 Research Article
Research Article
Use of the Tool After the Lingual Frenulotomy to Improve the Strength, Range of Motion And Efficiency of the Tongue in the Myofascial Release Technique. A Case Report
Monika Izabela Osko1* and Jose Duran von Arx2
1DDS, Second Level University Master in Advanced Clinical Orthodontics, doctoral student at Barcelona University (Odontostomatology), Spain
2Retired professor with chair of orthodontics at Barcelona University, Spain
Monika Izabela Osko, DDS, Second Level University Master in Advanced Clinical Orthodontics, doctoral student at Barcelona University (Odontostomatology), Spain.
Received Date:February 26, 2024; Published Date:March 11, 2024
Abstract
Objective: The aim of this article is to present the application of the myofascial release technique (MRT) as a form of management after
frenulotomy, and to present the arguments for using such a technique of therapeutic treatment.
Materials and Methods: A 16-year-old patient came to the orthodontic surgery. The main problem was speech-language pathology- lack
of realization of the letter r and mouth breathing during sleep. The functional examination revealed limited mobility of the tongue against the
background of ankyloglossia. The treatment was based on using MFS stimulators: mouth obturator, nasal stimulator to restore nose breathing during
sleep and facilitate to obtain palate tongue resting position. A frenulotomy of the tongue frenulum was conducted and a therapy using the myofascial
release technique was used to improve the strength, mobility and articulation skills of the tongue. The tool was custom ordered by a medical tool
factory.
Results: After 11 months of postoperative therapy with the myofascial release technique, assisted by the night use of MFS stimulators, the
mobility, strength, resting position and speech-languages skills of the tongue were improved.
Conclusion: The use of the myofascial release technique with the tool after the frenulotomy procedure, improved the mobility, strength, length
and speech-languages skills of the tongue in a 16-year-old patient with ankyloglossia.
Keywords:IASTM; MRT; Tongue; Frenulum; Nose stimulator, Mouth obturator; Speech language pathology
Introduction
Instrumental Associated Soft Tissue Mobilization (IASTM) is a form of massage procedure, dedicated to soft tissues performed with the use of instruments. As a commonly known technique, it is used in orthopedics in the rehabilitation process [1, 2]. The available literature evidence shows that the clinical use of IASTM instruments for soft tissue mobilization is highly effective. They are credited with increasing the effectiveness of therapy in restoring strength [3], viscoelasticity, and muscle volume, as well as reducing the phenomenon of fibrosis in the tissue that binds muscles in the healing process. These effects are the result of microtrauma during the massage therapy with the tool. The microtrauma results in the production of: fibroblast growth factor FGF, hepatocyte growth factor HGF, which directly affect the metabolism and proliferation of the tissue subjected to the technique using IASTM tools. Microtrauma causes an inflammatory response, the synthesis of new collagen fibers and the synthesis of collagen and elastin by the newly formed fibroblast cells, resulting in the release of scar tissue and the mobilization of MCTmuscle connective tissue that penetrates, surrounds and connects the muscles called fascia [4-8]. The regenerative processes of connective tissue and muscles of the oro-facial area show a strong tendency to fibrosis after an injury. It is related to the ectodermal origin [9].
The term ankyloglossia is used to refer an autosomal inherited congenital anatomical anomaly [10], which Todd defines as an embryological tissue residue in the midline between the underside of the tongue and the inferior alveolar process [11] that restricts the mobility of the tongue varying degrees. It may be the result of: a mutation in the T-box genes [12, 13], the result of exposure to teratogenic substances during pregnancy [14], it can also be attributed to scar tissue after previous surgery or other trauma [15]. It can manifest itself in various clinical types, from a severe with a connected tongue to the floor of the mouth to a milder form with a short and thick lingual frenulum [16]. Ankyloglossia is found in newborns, infants, young children and adults. It causes the disturbance of the mobility of the tongue to a varying degree, depending on the degree of its severity. In some cases, ankyloglossia is not recognized despite existing functional problems. The authors opinions about the symptoms of ankyloglossia are divided. Some authors report that in most cases it is asymptomatic, while another group lists many disorders of the anatomical and oral cavity functions. From the point of view of the growth and development of the cranium, the acquisition of motor skills, the coordination of activities of the nasopharynx spaces: breathing and swallowing, progression of the path in acquiring the ability to take food of various consistency, texture, hardness, shape and size; changes in motor operations related to the intake of fluids and food, enriching and diversifying the diet, as well as shaping and speech-languages skills, require optimal tongue mobility and an appropriate range of tongue movements. This movement can be altered by mobilityrestricted muscles and fasciae. The muscles of the tongue in patients with ankyloglossia are limited in mobility due to the shortened sublingual frenulum [17-19, 2, 20-27].
