 Research Article
Research Article
Malocclusion and Quality of Life in Children Aged 3 to 5 Years in Salvador-BA
Amanda Araujo de Carvalho1*, Mercia Sacramento dos Santos2, Marilene Batista Colaço Costa3, Tatiana Frederico de Almeida4 and Maria Cristina Teixeira Cangussu5
1Master’s student in Dentistry and Health/UFBA, Dentist/UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador BA, Brazil
2PhD in Dentistry and Health/UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador BA, Brazil
3Adjunct Professor/UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador BA, Brazil
4Adjunct Professor/UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador BA, Brazil
5Full Professor/UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador BA, Brazil
Amanda Araujo de Carvalho, Master’s student in Dentistry and Health/UFBA, Dentist/UFBA. Rua Araújo Pinho, 6th floor, 62 Canela. Salvador BA. CEP: 41110-150, Brazil.
Received Date: January 24, 2023; Published Date: February 03, 2023
Abstract
Objective: To describe the association between malocclusion and oral health-related quality of life (SOQL) in children aged 3-5 years in Salvador-BA.
Methods: This is a cross-sectional study involving children from health units and/or enrolled in public day care centers in 2018. The inclusion criteria were to be between 3 and 5 years old, be enrolled in municipal day care centers and be present during the gathering.
Exclusion criteria: Age outside the 3-5 years age group; not offering assent; have health conditions that make the exam unfeasible; not having the free and informed consent term and the questionnaire signed by the parents/guardians.
Results: 1566 children aged 3-5 years participated. The mean age was 53.5 months. 50.4% belong to the male gender, most were declared to be brown (60.7%) and black (31.7%). Malocclusion was moderate/severe in 26% of the population and the most frequent was anterior open bite (13.9%). There was a statistically significant difference between malocclusion and B-ECOHIS for pain in the teeth, mouth or jaws (p-value=0.05), difficulty in drinking (p-value=0.02), eating (p-value=0.02)-value=0.02), and difficulty sleeping (p-value=0.04).
Conclusion: Malocclusion has a potential association with conditions that interfere with the reduction of OHRQL in children aged 3-5 years.
Keywords:Preschool; Malocclusion; Health related quality of life; epidemiology
Introduction
Malocclusion consists of a change in the pattern of growth and development that directly affects the relationship between the teeth [1]. Its consequences involve the imbalance of the stomatognathic system and the impact on the quality of life of both children and adolescents [2-4]. This is because the aggravation has the potential to generate changes in the function, phonetics and aesthetics of those affected. In Brazil, due to its prevalence, it is considered a public health problem because it occurs from the preschool age group to adulthood [5].
According to the last national oral health survey with results released in the country, SB BRASIL 2010, 5-year-old children had a prevalence of 23% of class II and III, and 66.7% of 5-year-old children had at least 1 condition of malocclusion, which is the third most prevalent oral condition in Brazil [6]. The prevalence of malocclusion in the preschool age group in Brazil has been described in the literature by values ranging from 36.7% to 58.3% [7-10].
The analysis of the Quality of Life Related to Oral Health (QHROL) permeates daily activities and the way in which the individual understands their well-being in a physical, psychological and social sense [11]. In order to assess the effects of the oral health situation on the quality of children’s lives, the Early Childhood Oral Health Impact Scale (ECOHIS) was developed to be completed by parents/guardians. Its version adapted for Brazil, the B-ECOHIS, demonstrated effectiveness in measuring this issue, mainly for the age group from 2 to 5 years old. It includes child impact and family impact sections, considering the perception of parents or guardians regarding the impact of the oral health situation on quality of life and daily activities [12].
In addition, measuring the quality of life for oral health can provide information on health management that provide a basis for health policies, prioritization of more vulnerable groups and adequate distribution of resources [12].
