 Research Article
Research Article
Implications of Oral Health Policy Consequent Covid19
Shaymaa Hussein Rafat kotb*
Alazhar university, faculty of Dental Medicine, Department of Oral Medicine, Periodontology, oral Diagnosis and Dental Radiology, Assuit branch, Ministry of Health & Population, Egypt
Shaymaa Hussein Rafat kotb, Alazhar university, faculty of Dental Medicine, Department of Oral Medicine, Periodontology, oral Diagnosis and Dental Radiology, Assuit branch, Ministry of Health & Population, Egypt.
Received Date:January 03, 2023; Published Date: January 12, 2023
Abstract
COVID 19 virus rearrange the priorities of the global society regarding oral health to systemic health. Oral Health Policy and Epidemiology (OHPE) is the connection of dentistry, medicine, and public health which increase the perspective and impact of global and community health practice and policy through education, research, and leadership. Dental faculties and students, with community stakeholders and oral health professionals, drive collaborative, interdisciplinary, and innovative approaches to achieve oral health equity and wellbeing for all. Global vision for oral health policy is fully integrated in general health and based on primary health care, with emphasis on promotion on oral health and prevention of oral disease. This policy is a framework contribute to a program strategy of public health to guarantee the access to fundamental rights.
Aim: To thourough the light on impact of oral health diseases on systemic health condition.
Conclusion: The need to develop appropriate policies specific to the oral health needs. There is a bidirectional relation between poor oral hygiene and chronic systemic diseases. Oral microbium is consider a strong contributing factor that trigger the inflammatory condition and resultant systemic diseases. World Health Organization, promote and encourage the preventive measures program to help keep and maintain good oral health to protect the overall body health.
Keywords: Covid 19, Oral health, Oral prevention programs, Periodontal diseases, Malnutrition, Early childhood caries, Dental healthcare, Policy implementation, Oral health services
Introduction
Coronavirus 19 (COVID-19); is the most widespread pandemic in the last 3 years. Itis a highly contigous respiratory infection result in life threatening consequence. Dentistry is the most proffesion affected during pandemic wave. Dental healthcare professionals (DHCP) are potentially susceptible to this infection. Therefore, dental practitioners have to be aware of the various aspects of the disease, including its contagious nature and its impact on patients such as, adverse oral health outcomes or safe delivery of oral healthcare services. Academic or teaching dental hospitals provide dental education that is essentially based on safety and durability and adequately guarantee provision of successful clinical dental practicing [1].
Impact of the SARS-CoV-2/COVID-19 pandemic has an immense impact on the dental practice landscape. These include, for example, changed practice procedures due to change the hygiene standards, a reduction in jobs at one location and a need for new skills and jobs such as telemedicine applications at another location, changed patient flows and modified therapy options due to a possible loss of health insurance or improved training of staff to deal with pandemic situations. Consequences, all these challenges and possible influences that are changing the dental profession are collected, analyze, develop solutions and support for dental personnel that is for creating and forming the future of dental practice [2].
Health systems all over the world being faced with unprecedented COVID-19-related challenges ranging from the problems of a novel condition and a shortage of personal protective equipment to frequently changing medical guidelines. Covid 19 viruses has changed the global vision toward the importance relation of the oral health condition and the infectious diseases and with the noncommunicable diseases, moreover the impact role of the dental practitioners. Oral health remains a major and poorly managed problem in low income countries. Poor oral health can significantly impact on general health and so the quality of life. World health organization show the important to develop a dental health policy. Health Policy defines a vision for the future by outlines priorities and the expected roles of different groups; which aims at attainment of the highest possible level of good health and well developmental policies and universal access to good quality health care services without anyone having to face financial hardship as a consequence [3].
WHO, defines the health as “The fair opportunity to be healthy as possible”, This concept requires elimination of those societal factors (e.g., poverty, discrimination, lack of access to healthcare) that unfairly result in poorer health. Among the challenges identified is a normative environment in which oral health is not a priority. There is a demonstrated need for intensive health promotion campaigns aimed at changing attitudes toward oral health and increasing demand for oral health services that can contribute to both risk reduction and earlier diagnosis. With an educated and motivated public demanding oral health services, a need for expanded access to care would be required. Every patient should have a medical home and a dental home, preferably in a single setting, where the range of preventive and diagnostic services can be offered with all required expertise. Primary care providers from diverse professional back-grounds can play roles in educating the patients about impact of oral health state on general health and vice versa [4].