Appropriate tongue strength is essential for the oral motor skills, speech-languages skills and pharyngeal phases of swallowing and contributes to the formation, placement, and manipulation of a bolus within the oral cavity and propulsion into the pharynx [28]. It was determined that the IOPI is reliable for the measurement of tongue strength [29].
Materials and Methods
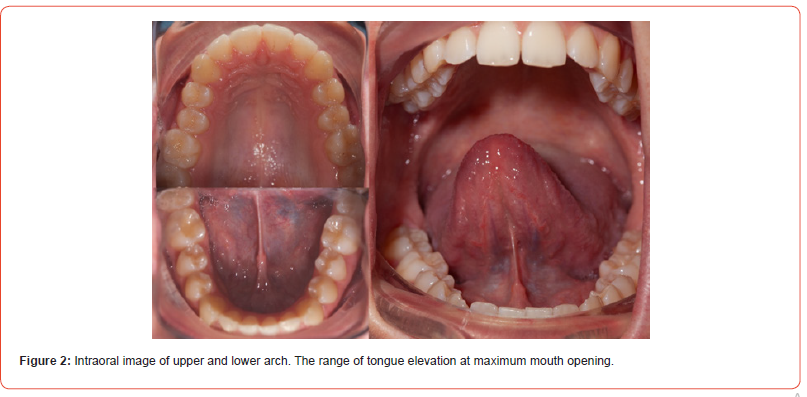
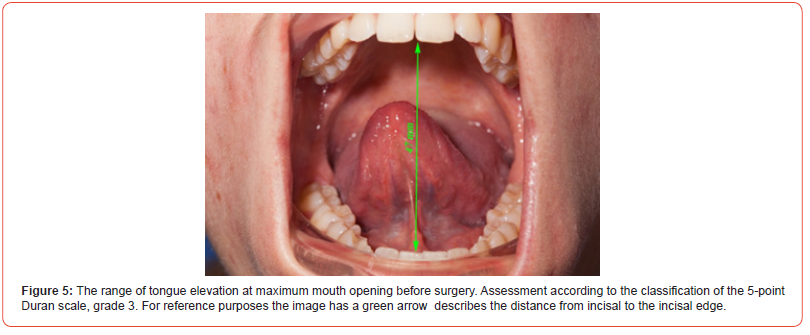
A 16-year-old patient came to the surgery for consultation. The main problem was speech-languages pathology- the lack of realization of the letter r and the disturbance of the mouth posture during sleep. The functional examination revealed limited mobility of the tongue. The range of tongue elevation on the Duran 5-point scale [30] at the maximum opening of the mouth was half the value of the maximum opening of the maxilla in relation to the mandibleassessed according to the classification as mobility No. 3. Dentally, Angle class I occlusion on both sides was stated. Overbite of 4 mm, overjet of 1.5mm The parabolic shape of the upper dental arche, in the area of premolars, the dental arche was narrowed. A similar situation occurred in the lower arch [Fig. 1, Fig. 2]. Palatine tonsils not exceeding the border of the palatine arches, uvula and soft palate, Mallampati grade I. The swallowing skills were examined, during which no additional facial muscle movements were noted. The value of negative pressure generated inside the mouth were examined by use IOPI medical device, value 33 was examined. The interview with the patient and her mother determined: term delivery by caesarean section with an Apgar score of 7 points, the score was reduced for respiratory function, muscle tone and skin color (by 1 point for each parameter), breastfeeding up to 1 year of age. During feeding, quick fatigue and falling asleep, reluctant consumption of food from the bottle, better results were obtained by feeding with a spoon, which was introduced at 5 months of age. Sucking on a pacifier up to 1.5 years of age. From the age of 3.5 years otitis media occurred three times, alternating between right and left, ended with ear drainage and tonsillectomy. The drains were in the ears for 8 months. In the period from 3.5 to 4.5 years of age breathing through the oral path.
The course of myotherapy to improve the tone of the orbicular muscle of the mouth lasted for a year. After this period, the patient was breathing through the nasal passages during the day and no attention was paid to it at night.