With regard to malocclusion, from an early age, occlusal changes can affect affected individuals in the social aspect, with negative experiences that can cause emotional harm. It is also observed that some subtypes of malocclusion may have greater negative impacts on quality of life than others [13]. In association with the B-ECOHIS instrument with the Scale of Oral Health Outcomes for 5 year old Children (SOHO-5), open bite was related to reduced quality of life in 5-year-old children. However, the same study did not observe an association between the other types of malocclusion and the quality of life of children [9].
Kramer, et al. (2013), identified a statistically significant association between the presence of malocclusion and SOQR in children aged 2-5 years [14]. However, the literature is still controversial in this regard, also showing a non-statistically significant relationship between malocclusion and the OHRQL in preschool children [7, 9, 15].
In this sense, the present study aimed to describe the association of malocclusion with quality of life related to oral health in children aged 3-5 years in Salvador-BA.
Methodology
A cross-sectional study was carried out, in which children of the preschool age group from health units and children enrolled in daycare centers and public and community preschools in the city of Salvador-BA in 2018 participated. sample, the 12 sanitary districts of the municipality were taken as reference, in a representative way.
It was established as an inclusion criterion to be 3-5 years old, to be regularly enrolled in the selected municipal day care centers and to be present at the day care center or at the health units chosen at the time of data collection. As exclusion criteria were established: being aged outside the age group of 3-5 years; children who do not offer assent to participate; have health conditions that make it impossible to carry out the oral examination; not having the free and informed consent term and the questionnaire signed by parents or guardians.
Data collection was based on the application of a questionnaire to parents or guardians and oral examination of the children. These examinations took place in selected day care centers and health units in each district and were performed by 11 examiners. A prior theoretical-practical calibration took place among all examiners. The intra-examiner agreement was measured from the repetition of 10% of the oral exams one week after the 1st exam. For the evaluated oral conditions, calibration was considered sufficient when Cohen’s Kappa values equal to or greater than 0.77 and interand intra-examiner agreement rates equal to or greater than 90% were reached.
At the end of data collection, the total study population was 1591 children. For the present study, the original database was revised, resulting in a sample consisting of 1566 children, for whom all the data of interest were obtained.
The questionnaire applied to parents or guardians contained questions about sociodemographic data, oral health condition and quality of life related to oral health. For sociodemographic data and general health, an instrument was constructed by the original project team. The examiner filled in the information about the district and neighborhood to which the school unit belonged and, subsequently, the self-administered questionnaire, together with the TCLE, was sent to those responsible for the children who met the inclusion criteria.
Caregivers were also asked to answer questions about SOQL using the B-ECOHIS, the Brazilian version of the Scale of Impact on Oral Health in Early Childhood (ECOHIS), culturally adapted in Brazil 16 in 2008 and later validated 12 in 2012. The B-ECOHIS consists of 13 items related to two sections: Children’s OHRQL and Family OHRQOL. The first has four domains: symptoms, function, psychological and social interaction. The family OHRQL section has two domains: stress and family function. The general effect on SOQOL was considered present during data analysis when there was at least one positive response (frequency equal to or greater than ‘sometimes’) for any of the items in this instrument, that is, the frequencies “never” and “almost never” were considered as absence of effects.
Malocclusion, the exposure in question in this study, was evaluated according to the Foster and Hamilton Index (1969) indicated by the WHO for the evaluation of primary and permanent dentition. The index considers four measures, namely: the presence or absence of a canine driver, posterior crossbite, overjet and overbite. At the end of the application, the child who presented at least one alteration in the evaluated measures was considered as having malocclusion.
Table 1:Classification of conditions analyzed in the questionnaire applied to guardians and oral examination-Salvador-BA, 2018-2019.
