 Case Report
Case Report
Management of Dental Implant in Mandibular Idiopathic Osteosclerosis: A Case Report
Yiying Zhu DDS, PhD1, Chenxin Wang DDS, PhD2 and Si Chen, DDS, PhD1*
1Resident, Department of Implantology, Shanghai Stomatological Hospital, Fudan University & Shanghai Key Laboratory of Craniomaxillofacial Development and Diseases, Fudan University, China
2Resident, Department of Orthodontics, Shanghai Stomatological Hospital, Fudan University & Shanghai Key Laboratory of Craniomaxillofacial Development and Diseases, Fudan University, China
Dr. Si Chen, Department of Implantology, Shanghai Stomatological Hospital, Fudan University 356 East Beijing Road, Huangpu, Shanghai, 200001, PR China.
Received Date:December 11, 2023; Published Date:January 19, 2024
Abstract
Idiopathic osteosclerosis (IO) is a high-density lesion frequently found in the mandibular alveolar bone, but few cases have been reporte to describe approaches to dental implant treatment. This clinical report describes a successful implant restoration for a 25-year-old man with IO in the right mandibular bone which followed up for 23 months. Moreover, histological examinations, including HE, Masson, and immunohistochemistry staining, were further performed to investigate the micromorphology of IO tissues. Finally, the operative strategies are concluded according to the case report and the microstructures. This article provides an effective therapeutic experience for dental implant treatment with IO.
Introduction
Idiopathic osteosclerosis (IO), also called osteosclerosis, enostosis or dense bone island, is a common intrabony radiopaque lesion with an estimated prevalence of 3%-6% [1, 2]. As a localized lesion with different shapes and sizes, IO is mainly located in the mandibular premolar and molar areas, single or multiple, and is characterized by an increased bone density. IO is often discovered through an incidental X-ray examination, exhibiting a uniform highdensity block mass that can be close to or far from the tooth roots [3, 4]. Surrounded by normal bone, IO has a well-defined margin but no capsule, which may be difficult to distinguish from some cases of condensing osteitis or alveolar bone inflammation caused by periapical periodontitis [5].
In most cases, IO is clinically asymptomatic with no need for specific treatment, but it has a certain influence on implant therapy when found in edentulous areas. Osseointegration plays an essential role in the clinical success of implants. During the process of osseointegration, the blood clot is replaced by granulation tissue, and mesenchymal cells start to differentiate. Newly formed vascular structures and woven bone promote the establishment of mature osseointegration [6]. The histological characteristics and osseointegration process in normal bone tissues have been thoroughly investigated; however, few reports on the histological characteristics of IO are available in the literature. Meanwhile, clinical experience in dealing with IO in implant therapy is rarely mentioned. This case shows how we managed implant therapy in a mandibular IO area. Moreover, a clinical biopsy was obtained to investigate the histological morphology of the IO tissues.
Case Report
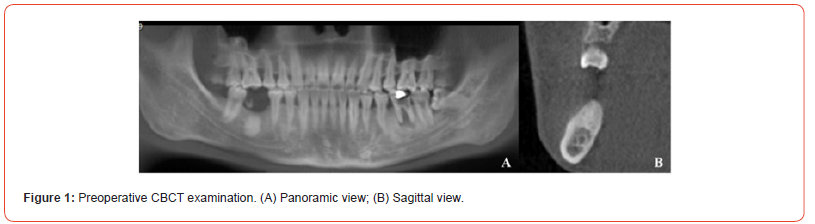
A 25-year-old man with loss of the right mandibular first molar was referred to the Department of Implantology at Shanghai Stomatological Hospital seeking implant-supported restorations. He reported no systematic diseases and no use of drugs. The clinical examination revealed the loss of the right mandibular molar. The buccal alveolar bone was moderately absorbed. His oral hygiene was poor with dental calculus. Cone beam computed tomography (CBCT) showed a high-density mass under the alveolar crest located at the ideal implant site, 7.86×11.48mm in size, extending to the buccal-lingual bone plate (Figure 1).