Since the age of 5, she has not had an ear infection again, and on average she had upper respiratory tract infections once a year. X-ray pantomographic image was taken [Fig. 3].


The Following treatment was proposed
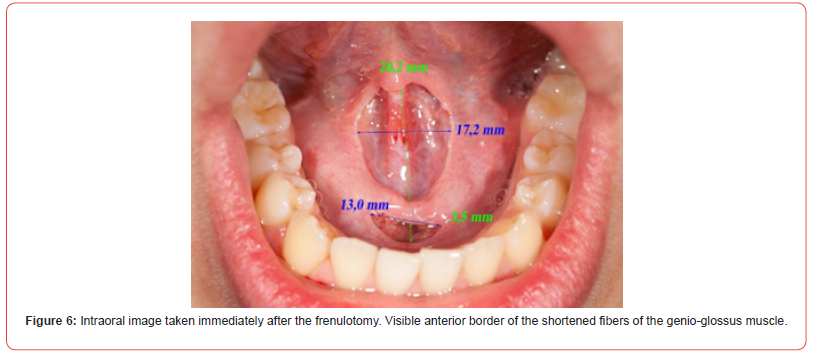
1. Frenulotomy of the tongue frenulum [Fig. 6 ]
2. Continuously, use a tongue exercises and myofascial
release techniques (MRT) as part of the therapeutic process
aimed at improving the mobility and strength of the
tongue, establishing a resting position on the palate. It was
recommended to start a tongue exercises 6 hours after the
frenulotomy and the exercises in (MRT) technique 1 month
after the frenulotomy, 3 times a week for about 10 minutes.
3. Night use of MFS stimulators: the mouth obturator to
improve the tone of the orbicular muscle of the mouth and
serve as isolation to prevent mouth breathing and to create
negative pressure conditions inside the mouth to facilitate the
positioning of the tongue on the palate. Use of a nasal stimulator
to increase airflow through the nostrils.
4. Work on improving speech-languages skills. The patient
and the patient’s mother accepted the proposed treatment plan.
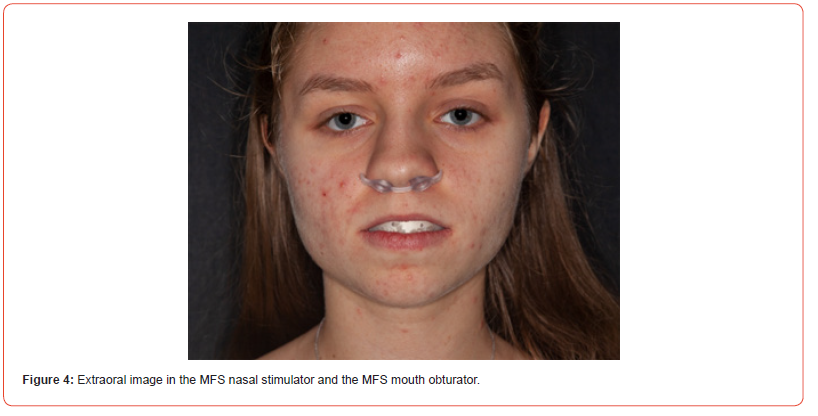
The nasal stimulator and the mouth obturator were selected
during the same visit , Fig. 4. The use of stimulators at night
was recommended.
The frenulotomy procedure was scheduled 14 days after the consultation visit. In order to prepare the area of the bottom of the mouth for the procedure, the patient was asked to do the recommended exercises. The frenulotomy was operated using electrocoagulation in cutting mode without coagulation on low current parameters.