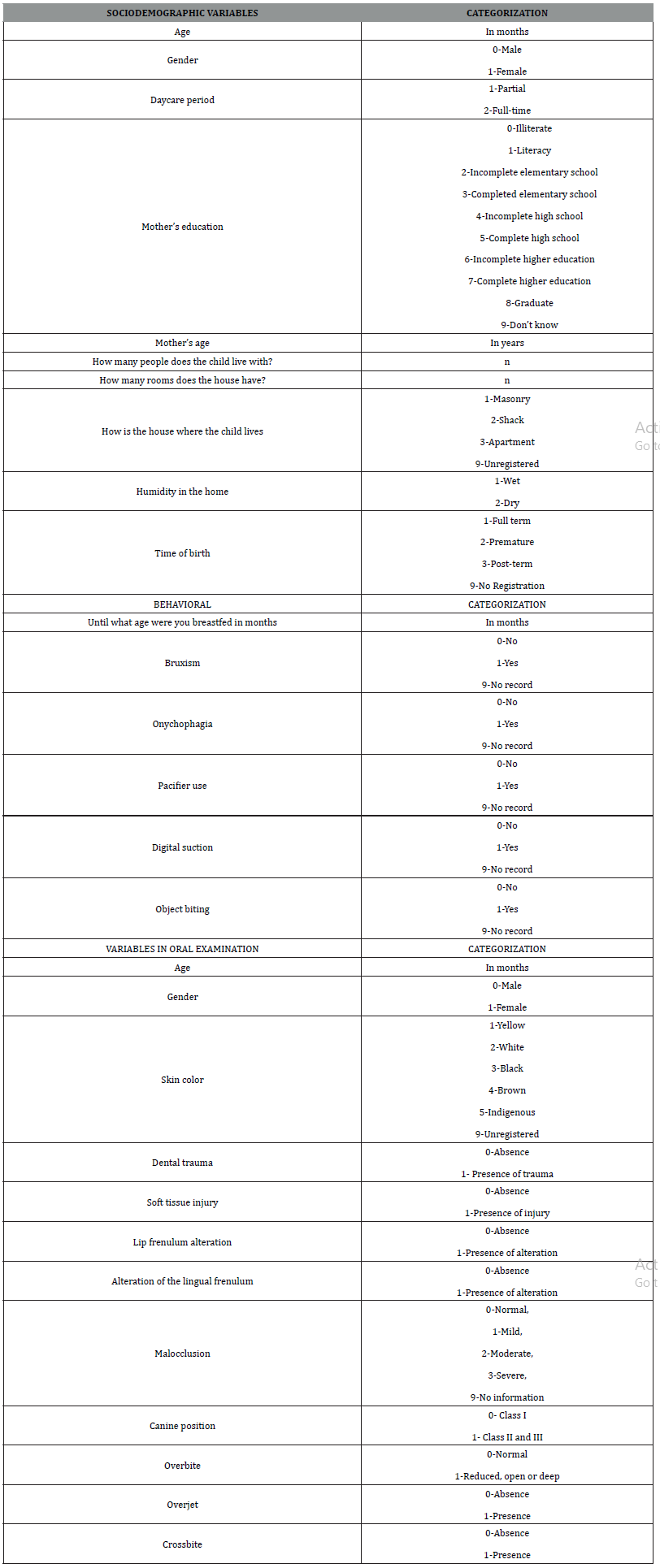
Table 1 explains the variables of this research and their respective categorizations.
For statistical analysis, data from oral examinations and questionnaires were entered into the EXCEL program to clean and prepare the database for analysis that took place later in the Minitab 14 software.
In this study, we considered the answer “I don’t know” to questions about the frequency of negative events related to the child’s oral health, such as lack of perception of a negative effect. The same occurred for the absent responses, so that both were recoded as “never”.
Descriptive analyzes of sociodemographic conditions, B-ECOHIS (its sections, domains and items separately) and malocclusion were performed. Pearson’s chi-square test was used in the exploratory analyzes of the factors potentially associated with the negative effect on the B-ECOHIS and its sections (in the four evaluated models), observing a significance level of 5%.