Whenever the population growth there are worsen the unmet demands for dental services. Oral health inequalities are usually defined as “avoidable and unfair differences in oral health between different groups of people”. Oral health outcomes tend to be worse among poorer, less educated, and less socioeconomic, even after controlling for individual behavioral factors. This is attributed to inability to afford dental care due to low-income category or no insurance cover. The affordability of a specific healthcare service, is determined by the ability to pay and the willingness to pay. This simply means that among older adults, two factors are at play; on one hand the decline of income and loss of private insurance after retirement affects an individual‘s ability to pay for dental services, Simultaneously, the dental need services continue to increase as long as the populations retain the teeth which develop more dental problems including periodontal diseases and coronal and root caries, so worsen the oral health condition [5].
Unmet dental care needs occur when an individual fails to receive effective dental care that could have improved his/her oral health. Oral diseases that have not been treated appropriately can lead to deteriorated quality of life through not only physical problems but also social and psychological issues such as work function, appearance, and interpersonal relationships. Failure of access to timely dental care could lead not only to poor oral health but also to productivity losses. Variables in the predisposing domain include demographic characteristics, health beliefs, and social structures predisposing variables such as younger age, female gender, marital status, and low education level enabling variables such as income, engagement in precarious work, unemployment, medical aid as a type of insurance, and long working hours and need factors such as poor oral health status [6].
As urbanization increases, so does the expectation for a healthy life and thus the demand for dental care services. Dental health is an important factor in daily life routines and is closely associated with maintaining a health-related quality of life. Poor dental health is negatively associated with general health conditions. Tooth loss among the elderly is one of the biggest contributors to impaired oral health, which affects physical health through the reduced capacity for chewing. The dissatisfaction with chewing ability had a significant effect on the quality of life by depriving individuals of the pleasure of eating what they desired. There is a positive association between tooth loss and increased risk of systemic diseases in adults [7].
Dental caries and periodontal disease are classified among the most common noncommunicable diseases in the world and, in addition, the most prevalent diseases of the mouth. These diseases result in reduced masticatory, swallowing and speech functions as well as pain and oral infections, leading to an increased risk of systemic diseases (e.g., heart attack, stroke) and psychological and relational disorders. Impact of oral health problems lead to several adverse consequences to the the general population, such as inability to keep a job, adverse pregnancy events, elevated risk of general chronic diseases, inflammatory diseases, nutritional imbalance, and oral cancer. Several barriers to access to dental care services, like inadequate dental coverage, insufficient provider availability, and individual level barriers such as lack of dental benefit and oral health literacy, lack of referral to oral care through primary providers, and perspective as the least priority in terms of overall healthcare [8, 9].
Periodontal disease is a common inflammatory microbial
disease affecting the population worldwide. Dental biofilm is the
main cause in initiating this condition. Its pathogenesis affected
and complicated by the relation of the pathogens and the immune
system. The mechanisms explain the role of periodontal disease in
systemic diseases:
a. Direct mechanism: The endotoxins produced mainly by
Gram-negative anaerobic bacteria in the oral cavity are known
to directly contribute to systemic disease. The periodontal
pathogens gain access into the blood circulation through the
ulcers located in the soft tissue walls of the periodontal pockets
resulting in collagen degradation, aggregation of platelets and
thrombus formation;
b. Indirect mechanism: This involves a possible trigger to
periodontal pathogens producing inflammatory mediators
in the body such as C-reactive protein (CRP), tumor necrosis
factor (TNF)-_, interleukin (IL)-1_, IL-1_, IL-6, prostaglandin
E2 (PGE2) and matrix metalloproteinases (MMP) causing an
autoimmune reaction.
There is a bidirectional relation between periodontitis and systemic disease based on the periodontal pathogens, which are mediators of inflammatory reactions in the body; whether they have entered the blood stream or remained in the oral cavity, they link oral and systemic health. The two-way association between periodontitis and non-oral systemic diseases, with periodontal pathogens needs to be broken by pay the attention to importance of the oral microbiome [10, 11].
Tooth decay (dental caries) is the most common chronic childhood disease worldwide, its progression contribute to many factors such as diet, oral bacteria biofilm, poor oral hygiene, and socioeconomic conditions. Most cavities from tooth decay when remain untreated, can cause mouth pain, difficulty eating and sleeping, poor school performance, and an overall worsened quality of life. There is a link between dental caries, dietary pattern, malnutrition and obesity. Diet is one of the contributing factors to poor oral health that consisting mainly of carbohydrates with a high glycaemic index. The “nutrition transition”, characterized by a global shift from traditional, whole-food diets to foods and beverages that have high sugar, fat, and salt content, has been driven by global increases in urbanization, trade liberalization, and food marketing. The key challenges which barrier the good oral health, like: nutrition widely-available and inexpensive junk food; parents giving children money to buy snacks, not enforcing tooth brushing, and poor access to a ordable and dental services, leaving most dental disease untreated and frequent consumption of sugar in sugary liquids in the baby bottle, carbohydrate-dense and sugary snack foods and beverages-has been identified as the main cause of early childhood caries (ECC) in children under age six [12-14].