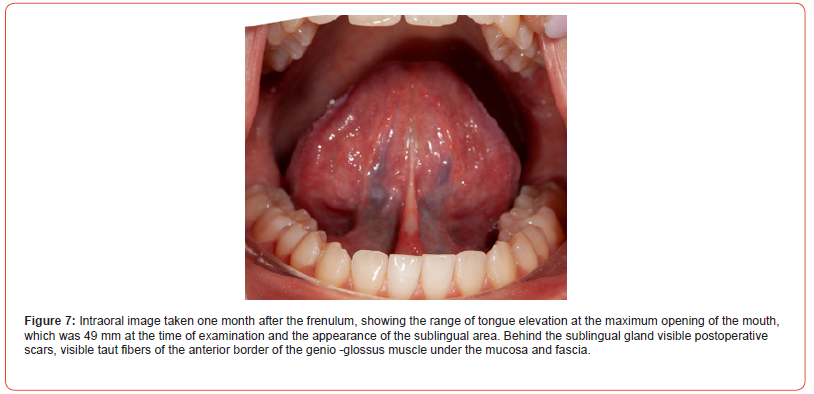
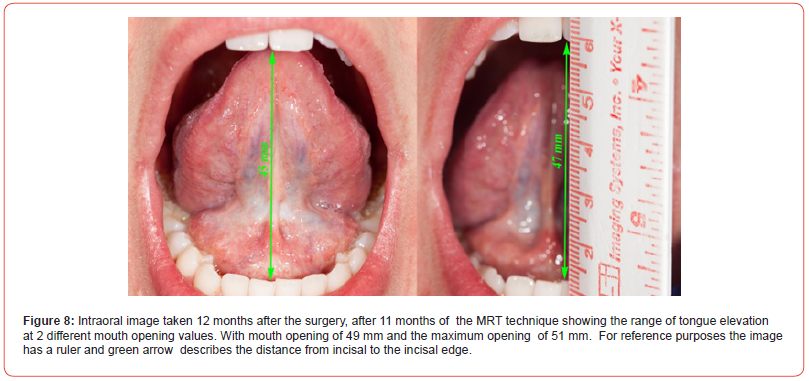
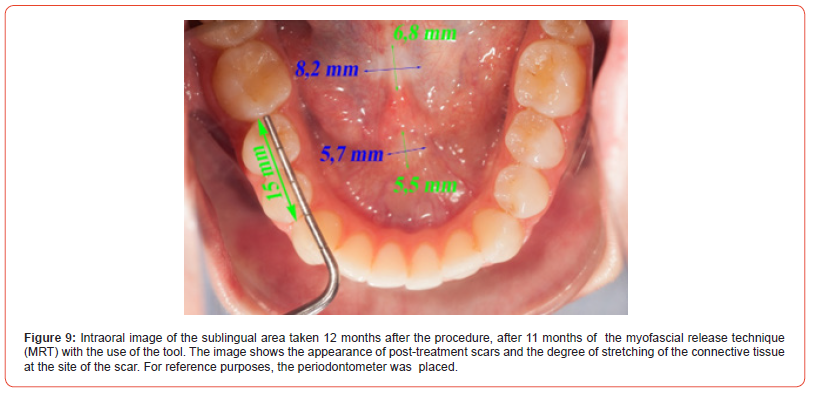
The myofascial release techniques MRT was performed by the patient on her own according to the recommendations of 3 exercises three times a week for about 10 minutes. First, it was recommended to perform the exercise using a narrower and later wider part of the tool in a longitudinal plane, moving from distal to proximal along the length of the genio-glossus muscle. It was recommended to perform the exercise on right and left sides of the tongue, an equal number of repetitions. The second exercise was to perform the exercise in a longitudinal plane, moving distal to proximal and proximal to distal along the length of the genio-glossus muscle at the site of the postoperative scar. As the third exercise, it was recommended to apply pressure at the base of the tongue to the inside of the oral cavity, and the patient used his tongue to push wider part of the tool in the opposite direction. It was recommended to perform pressure with force on the border of pain. Safety and effectiveness were assessed before the procedure, immediately after the procedure, and after the first, sixth and twelfth month after the procedure. The mobility of the tongue, the value of negative pressure generated inside the mouth and signs of myofascial tension were examined by means of the assessment of tongue mobility according to Duran, a comparative study assessing the value of negative pressure generated inside the oral cavity was assessed using an IOPI device for measuring negative pressure inside the oral cavity. The size of the postoperative scar was assessed on the basis of the analysis of the intraoral image taken one month after the procedure and in the subsequent measurement months. In the therapeutic process, great emphasis was also placed on learning to position the tongue on the palate.
The therapeutic management after the frenulotomy of the lingual frenulum was exercised using a stainless steel tool designed for this purpose, made by a medical instrument factory.
