique for Orthodontic Gap Closure with Access through the Maxillary Sinus. On J Dent & Oral Health. 6(1): 2022. OJDOH.MS.ID.000629. DOI: 10.33552/OJDOH.2022.06.000629.
-
Prosthetic restorations, Tooth movement, Orthodontic cases, Root resorption, Orthodontic gap, Sinus base, Soft tissue, Sphenoid bone, Dental arch, Maxillary sinus
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