Obesity is a chronic health condition determined by an individual‘s body mass index (BMI). It is consider as epidemic and a worldwide growing concern due to the modern urbanization and the dramatic transition in the food habits and lifestyle. This complex metabolic disorder is characterized by excessive fat accumulation in the body resulting in adverse health effects and life-threatening noncommunicable diseases in adulthood. The association of gastrointestinal or gut microbiome alterations with obesity in adults and children attributed to gut microbial dysbiosis, which triggers the host‘s inflammatory, immune, and metabolic responses. The potential role of the salivary microbiome in human diseases has increasingly been explored. The oral cavity is a potential point of ingress for the microbes into the human body serving as a passage to the gut, mediated by saliva ingestion. Human microbiome becomes the prey of human immunity and directly provides essential nutrients to the human body and the microbial dysbiosis (the overgrowth of any microbial species at any site of the human body) is the direct cause of the host‘s inflammatory and metabolic disorders. A decrease in the microbial diversity in gut microbiome and richness was observed in people with obesity compared to the normal controls this suggeste changes in salivary microbiome composition in people with obese or overweight BMI which reflect their susceptibility to oral diseases [15].
The contemporary philosophy of caries management has shifted from the traditional surgical approach to a novel concept that is more oriented toward controlling etiological factors due to the current understanding of dental caries as a non-communicable chronic behaviour-mediated biofilm disease. A healthy oral microbiota benefits the host by immunological initiation, the down-regulation of inflammatory responses, and the regulation of exogenous microorganism colonization. The changes to the local environment, such as increased sugar intake, shifts the composition of the oral microbiota to adapt to the new environment. The enrichment of the acidogenic and aciduric microorganisms break the homeostasis of the micro-community and cause dental caries. The ecological plaque hypothesis indicates that caries can be controlled by improving oral hygiene, by reducing the targeting pathogenic microorganism and interfering with the environmental factors that are suitable for the cariogenic microorganism. contemporary caries management embraces the philosophy of minimal intervention dentistry, which places the nonrestorative management of dental caries as a priority in all of the stages of caries development. The essential components in this management include dental plaque control, reducing caries risk, preserving dental hard tissue, and long-term maintenance [16].
There is increasing evidence of an association between oral and general health in older people, mediated through common risk factors including nutrition, systemic inflammation, infection, and psychosocial factors, but causal links are still under investigation. A confirmed bidirectional association exists between periodontal disease and diabetes mellitus. Diabetes mellitus is one of the most rapidly growing chronic conditions in the world especially in low- and middle-income countries and is strongly associated with being overweight, poor nutrition and socioeconomic inequalities. Elevated blood glucose levels (hyperglycaemia) leads to several microvascular and macrovascular complications such as diabetic retinopathy; neuropathy; nephropathy, heart, peripheral arterial, and cerebrovascular disease; obesity, certain cancers; pancreatitis; erectile dysfunction; and non-alcoholic fatty liver disease. Hyperglycaemia also leads to various oral complication and more particularly, periodontal (gum) diseases. Poor control of diabetes results in increased severity of periodontal disease, whilst periodontitis is associated with elevated risk of dysglycaemia and insulin resistance in patients with diabetes as well as increased incidence of diabetes [17, 18].
Another association between periodontal disease and cardiovascular disease cancer, coronary heart disease, and cerebrovascular diseases, also confirmed. Increasing evidence of an association between aspiration pneumonia and poor oral health amongst older people, including the presence of periodontal pathogens, dental and denture plaque. The prevention and intervention of oral disease may lead to improving the health status. Moreover, Maintaining good maternal oral health during pregnancy is important for both the mother and the child. Children are more likely to have poorer oral health across the lifespan if the mother also has poor oral health. A lack of timely oral health education for mothers may also contribute to oral health or feeding behaviours in children that precipitate dental decay during early childhood. In addition, there is a link between poor maternal oral health during pregnancy and an increased risk of adverse birth outcomes, such as low birth weight or pre-term birth. The early prevention approach help in reverse the condition [19].
The WHO defines health systems as “all organizations, people and behaviors whose primary purpose is to promote, restore or maintain health”. Thus, a well-developed health system includes not only public hospitals, but also private hospitals, community health facilities, nursing homes, and other types of healthcare organizations and related healthcare workers. A well-designed policy framework is the cornerstone for quality healthcare systems. Without government supervision, it is impossible to achieve effective coordination for various services. A community-based participatory research approach, involves community leaders and members, can be effective oral health education programs. Dental health educators can play a unique and valuable role. They can collaborate with dental health providers in promoting oral health through effective interprofessional, skill-mix efforts. The success of persuasive health messages depends not only on message content (i.e., what is said), but also on how that content is linguistically framed and delivered (i.e., how it is said) Understanding these oral health disparities is key for developing efforts to facilitate oral health treatment. Impact of this policy help in bridging the gap by development of multilevel interventions in addressing oral health service accessibility [20].