Results
There were no complications after the frenulotomy, postoperative bleeding was limited to a few minutes after the procedure. Postoperative pain causing difficulties in tongue movements and shifting food with the tongue persisted until the third day after the procedure. In the following days, up to a week, the condition was defined by the patient as discomfort, but it did not cause pain when moving the tongue and maintaining the resting position of the tongue. On the day of the procedure, immediately after the procedure, the tongue lift was assessed. In this assessment, the range of tongue lifting ranged between the first and the second on the Duran scale for tongue mobility. Following assessment of the mobility range of the tongue was made one month after the procedure, and then 6 months and 12 months after the procedure. Ultimately, an improvement in the mobility of the tongue, an improvement in the value of the negative pressure generated inside the oral cavity, the relaxation of the fascia of the bottom of the oral cavity, and the expansion of the mucosa area covering the genioglossus muscle constituting the area of the postoperative scar, were achieved. These values were obtained successively in the following months of exercising. Ultimately, 12 months after the surgery, the pronunciation of the isolated consonant r and the isolated words with “r” with a distinct vibration of the front part of the tongue were improved. In order to apply the acquired speech-languages skills in the pronunciation of the consonant “r” in everyday speech. Speech therapy and language exercises have been performed to acquire these skills.
The postoperative therapeutic management in the first month
after the procedure included:
1. Pressure on the extreme edges of the wound on both
sides.
2. Pressure on the tip of the tongue from the bottom of the
mouth with the tip of the tongue pointing towards the throat.
3. Sliding the finger once on the right and once on the left
side between the alveolar process and the lateral edge of the
tongue with the tongue lifting.
4. Sucking the tongue towards the roof of the mouth, then
(without lifting the tongue from the roof of the mouth, opening
and closing the mouth).
5. With the jaws open to the maximum, trying to touch the
last molars in the maxilla and the mandible with the tip of the
tongue.
6. Moving the tongue from one side of the mouth to the other
without moving the lower jaw.

Table 1:
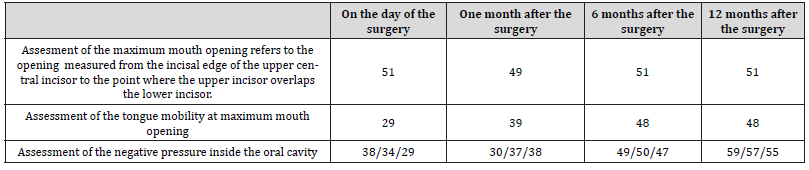
A table presenting a comparison of maximum opening of the mouth, the mobility of the tongue and the value of negative pressure generated inside the mouth in the IOPI test on the day of the procedure, after 1, 6 and 12 months after the procedure.
Discussion
The architectural design of the bottom of the oral fascia as a “diaphragm” or diaphragm-like structure attached around the mandibular arch ensures the suspension and stability of the tongue in the oral cavity. The fascial dimensions of a person’s floor of the mouth affect the range of motion of the tongue. The tongue is mobilized in the mouth by contraction of the external and internal muscles of the tongue. The relaxation in the fascial layer of the floor of the mouth allows a wide range of tongue movement before the fascia is tightened, potentially affecting the “end point” of the range of tongue movement. Ankyloglossia can be considered an imbalance of fascial roles, which affects the mobility of the tongue [31, 32]. Surgical intervention to improve the mobility of the tongue makes sense when we can count on the effectiveness of this intervention. The wound healing process always leads to the formation of a scar and its shrinkage. Shrinking sometimes leads to distortion and even restricts the range of motion. The nature of the wound matrix changes as the scar remodels. The immature scar contains a disorganized system of fine collagen fibers, which is gradually replaced by thicker fibers arranged in an orientation corresponding to the tensions acting on them. At the same time, the granulation tissue begins to fill the wound. Granulation tissue is used to regenerate connective tissue. It does this by migrating new blood into the area and forming a matrix of fibers that are precursors to scar formation. It may take months to form a mature wound. During this time, the wound contracts as the scar fibers organize. Frenulotomy is performed in order to improve the mobility of the tongue, while “injury, trauma, even microtrauma, can cause scarring that changes the properties of coenergic tissues” [33].
According to the researchers Salazar, Monroy, Wagener, and Hoff, improving regeneration in the orofacial region should focus on reducing fibrosis, and therapeutic strategies after orofacial procedures. They should include antifibrotic agents, as well as growth factors stimulating satellite cell differentiation, such as FGF ( fibroblast growth factor) and HGF (hepatocyte growth factor) [34]. A muscle with limited mobility limits the strength of the tongue and the range of motion. the tongue, as a transversely striated muscle, is characterized by the possibility of generating a certain force, which, as tested in an adult (IOPI device), amounts to an average of 53 kPa [29]. After releasing the tongue through the frenulotomy procedure, in order to increase the strength of the tongue in a situation of reduced strength, the tongue should be trained in terms of the force generated. The MRT technique seems to be innovative in this area of the body. It was shown on the example of a patient that it gives results in improving the efficiency, mobility. Speechlanguages skills and strength of the tongue.