The original study was approved by the Ethics and Research Committee of the Faculty of Dentistry of the Federal University of Bahia (CAAE 78351317.0.0000.5024).,
Results
The study population consisted of 1566 children aged 3 to 5 years from Salvador-Ba, living in 25 neighborhoods divided among the 12 health districts of the municipality. Age ranged from 12-71 months, with an average of 53.5 months. Of these, 50.4% (n=789) are male, most were declared by parents or guardians to be brown or black, 60.7% and 31.7% respectively. With regard to socioeconomic data, maternal education was mostly incomplete higher education (43.6%) and 65.9% of mothers are between 26 and 44 years old. Regarding housing, 76.9% of families lived in masonry houses and 72.2% reported living with 2-4 people in each residence, in addition to the child (Table 2).
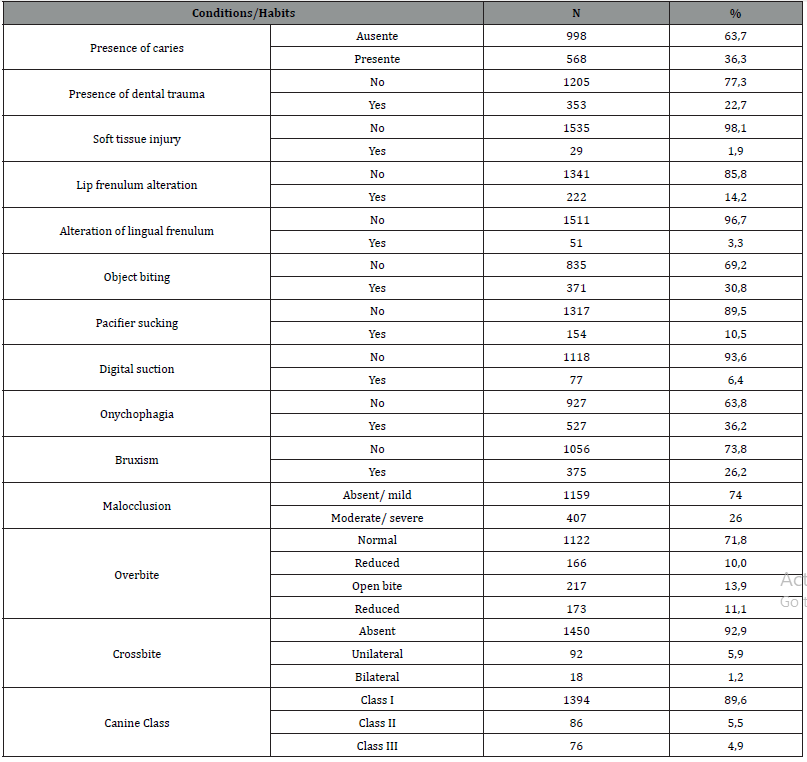
When assessing oral health, most preschoolers (77.3%) did not have dental trauma or alterations in soft tissues (98.1%). In addition, a prevalence of 36.3% of dental caries was observed. With regard to parafunctional habits, the most frequent were: the habit of biting objects and bruxism, resulting in 30.8% and 26.2% of the sample respectively. Malocclusion was identified as moderate or severe in 26% of the population and the most frequent type was anterior open bite, in 13.9% of preschoolers. The least frequent condition was bilateral crossbite, occurring in 1.2% of children, and reduced overbite, identified in 3.2% of the study population (Table 3).
Table 2:Distribution of sociodemographic characteristics among preschoolers in Salvador-BA, 2018 (n=1566).