ADA governing bodies played a significant role in creating the dental branch at the WHO, an organization which shaped global dental public health messages. The World Health Organization (WHO) declared that maintaining oral health is an essential factor for maintaining health. Therefore, that is state should focus in the importance of the management of periodontal diseases and consider public health approaches to pursue improved methods of preventing and managing periodontal diseases. Oral health education for patients, and continuous maintenance and care are crucial for preventing periodontal diseases. Therefore, it is possible to prevent oral disease by removing dental plaques, which is the cause of oral diseases. Dental plaques cannot be completely removed by physiological exercises such as the tongue or cheek movement and gargling. It is effectively removed by a physical method current dental scaling procedures are generally focused on removing dental calculus, and they rarely include removal of biofilms and tooth brushing education for maintenance and management following calculus removal. Moreover, WHO recommends brushing one‘s teeth at least twice daily. Toothbrushing is the basic and practical self-management method for dental plaques. Toothbrushing removes food residues and stains, as well as dental plaques attached to maintain good oral hygiene [21].
The policy strategies based on social trust and transparency. Transparency is consider a key concept of public justification, which plays a pivotal role in reaching a legitimate conclusion through pluralistic democracy. Public trust initiated from the provision of transparent information and communication, to which the profession has insufficiently committed until now. Thus, maintaining trust and honesty, one of the commitments in the charter of medical professionalism. transparently in the dental profession, will be a big challenge and change for the profession in the future. The policy require to be dynamic to match the changes in consumer behaviors. Long-term market observations are needed to assess the importance of decesion maker and so changing the social behavior [22].
The perspective of public health, need an ethical frameworks to resolve the conflicts between values in public health interventions. Ethical justification mention briefly as follows: Non-maleficence: possible harms or adverse events on health may be rare. Autonomy: protect the general public‘s oral health and reduction of health inequity can override individual freedom of choice and become exempt from seeking consent by a legitimate process of the representative system. Public health scheme based on large portion of empirical systematic reviews support the benefit of the preventing measures of oral diseases. public health policymaking built on a schematic diagram for over-simplification public health interventions. The-Intervention Ladder‖ is a useful metaphor representing the level of liberty infringement in public health interventions The ladder utilized on several occasions for demonstration of public health ethics and modification to improve its unidimensional approach [23].
Health policy-related action need decision making, like reduce the consumption of sugar or efficacy adding of Community water fluoridation for reducing dental caries incident. This can be done by using effectively the ban on advertisements by the advertising health warnings label. Scaring the consumers with depictions of illnesses and deteriorating health may be a more straightforward and effective message. Another warnings stating that “smoking can end in death” and have other frightening effects. On the other hand, “nutritional warnings “only include information on the content of the product. The real challenge for consumers are to identify and combat the misleading marketing information [24, 25].
Health care provision becoming a growing concern for policy makers and researchers, as part of the Universal Health Coverage target of the Sustainable Development Goals. The World Health Organization focused the policy framework to carry out its “health for- all policy for the twenty-first century” platform, oral health care is prioritized for its impact on quality of life, disease prevention, and maintenance of good health, alongside its ease of prevention. In fact, the WHO notes that oral healthcare is the singular area of public health where “such a major problem can be so easily prevented through very simple methods”. Overall, higher education levels, better general and mental health, lower age, parental status, lower sense of discrimination, and better access to dentists are positive predictors of having good teeth and thus generally good oral health. The barriers to oral healthcare-seeking change the behaviors by change in dietary habits and the limited access to dental services in remote settling areas pose public health problems in the host countries [26].
The need for policymakers, researchers, and providers to expand the focus from individual level factors to broader contextual processes. Other strategies can include providing staffing, the provision of adequate infrastructure for effective workplace organization, housing programs, and the establishment of career pathways There is also a critical need for culturally competent educational and community outreach programs on oral health literacy, attitudes, oral health information, and selfcare interventions. Dental health educators can play a unique and valuable role. Dental health providers aid in promoting oral health programs that better support communities through effective interprofessional, skill-mix efforts. Dental providers are also ideally positioned to provide brief interventions to assist their patients to quit smoking Routine dental visits can examine the oral cavity for signs of mucosal and tooth changes, recognize variations from normal, and establish management and referral pathways. policy makers design the most suitable and contextually relevant academic interventions by using online platform which was widely used during pandemic covid19 [27, 28].