Conclusion
Achieving positive results in improving the mobility of the tongue and preventing scar formation is possible thanks to the use of the myofascial release technique with the use of a tool. It can be an effective method in restoring the mobility of the tongue after frenulotomy, in counteracting the negative effects of scarring, restoring, among others, mobility, strength, length, viscoelasticity, muscle volume. From the point of view of the growth and development of the cranium, the acquisition of motor skills, the coordination of activities of the primary nasopharynx spaces: breathing and swallowing. The progression of the path in acquiring food intake skills and the development of speech-languages skills require optimal tongue mobility and an appropriate range of tongue movements. This movement can be altered by mobility-restricted muscles and fasciae. The tool, technique, frequency and duration of therapy in post frenulotomy treatment procedings with the use of the tool was developed based on the literature. The results obtained by researchers using the IASTM in literature technique were taken into account. Exercise no. 3 it has been developed on the basis of physiotherapeutic rehabilitation techniques used in restoring the: strength, length, mobility and viscoelasticity of the tongue [7, 8, 35, 36].
Acknowledgement
Thanks to the patient for perfect cooperation during therapy and for providing the image.
Conflict of Interest
No conflict of interest.
References
- Sevier TL, Gehlsen GM, Wilson JK, Stover SA, Helfst RH (1995) Traditional physical therapy vs. graston augmented soft tissue mobilization in the treatment of lateral epicondylitis. Medicine & Science in Sports & Exercise 27(5): 52.
- Segal LM, Stephenson R, Dawes M, Feldman P (2007) Prevalence, diagnosis, and treatment of ankyloglossia: methodologic review. Can Fam Physician 53: 1027-1033.
- Hammer W l (2008) The effect of mechanical load on degenerated soft tissue. J Bodyw Mov Ther 12: 246-256.
- Burke J, Buchberger DJ, Carey Loghmani MT, Dougherty PE, Greco DS, et al. (2007) Journal of Manipulative and Physiological Therapeutics 30(l): 50-61.
- Melham TJ, Sevier TL, Malnofski MJ, Wilson JK, Helfst RH (1998) Chronic ankle pain and fibrosis successfully treated with a new noninvasive augmented soft tissue mobilization technique(ATSM): A case report. Med Sci Sports Exerc 30(6): 801-804.
- Stow R (20ll) Instrument-assisted soft tissue mobilization. International journal of athletic therapy & training 16(3): 5-8.
- Davidson CJ, Ganion LR, Gehlsen GM, Verhoestra B, Roepke JE, et al. (1997) Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc 29(3): 3I3-319.
- Gehlsen GM, Ganion L, Helfst R (1999) Fibroblast Responses to Variation in Soft Tissue Mobilization Pressure. Med Sci Sports Exerc 31(4): 531-535.
- Sefton EM, Kardon G (2019) Connecting muscle development, birth defects, and evolution: An essential role for muscle connective tissue. Curr Top Dev Biol 132: 137-176.
- Klockars T, Pitkäranta A (2009) Inheritance of ankyloglossia (tongue-tie). Clinical Genetics 75: 98-99.
- T Hogan (2015) Tongue tie in newborn: Early diagnosis and division prevents poor breast feeding outcomes. Breastfeeding review 23(1): 11-16.
- Braybrook C, Lisgo S, Doudney K (2002) Craniofacial expression of human and murine TBX22 correlates with the cleft palate and ankyloglossia phenotype. Hum Mol Genet.
- Herr A, Meunier D, Müller I (2003) Expression of mouse Tbx22 supports its role in palatogenesis and glossogenesis. Dev Dyn 226: 579-586.
- Morita H, Mazerbourg S, Bouley DM (2004) Neonatal lethality of LGR5 null mice is associated with ankyloglossia and gastrointestinal distension. Mol Cell Biol 24: 9736-9743.
- Horton CE, Crawford HH, Adamson JE, Ashbell TS (1969) Tongue‐tie. The Cleft Palate-Craniofacial Journal 6: 8-23.