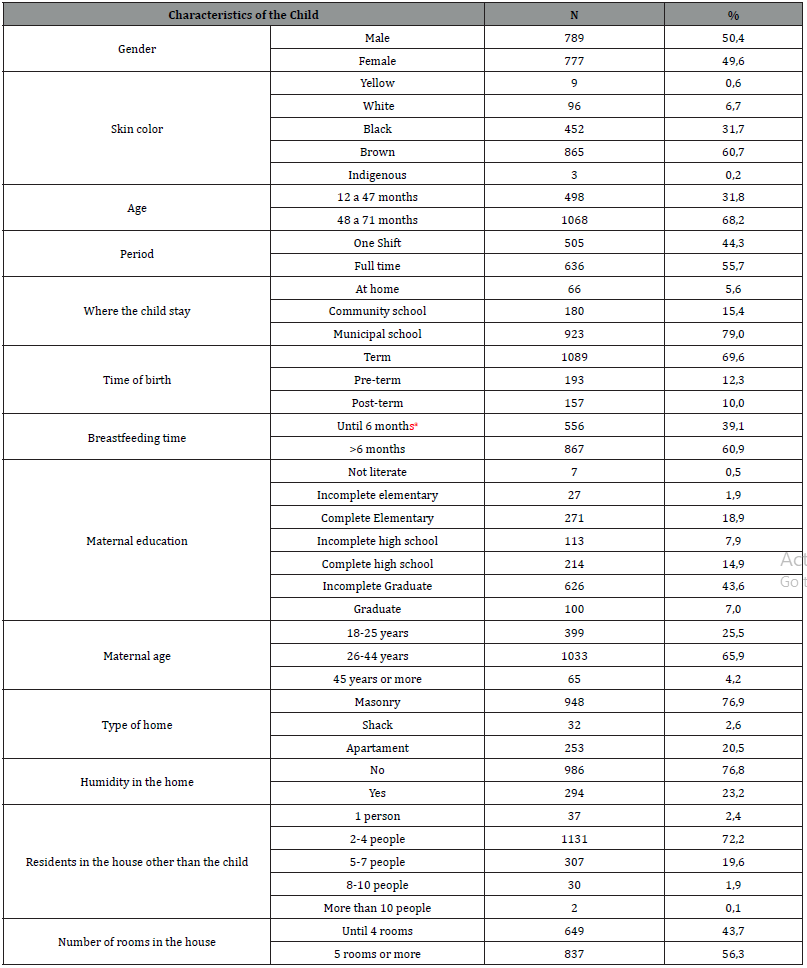
aIndicates breastfeeding absent or in a period less than or equal to 6 months
Table 3:Distribution of oral health conditions and parafunctional habits among preschoolers in Salvador-Ba, 2018 (n=1566).
In the assessment of quality of life related to oral health, analyzed using the B-ECOHIS, the negative effect according to the presence of malocclusion was recorded in Table 3. Among those who reported the existence of pain in the teeth, mouth or jaws, observed There was a higher prevalence in children who did not have malocclusion (21.74%) compared to those who had malocclusion (19.67%). The difficulty in drinking hot or cold drinks due to problems with teeth or dental treatments, when existing, was mostly reported by those who did not have malocclusion (9.32%) when compared to those who had malocclusion (6 .14%). In terms of eating, difficulties due to problems with teeth or dental treatments were more prevalent among those without malocclusion (12.51%) and 9.58% among those with malocclusion. Sleep was impacted due to dental problems or dental treatments in 6.21% of children without malocclusion and in 3.19% of those with malocclusion (Table 4).
Table 4:Negative effect reported for each B-ECOHIS item, according to the presence of malocclusion, by caregivers of preschoolers in Salvador-Ba, 2018 (n=1566).
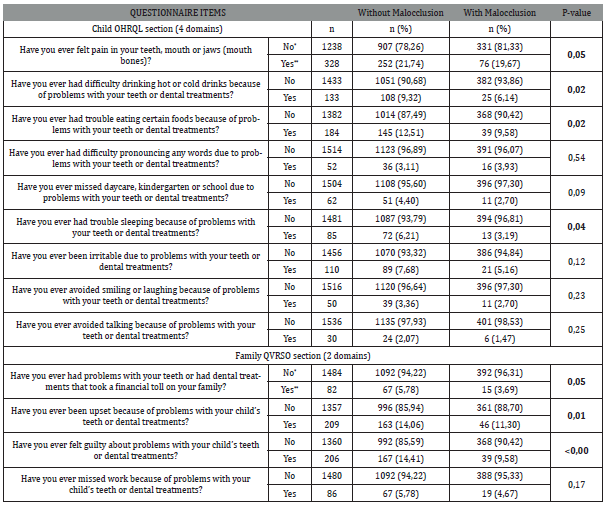
There was statistical significance for pain in the teeth, mouth or jaws (p-value = 0.05), difficulty in drinking (p-value = 0.02) and food intake (p-value = 0 .02), and also for difficulty sleeping due to problems with teeth or dental treatments (p-value= 0.04) (Table 4).