Changing behaviour considered as a cycle. It start with patients being unaware of the problem, through a time when they are thinking about making a change, to when they are actively preparing to change by planning and setting goals, to when they are ready to act, and then trying to maintain the change to avoid the relapse. Oral health behaviours are influenced by the social determinants of health. and people who are from lower socioeconomic groups often have more limited knowledge and negative attitudes to oral health and uptake of dental services, lack of awareness, and compliance with certain oral health behaviours (such as brushing and flossing) and lower probability of visiting a dentist regularly and are more likely to experience the burden of oral disease. it is important to understand the distinctive gaps in knowledge, attitudes and practices of this population to help inform preventive strategies, policies and practices required to improve oral health [29].
Ministry of Health (MOH) Malaysia introduced the preschool oral healthcare programme (POHP) with the objective of improving the oral health status of 5-6-year-old preschool children. This programme primarily focuses on oral health education (OHE) and clinical prevention at preschool centers. In 2003, the MOH published guidelines on oral healthcare for preschool children. In the guidelines, a few components of the POHP were revised including empowering dental therapists (DT) and teachers in school health and improving the oral health activities at preschool centers. Oral hygiene education is the provision of oral health information through giving advice or instructions to improve people‘s oral hygiene behaviour or their oral condition. The teamwork among dental personnel was very good. The healthcare assistants (HCA) are well trained in helping Dental therapist (DT) to provide dental treatment to the children such as atraumatic restorative treatment (ART). In 2018, the OHD of Selangor established the Oral Health Promotion Unit (OHPU) for each dental clinic. This unit consists of two dental officers (DO) and one dental therapist that aims to provide oral health education (OHE) such as TBD to all preschools. The OHPU helps in reducing the time taken during each visit as they provide OHE while DT concentrates on providing dental treatment [30, 31].
This policy recognizes that the primary responsibility for the health of the population lies in the population itself. The policy shall empower the population to participate in the design, planning and the execution interventions that improve their health status and receive feedback from respective duty bearers for their actions. Health education and guidance should be given priority in workplaces that mainly involve skilled workers, salespersons Oral health education provided by health care providers was the preferred source of information, developing resources which need training programs to account for sociodemographic and environmental variations such as language, culture and available access to dental services. There is gap of polices and practice guidelines to encourage and assist non-dental care professionals in promoting oral health. Therefore, the need to focus on developing policies and practice guidelines to promote oral health among people with systemic diseases. The importance of developing guidelines for mandatory oral health screening of all newly diagnosed people with systemic diseases( like diabetes ) and designing and implementing community based integrated approaches to improving health behaviour for promoting oral health and management of the systemic diseases [32].
A new model of health policy should be developed (in addition to the existing one) with solutions able to meet socially vulnerable subjects in their environment without waiting for the patient to visit the dental office. In other words, this health policy should be based more on education, prophylaxis and minimally invasive treatment of oral diseases, also using innovative transportable devices and instruments in order to reach people living on the margins of the social network. Atraumatic restorative treatment (ART) is the best known of these types of easy intervention, which can be performed outside the dental office [33].
The World Health Organization (WHO) declared that maintaining oral health is an essential factor for maintaining health. Oral health is determined by how well oral health behaviors are performed, and especially, the frequency of toothbrushing per day that is widely used as an index to predict healthy behavior. Brushing teeth three or more times a day not only reduces the risk of oral diseases but also the risk of cardiovascular diseases. The toothbrushing education project has a low level of awareness. Toothbrushing education should be monitored, and repeated training should be provided to increase. The average frequency of toothbrushing per day. the average frequency of toothbrushing per day was lower in males, those with a low educational level, the unemployed, and in those in the rural area. Therefore, indepth oral health promotion projects and national benefit policies should be considered for effective toothbrushing education by identifying the participants with lack of toothbrushing according to sociodemographic characteristics [34].
Policies and strategies that support oral health literacy, integration of oral health care with medical care, availability of resources to address inequities in access to care, and appropriate expenditures with improved utilisation are needed worldwide. Oral disease prevention and treatment at early stages of oral disease can support systemic health, preserve private and public resources, and maintain quality of life and well-being for older adults at every stage of life. Oral health integration is a key strategy for improving oral health care access, quality, and outcomes. Increasing prevalence of medical comorbidities will increase the importance of medicaldental integration to effectively manage patient care needs. A newly established partnership between the Centers for Disease Control and Prevention and the National Association of Chronic Disease Directors should help create a national medical-dental integration framework. To achieve the promise of oral health integration and better align oral and medical health care delivery, interprofessional partnerships between dental and medical practitioners are needed [35].