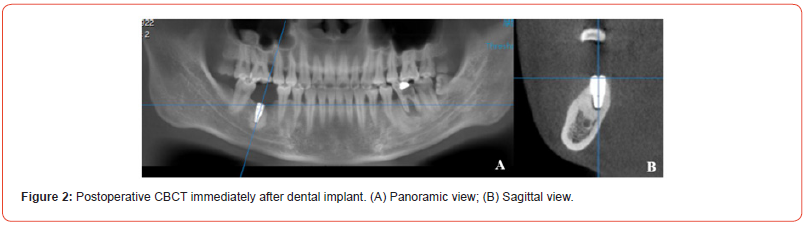
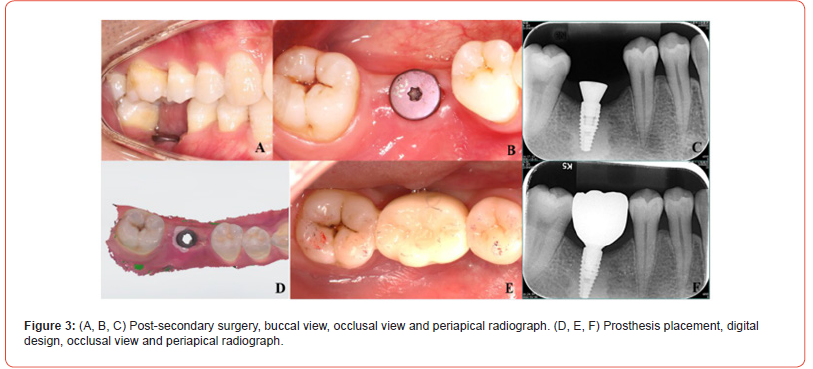
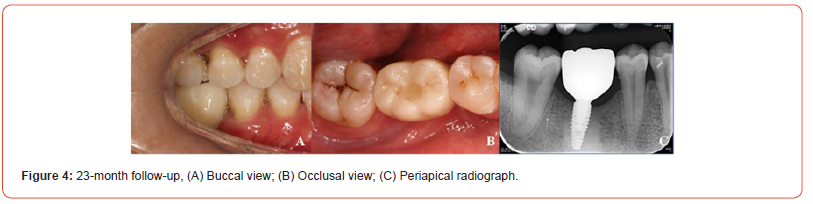
Implant surgery was performed after periodontal treatment. A brand new Straumann surgical instrument was used for better bone preparation. Graded drilling ensured proper implant positioning and spacing while avoiding overheating. Cold normal saline was additionally applied around the surgery site to reduce heat production. An implant (Bone Level Tapered; 4.1 mm×10 mm; Institut Straumann AG) was placed after thread tapping (Figure 2). The insertion torque was 80 N·cm. The secondary surgery was completed 3 months later, with no evident marginal bone loss, and the ceramic crown was placed using intraoral scanning and the CAD/CAM technique (Figure 3). At the 23-month follow-up, the implant functioned normally, and the marginal bone remained stable (Figure 4).
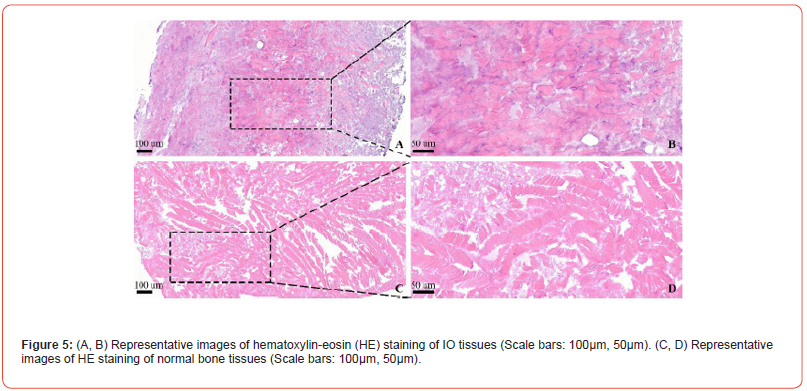
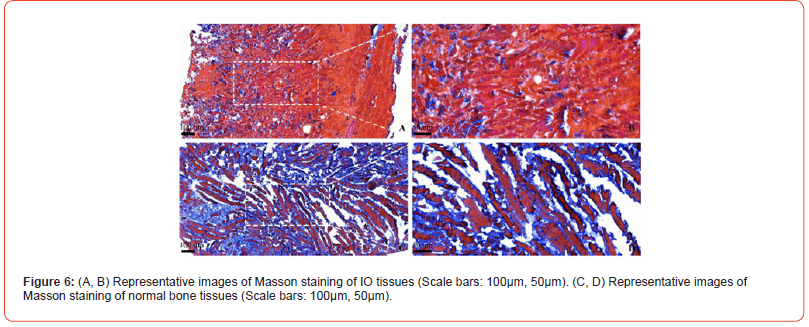
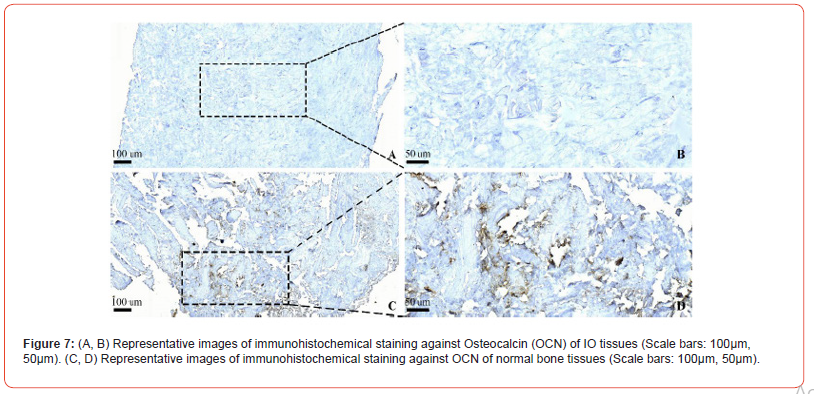
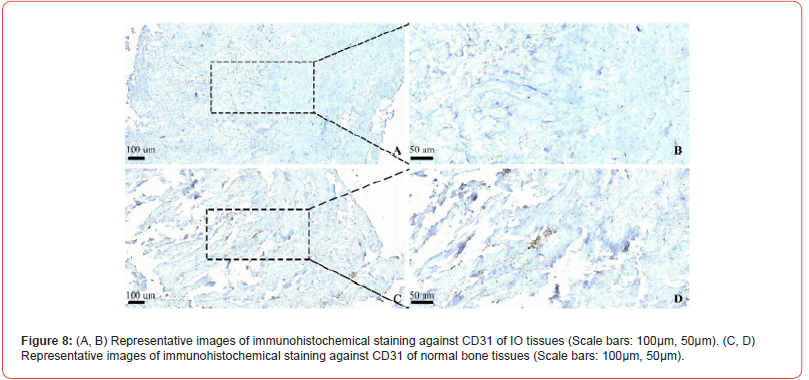
During the operation to place the implant, a biopsy was taken from the graded drilling. The bone tissues were decalcified by 10% EDTA for histological analysis. Hematoxylin-eosin (HE) staining showed that the IO tissues had few osteocytes, osteoblasts and osteoclasts, mainly just lamellar bone, which was regular and closely arranged, while the normal bone tissues had more trabecular structures, fibers, osteoblasts and osteoclasts (Figure 5). Masson staining revealed that the mature bone-derived IO tissues included fewer dark blue-stained collagen fibers than the normal bone (Figure 