For children without malocclusion, a higher prevalence of negative effects was observed when evaluating the child and family sections of the B-ECOHIS, and its domains. There was statistical significance for the children’s QHRSB section (p-value=0.00), Symptom Domain (p-value=0.05), Function Domain (p-value=0.00), Psychological Domain (p-value=0.00), value= 0.00), Family QVRSB section (p-value= 0.00), Parental stress domain (p-value= 0.00) and Family function domain (p-value = 0.04) (Table 5).
Table 5:Negative effects on the B-ECOHIS sections and their respective domains, according to the presence of malocclusion, reported by caregivers of preschoolers in Salvador-Ba, 2018 (n=1566).
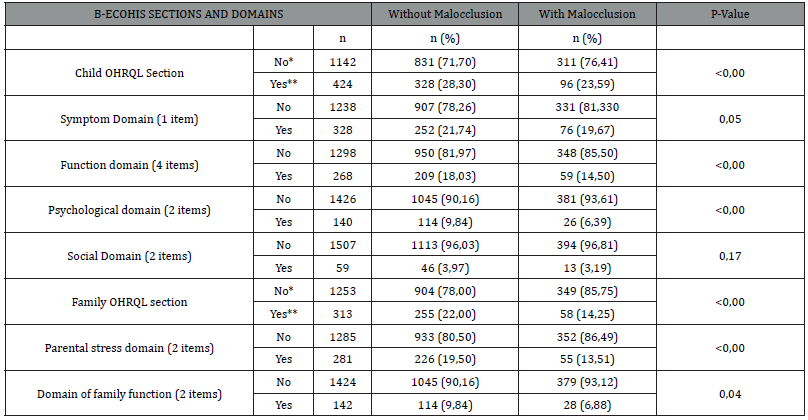
*No=Never/almost never **Yes=Sometimes, often, very often
Discussion
The present study identified the presence of malocclusion potentially associated with the frequency of pain in the teeth, mouth or jaws, difficulty in ingesting liquids and food, as well as difficulty sleeping. Regarding the family domain, malocclusion has the potential to cause family financial impact, lead to annoyance and guilt. In addition, the B-ECOHIS identified an association between malocclusion and the child OHRQOL section, with the function, psychological and symptom domains, with the family OHRQOL section, the parental stress domain and the family function domain.
Although the current study demonstrates a potential association between malocclusion and OHRQOL, for the instrument used (B-ECOHIS) the relationship is still controversial. Kragt, et al. (2016), in a systematic review and meta-analysis, show that children with malocclusion are 1.74x more likely to have an impacted OHRQL compared to children who do not have malocclusion [3].
Despite having the same design as that of this study, in a crosssectional study carried out in 2013 with preschoolers aged 60- 71 months, although percentages of interference of oral health in the quality of life of children and adolescents were observed, for malocclusion there was no statistical significance with direct association [15]. Like the study conducted here, the B-ECOHIS was used as an impact measurement instrument. It is suggested, therefore, that the instrument may have limitations for such measurement.
The ECOHIS and its adaptations, such as the B-ECOHIS (used in the present study) are indicated for a specific age group-3 to 5 years. The age group studied potentially does not have an intense social life and refined aesthetic self-perception of the problem. In addition, in this age group, children do not mature enough to make an intense aesthetic comparison with other children [10]. In addition, the age of children can interfere with the association of malocclusion with OHRQL, being more noticeable at older ages [3].