The Committee on Quality Health Care in America of the Institute of Medicine (IOM) states that health systems in the 21st century should strive to improve six dimensions of quality of care: safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity. International organizations, including the World Health Organization (WHO), and multinational health system evaluations have relied on this research, on whose basis the Lancet Global Health Commission defines a high-quality health system as follows: “A high-quality health system is one that optimizes health care in a given context by consistently delivering care that improves or maintains health outcomes, by being valued and trusted by all people, and by responding to changing population needs”. A quality health system is based on four values: its primary concern is its patients and it is equitable, resilient, and efficient. The demand for healthcare is increasing alongside economic growth. smart health is in a golden age of rapid development, a clear and unified definition of smart health is still lacking. smart health enables patients and doctors to communicate with each other through a mobile platform, while also enabling cross-regional and cross-country consultations, which demonstrates the true realization of mobile healthcare and telemedicine and, consequently, improves service quality [36, 37].
Tele dentistry is not a new field of study. The definition of tele dentistry is “the remote diagnosis and suggestion of treatment using videoconferencing technology”. It is an alternative to the standard delivery of dental treatment. Tele dentistry is a revolutionary aspect of patient treatment that is gaining popularity and importance fast. The exchange of information will result in enhanced patient care, and the capacity to engage more effectively with colleagues will increase comprehension of treatment goals. Tele dentistry has developed as a viable alternative for a number of dental specialties, including endodontics, orthodontics, oral surgery, and pediatric dentistry. Acceptable for identifying children with a reduced risk of developing dental caries. The accurate diagnosis of oral disorders, such as oral cancer, may be difficult in diagnostic dentistry, particularly in low-income regions with limited access to specialized dental treatment. Tele dentistry may thus satisfy this requirement and enhance treatment quality [38].
Results
The study findings are useful to guide the policymakers and stakeholders to improve “The Oral Healthcare Programme” through policy changes, financial aid by alleviate the financial barrier, human resource development, and enhanced school cooperation.
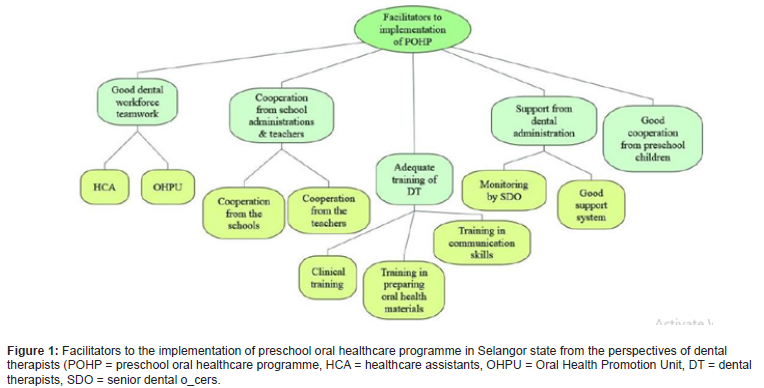
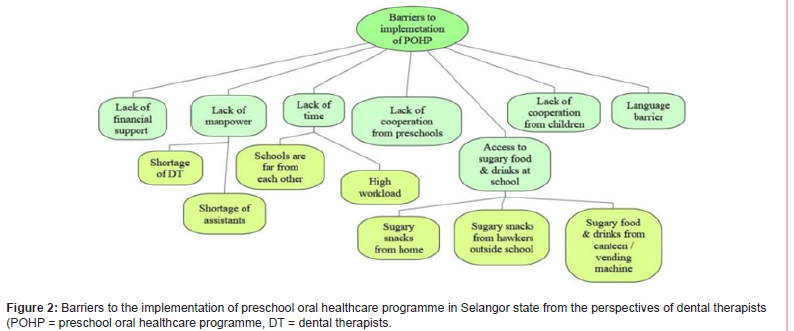
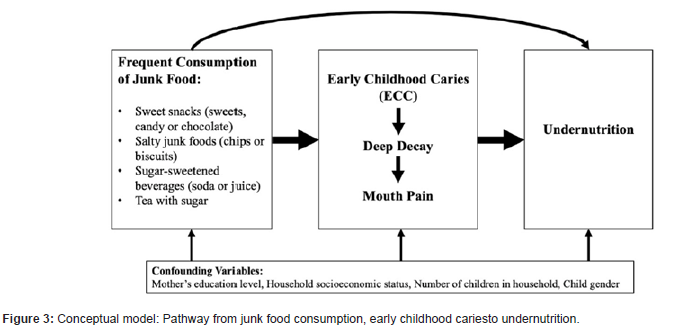
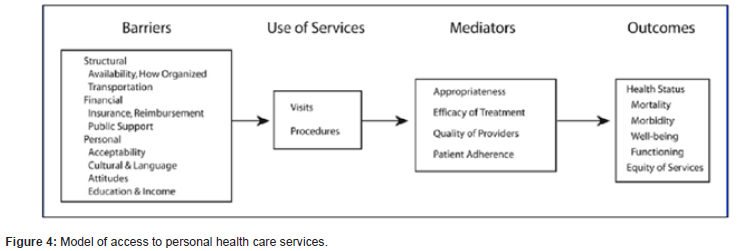
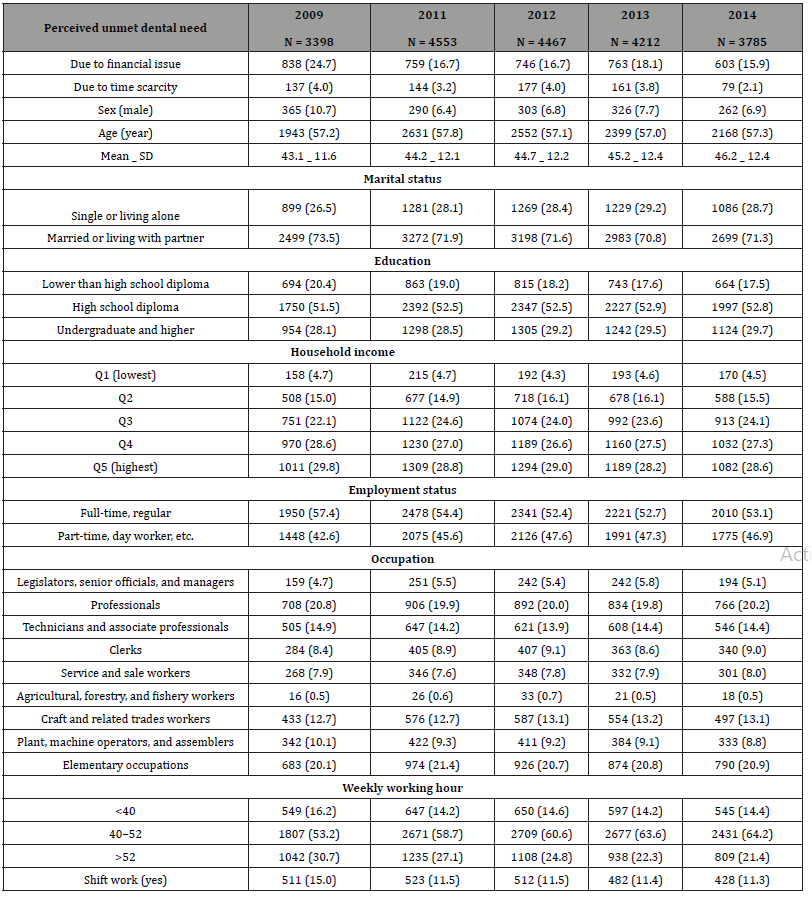
Table 1:General characteristics of the subjects.
Discussion
Good oral health contribute to the general health and the prevention of pathologies affect overall quality of life. Poor oral health causes a number of different limitations such as, functional, nutritional, aesthetical or psychological problems which effect on quality of life. Quality of life need awareness of impact of oral health on systemic health. A clear language as well as a charming smile a powerful sign of friendship, trust, togetherness and love. It’s also a sign of good oral health that have an impact on social life like self-awareness and well-being of the own body [39]. An imbalance towards a periodontal immune response is underlined for other chronic diseases. Epidemiological studies had shown that periodontitis was associated with the metabolic syndrome and cardiovascular disease. The suboptimal oral function was a