6). Moreover, immunohistochemical (IHC) staining for osteocalcin (OCN) and CD31 was conducted to investigate the distribution of the osteoblasts and vascular tissues. OCN was expressed in normal bone but not in IO tissues, confirming that the IO tissues contained very few osteoblasts (Figure 7). Similar results were observed for CD31, with few CD31-positive cells observed in the IO tissues (Figure 8).
Discussion
IO has no known etiology. Most lesions are stable in size, while in some cases, the lesions will diminish or disappear. In this case, as the patient insisted, we designed detailed procedures and performed a biopsy. Histopathological examination confirmed the diagnosis. The tissue sections revealed thick dense bone filling the IO region. Osteoblastic rimming of the bony masses was not detected. Collagen fibers and other vascular tissues were rarely seen. There were no inflammatory cells.
Predicting implant success is an inherently difficult challenge. Usually, better bone-to-implant contact develops over time in implants placed in more dense bone; however, the bone density of IO is much higher than that of normal bone [7, 8]. Bones such as type III bone with great regenerative potential are prone to form osseointegration. Type Ⅰ bone is considered to have less potential for cell proliferation and mineralization [9]. This case indicates that high-density bone may also achieve good osseointegration. It is presumed that a fully bonded interface is appropriate for achieving interlocking between the thread and lamellar bone. The initial stability of the implant is essential for successful osseointegration [10].