Furthermore, the completion of the instrument is carried out by the parents/guardians. From this, the results suffer interference from the parents’ perception regarding the very definition of malocclusion with the concept of OHRQOL [3, 7, 9, 16]. This is because the presence of pain can be a determining factor for parents or guardians to perceive problems oral cavity in children, which does not usually occur in malocclusion [17]. It is considered, therefore, the possibility that the results are underestimated. In addition, it should be considered that cultural influences can lead to different interpretations of quality of life, as well as of malocclusion [3].
Despite not identifying an association with general malocclusion and SOQR, some studies have identified a significant association with open bite. This finding may be related to the fact that-mainly because it is anterior -it is a more noticeable subtype of malocclusion [9, 18, 19]. In another cross-sectional study, which evaluated preschoolers aged 2-5 years, conducted in Canoas-RS, an association was identified between malocclusion and SOQOL, using the B-ECOHIS [14]. When performing a meta-analysis in 2016, Kragt and collaborators reinforce that, despite identifying impacts on the quality of life of children with malocclusion, , further research is needed to assess the impacts of age group, cultural diversity and potential other individual factors in reducing the quality of life related to oral health [3].
In this study, the most frequently reported discomforts in the B-ECOHIS by parents/guardians were: pain in the teeth, mouth or jaws and difficulty in ingesting food and liquids. Such findings are similar to those reported by Corrêa Faria, et al. (2015) and Vasconcelos, et al. (2021), the latter only did not report difficulty in ingesting liquids and food, but highlighted an impairment in the pronunciation of words [7, 20]. Such alterations are more evident to parents or guardians than aesthetic impairments, since they densely interfere with function [20]. Thus, it is possible to infer that despite the alterations generated by malocclusion, its impacts are not robustly experienced in terms of OHRQOL in preschoolers aged 3-5 years and their families. Studies that identify such associations are not common in the literature, and it is suggested that other studies be conducted in the same line so that the association is investigated [21].
As potentialities of this work, we highlight the sample size and its representativeness, which provides greater reliability to the results. However, as limitations, it is believed that the B-ECOHIS instrument used may have underestimated the findings due to the interference of the subjective perception of parents/guardians. Furthermore, the hypothesis that malocclusion may have little or no effective impact on the experiences that make up the OHRQOL in children aged 3-5 years is taken into account.
The present study concludes that malocclusion has a potential association with aggravation in the frequency of pain in the teeth, mouth or jaws (p-value=0.05), difficulty in ingesting liquids (p-value=0.02) and food (p-value =0.02) and difficulty sleeping (p-value=0.04)-domains of function, symptoms and psychological. There was also significance in the family domain by generating family financial impact (p-value=0.05), leading to annoyance (p-value=0.01) and guilt (p-value<0.00)-parental stress. Such results are important to support the establishment of public policies in health management from primary care to the age group.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Tondolo Junior J, Knorst JK, Menegazzo GR, Emmanuelli B, Ardenghi TM (2019) Influence of malocclusion on oral health-related quality of life in children: a seven-year cohort study. Dental Press J Orthod 26(2): e2119244.
- Dimberg L, Arnrup K, Bondemark L (2015) The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod 37(3): 238-247.
- Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM (2016) The impact of malocclusion on oral health-related quality of life in children-a systematic review and meta-analysis. Clin Oral Investig 20(8): 1881-1894.
- Feres MFN, Abreu LG, Insabralde NM, Almeida MR, Flores Mir C (2017) Effectiveness of open bite correction when managing deleterious oral habits in growing children and adolescents: a systematic review and meta-analysis. Eur J Orthod 39(1): 31-42.
- Bauman JM, Souza JGS, Bauman CD, Flório FM (2018) Epidemiological pattern of malocclusion in Brazilian preschoolers. Cien Saude Colet 23(11): 3861-3868.
- Ministry of Health. SB Brazil 2010: National oral health survey-main results. MS Publisher; Brasilia; 2012.