potential risk of mortality. Dental health policy is critical to daily health maintenance and not just preventing the pain of dental diseases. The government needs to raise patients awareness regarding the importance of visiting a dentist, the promotion of oral health examinations and dental health policies for the population. The more national efforts and policy actions are needed to change the current unfavorable situation. This policy aims to provide equal dental service to all people and guarantees their “right to health”. Numerous countries have achieved the goal plan by addressing oral health disparities through sustained efforts to improve oral healthcare accessibility. The government should promote policies that relieve the financial burden of dental care for the population because the out-of-pocket expenditure. These policies would increase patient satisfaction with dental health and contribute to improving the quality of life of the population [40]. Implementation of oral healthcare programme from an early age to instill good oral health behaviours is vital. This is because healthy oral health habits developed at a young age tend to last until adulthood. Updated OH promotional materials are also very important to keep population and children especially interested. The language used in oral health promotion is very important in ensuring the children and population receive the messages clearly [41]. Most oral diseases can be prevented or managed by healthy behaviors’ such as enjoying a healthy balanced diet and cleaning teeth and gums effectively with a fluoride toothpaste twice every day. The key messages for the population include when and how to brush, specific habits associated with brushing, and, where necessary, assistance with brushing. Helping patients to improve their oral health involves providing tailored advice, teaching new skills, answering questions and regularly reinforcing key messages. Preventive approaches would not be successful without complete participation from every personnel especially the parents before teamwork. Teamwork within the team and the formation of OHPU were the main facilitating factors of implementing the POHP. In spite the teamwork in prevention activities would take time, but it offers a basis for enhanced health outcomes, so a good teamwork among the implementers is mandatory. The need to improve staff role descriptions, job descriptions, performance assessment, services objectives, and communications and relations between staff. The factor that highly influences as a barriers to the implementation of an oral health programme is financial support. Due to budget constraints and Insufficient funds. Another barrier factor is, dental fear and anxiety among adults and children have been documented as a problem in dentistry for numerous years. The cost of dental services imposes a large economic burden for the population and the government. lack of dental providers consider another challenging factor. To overcome this issue, the oral health care workforce need to be diverse and highly trained [42]. The Integration of Oral Health and Primary Care Practice and the Oral Health Delivery Framework models focus on improving access to care by providing risk assessment, caries prevention, patient education, and referrals for patients in smaller towns receiving services in safety net settings, using interprofessional practice collaborations. Oral Health Delivery Framework sites successfully integrated oral health screenings and fluoride varnish application into medical visits, followed by a dentist referral. Oral health education for patients, and continuous maintenance and care are crucial for preventing periodontal diseases. The implementation of dental scaling led to an increase