- Chu MW, Bloom DC (2009) Posterior ankyloglossia: a case report. Int J Pediatr Otorhinolaryngol 73: 88-883.
- Lalakea ML, Messner AH (2003) Ankyloglossia: does it matter? Pediatr Clin North Am 50: 381-397.
- Martinelli RL, Marchesan IQ, Gusmão RJ, Honório HM, Berretin Felix G ( 2015) The effects of frenotomy on breastfeeding. J Appl Oral Sci 23: 153-157.
- Hogan M, Westcott C, Griffiths M (2005) Randomized, controlled trial of division of tongue-tie in infants with feeding problems. Journal of Paediatrics and Child Health 41: 246-250.
- Mukai S, Mukai C, Asaoka K (1991) Ankyloglossia with deviation of the epiglottis and larynx. Ann Otol Rhinol Laryngol 153: 3-20.
- Mukai S, Mukai C, Asaoka K (1993) Congenital ankyloglossia with deviation of the epiglottis and larynx: Symptoms and respiratory function in adults. Ann Otol Rhinol Laryngol 102: 620-624.
- Wright J (1995) Tongue-tie. Journal of Paediatrics and Child Health 31: 276-278.
- Sánchez Ruiz I, González Landa G, Pérez González V (1999) Section of the sublingual frenulum. Are the indications correct? Cir Pediatr 12: 161-164.
- Peng CL, Jost Brinkmann PG, Yoshida N, Chou HH, Lin CT (2004) Comparison of tongue functions between mature and tongue-thrust swallowing: an ultrasound investigation. Am J Orthod Dentofacial Orthop 125: 562-570.
- Chia Fen C, Chien Lun P, Hung Yi C, Chi Yang T (2002) Dentofacial morphology and tongue function during swallowing. Am J Orthod Dentofacial Orthop 122(5): 191-199.
- Messner AH, Lalakea ML, Aby J, Macmahon J, Bair E ( 2000) Ankyloglossia: Incidence and associated feeding difficulties. Arch Otolaryngol Head Neck Surg 126: 36-39.
- Jang SJ, Cha BK, Ngan P, Choi DS, Lee SK, et al. (2011) Relationship between the lingual frenulum and craniofacial morphology in adults. Am J Orthod Dentofacial Orthop 139: 361-367.
- Youmans S, Stierwalt JAG (2006) Measures of tongue function related to normal swallowing. Dysphagia 21(2): 102-111.
- Adams V, Baines SK, Mathisen BA, Lazarus CL (2013) Reliability of Measurements of Tongue and Hand Strength and Endurance Using the Iowa Oral Performance Instrument with Healthy Adults. Dysphagia 29(1): 83-95.
- Duran Von Arx J(2010) Stimulotherapy in orthodontics, Etiopathogenic and Recurrence Control. Ripano Ed I, p. 83.
- Mills N, Pransky SM, Geddes DT, Mirjalili SA (2019) What is a Tongue Tie? Defining the anatomy of the in-situ lingual frenulum. Clin Anat 32: 749-761.
- Mills N, Keough N, Geddes DT, Pransky SM, Mirjalili SA (2019) Defining the anatomy of the neonatal lingual frenulum. Clin Anat 32(6): 824-835.
- Jarvinen T, Kariainen M, Kalimo H, Jarvinen M (2005) Muscle injuries: Biology and treatment. Am J Sports Med 33(5): 745-766.
- Rosero Salazar DH, Carvajal Monroy P, Wagener FADTG, Von den Hoff JW (2020) Orofacial Muscles: Embryonic Development and Regeneration after Injury. J Dent Res 99(2): 125-132.
- Meyers TW (2014) Anatomical tapes. DB Publishing. (edn. III), 232,233,234.
- Sevier TL, Wilson JK (1999) Treating lateral epicondylitis. Sports Medicine 28(5): 375-380.
-
Monika Izabela Osko* and Jose Duran von Arx. Use of the Tool After the Lingual Frenulotomy to Improve the Strength, Range of Motion And Efficiency of the Tongue in the Myofascial Release Technique. A Case Report. On J Dent & Oral Health. 7(5): 2024. OJDOH.MS.ID.000671.
-
Mouth, Tongue, Oral cavity, Orofacial procedures, IASTM technique, Mature wound, lower jaw, Maxilla, Throat
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