- Vasconcelos FMT, Vitali FC, Ximenes M, Dias LF, Silva CP, et al. (2021) Impact of primary dentition malocclusion on the oral health‑related quality of life in preschoolers. Prog Orthod 22(1): 38.
- Carvalho AA, Almeida TF, Cangussu MCT (2021) Prevalence of mallocclusion and associated factors in preschoolers from Salvador-BA in 2019. Oral Health & Dental Science 5(4): 1-8.
- Perazzo MF, Gomes MC, Neves ET, Martins CC, Paiva SM, et al. (2017) Oral problems and quality of life of preschool children: self-reports of children and perception of parents/caregivers. Eur J Oral Sci 125(4): 272-279.
- Souza RV, Clementino MA, Gomes MC (2014) Malocclusion and quality of life in Brazilian preschoolers. Eur J Oral Sci 122(3): 223-229.
- Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, et al. (2016) A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Int Dent J 66(6): 322-324.
- Martins Junior PA, Jorge JR, Paiva SM, Marques LS, Jorge MLR (2012) Validations of the Brazilian version of the Early Childhood Oral Health Impact Scale (ECOHIS). Cad Saude Publica 28(2): 367-374.
- Piassi E, Antunes LS, Graça TCA, Antunes LAA (2019) The impact of mixed dentition malocclusion on the oral health-related quality of life for children and their families: a case-control study. J Clin Pediatr Dent 43(3): 211-217.
- Kramer PF, Feldens CA, Ferreira SH, Bervian J, Rodrigues PH, et al. (2013) Exploring the impact of oral diseases and disorders on quality of life of preschool children. Community Dent Oral Epidemiol 41(4): 327-335.
- Carvalho AC, Paiva SM, Viegas CM (2013) Impact of Malocclusion on Oral Health-Related Quality of Life among Brazilian Preschool Children: a Population-Based Study. Braz Dent J 24(6): 655-661.
- Carminatti M, Lavra Pinto B, Franzon R, Rodrigues JA, Araújo FB, et al. (2017) Impacto da cárie dentária, maloclusão e hábitos orais na qualidade de vida relacionada à saúde oral em crianças pré Audiol. Commun Res 22(0): e1801-e1801.
- Gomes MC, Neves ETB, Perazzo MF, Paiva SM, Ferreira FM, et al. (2018) Contextual and individual determinants of oral health-related quality of life among five-year-old children: a multilevel analysis. PeerJ 6: e5451.
- Ramos Jorge J, Motta T, Marques LS, Paiva SM, Ramos Jorge ML (2015) Association between anterior open bite and impact on quality of life of preschool children. Brazilian Oral Research [online] 29(1): 1-7.
- Rosa GN, Buzzati BCS, Piovesan C, Mendes FM, Oliveira MDM, Ardenghi TM (2015) Impact of malocclusion on oral health-related quality of life of preschool Children. Rev Gaúch OdontoL 63(1): 33-40.
- Corrêa Faria P, Paixão Gonçalves S, Paiva SM, Martins Júnior PA, Vieira Andrade RG, et al. (2015) Dental caries, but not malocclusion or developmental defects, negatively impacts preschoolers’ quality of life. Int J Paediatr Dent 26(3): 211-219.
- Tesch FC, Oliveira BH, Leão A (2008) Semantic equivalence of the Brazilian version of the Early Childhood Oral Health Impact Scale. Cad Saude Publica 24(8): 1897-1909.
-
Amanda Araujo de Carvalho*, Mercia Sacramento dos Santos and Marilene Batista Colaço Costa. Malocclusion and Quality of Life in Children Aged 3 to 5 Years in Salvador-BA. On J Dent & Oral Health. 6(4): 2023. OJDOH.MS.ID.000645
-
Oral health, Teeth, Mouth, Jaws, Food, Malocclusion with OHRQL, Sleeping, Dental treatments, Pain in the teeth, Oral examinations.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