An IO lesion is composed of dense bone. Four operative strategies are concluded according to the case report and the microstructures. Firstly, using a brand new instrument. During oral surgical bone preparation, there is a direct correlation between drill wear and intraosseous temperatures [11]. Therefore, it is necessary to use new instruments to ensure quick intraoperative drilling and low temperatures. Secondly, auxiliary cooling when preparing the alveolar bone. Adequate irrigation with cold water also plays a significant role in keeping the intraosseous temperature down [12]. Thirdly, over preparation slightly to reduce the insertion torque. Last but not least, designment of the implant. The implant size should be appropriately reduced within a safe range to reduce insertion torque, and a self-tapping implant with tapered design is favored [13]. Following the above operation strategies, the implant in the IO region with a functional prosthesis worked well in the present case.
In conclusion, the implant placed in idiopathic osteosclerosis successfully restored function in this case. Characterized with thick dense bone with little collagen fibers, idiopathic osteosclerosis exhibits little mature osteoblasts and vascular tissues. Reduced heat production, sufficient or even over bone preparation, and application of self-tapping implants are the keys to success.
Acknowledgement
The authors thank the patient for his understanding and cooperation.
Conflict of Interest
The authors declare no conflict of interest.
References
- Sisman Y, Ertas ET, Ertas, H, Sekerci AE (2011) The frequency and distribution of idiopathic osteosclerosis of the jaw. Eur J Dent 5(4): 409-414.
- Naser AZ, Roshanzamir N (2016) Prevalence of idiopathic osteosclerosis in an Iranian population. Indian J Dent Res 27(5): 544-546.
- Moshefeghi M, Azimi F, Anvari M (2014) Radiologic assessment and frequency of idiopathic osteosclerosis of jawbones: an interpopulation comparison. Acta Radiol 55(10): 1239-1244.
- McDonnell D (1993) Dense bone island: A review of 107 patients. Oral Surg Oral Med Oral Pathol 76: 124-128.
- Ledesma Montes, C, Jiménez Farfán, MD, Hernández-Guerrero, JC. (2019) Idiopathic osteosclerosis in the maxillomandibular area. Radiol Med 124: 27-33.
- Salvi GE, Bosshardt DD, Lang NP, Abrahamsson I, Berglundh T, et al. (2015) Temporal sequence of hard and soft tissue healing around titanium dental implants. Periodontol 2000 68: 135-152.
- Molly L (2006) Bone density and primary stability in implant therapy. Clin Oral Implants Res 17: 124-135.
- Wirth AJ, Goldhahn J, Flaig C, Arbenz P, Müller R, et al. (2011) Implant stability is affected by local bone microstructural quality. Bone 49: 473-478.
- Li J, Yin X, Huang L, Mouraret S, Brunski JB, et al. (2017) Relationships among bone quality, implant osseointegration, and Wnt signaling. J Dent Res 96: 822-831.
- Qu C, Luo F, Hong G, Wan Q (2021) Effects of platelet concentrates on implant stability and marginal bone loss: a systematic review and meta-analysis. BMC Oral Health 21(1): 579.
- Szalma J, Klein O, Lovász BV, Lempel E, Jeges S, et al. (2018) Recommended drilling parameters of tungsten carbide round drills for the most optimal bone removal in oral surgery. Biomed Res Int 2018: 3108581.
- Augustin G, Davila S, Udilljak T, Staroveski T, Brezak D, et al. (2012) Temperature changes during cortical bone drilling with a newly designed step drill and an internally cooled drill. Int Orthop 36: 1449-1456.
- Benca E, Ferrante B, Zalaudek M, Hirtler L, Synek A, et al. (2021) Thermal effects during bone preparation and insertion of osseointegrated transfemoral implants. Sensors (Basel) 21(18): 6267.
-
Yiying Zhu DDS, PhD, Chenxin Wang DDS, PhD and Si Chen, DDS, PhD*. Management of Dental Implant in Mandibular Idiopathic Osteosclerosis: A Case Report. On J Dent & Oral Health. 7(4): 2024. OJDOH.MS.ID.000666.
-
Dental implant treatment, Idiopathic osteosclerosis, IO tissues, Periapical periodontitis, Implant therapy, Mandibular molar, Dental calculus, Implant surgery, Oral hygiene, CAD/CAM technique.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