in the percentage of adults with healthy periodontal tissues. No set standards have been defined for scaling. Thus, dentists and dental hygienists usually choose to scale with ultrasound scalers, except in situations in which their use might be restricted. Caries also can be prevented by limiting bottle feeding, avoiding feeding young children sugar-sweetened beverages (SSBs)and ultra-processed snacks, brushing children‘s teeth with fluoride toothpaste starting in infancy, applying topical dental fluoride varnish, and ensuring dental screening and treatment. Using Tele dentistry is a novel part of patient care that is rapidly rising in popularity and significance. Virtual consultations are a simple method to communicate with your dentist from the comfort of your home [43].
Conclusion
Oral diseases are the most prevalent diseases globally and have serious health and economic burdens. Global oral health aims to provide optimal oral health for all and to eradicate global health inequalities via health promotion, disease prevention, appropriate oral care strategies and recognize that oral health is integral to overall health. Establishing good oral health behaviours in childhood is essential to good oral heath across the life course. There is a gaps in oral health knowledge, attitudes, and practices, which warrants a need for enhancing the oral health awareness. The government implemented a health policies and oral health care programmes that help maintain adequate oral and general health. These programmes have a positive feedback for the public and dental service providers as well. There is a directed messages to different groups especially; preschool age children, Elder patients, pregnant, patient compromised with systemic diseases.
Recommendations
The Eatwell Guide encourages us to dietary recommendations:
• Eat at least 5 portions of a variety of fruit and vegetables
every day
• Base meals on potatoes, bread, rice, pasta and other
starchy carbohydrates, choosing wholegrain versions where
possible
• Drink plenty water help maintain immunity and general
health
• Have some dairy or dairy alternatives (such as soy drinks);
choosing lower fat and lower sugar options
• Eat some beans, pulses, fish, eggs, meat and other proteins
(including 2 portions of fish every week, 1 of which should be
oily)
• Choose unsaturated oils and spreads and eat in small
amounts
• Drink 6 to 8 cups or glasses of fluid a day
• If consuming foods and drinks high in fat, salt or sugar,
have these less often and in small amount
Acknowledgement
None.
Acknowledgement
No conflict of interest.
References
- Mahase E (2020) Covid-19: What do we know about “long covid‘? BMJ 370: m2815.
- Chamorro Petronacci C, Martin Carreras Presas C, Sanz Marchena A, Rodríguez Fernández AM, María Suárez Quintanilla J et al. (2020) Assessment of the Economic and Health-Care Impact of COVID-19 (SARS-CoV-2) on Public and Private Dental Surgeries in Spain: A Pilot Study. Int J Environ Res Public Health 17: 5139.
- Knorst JK, Sfreddo CS, de F Meira G (2021) Socioeconomic status and oral health-related quality of life: A systematic review and meta-analysis. Community Dent Oral Epidemiol 49(2): 95-102.
- Institute of Medicine, National Research Council (2011) Improving Access to Oral Health Care for Vulnerable and Underserved Populations. Washington, DC: National Academies Press.
- Hakeem FF, Sabbah W (2019) Is there socioeconomic inequality in periodontal disease among adults with optimal behaviours. Acta Odontol Scand 77: 400-407.
- Naito M, Yuasa H, Nomura Y, Nakayama T, Hamajima N, et al. (2006) Oral Health Status and Health-Related Quality of Life: A Systematic Review. J Oral Sci 48: 1-7.
- Fang WL, Jiang MJ, Gu BB, Wei YM, Fan SN, et al. (2018) Tooth Loss as a Risk Factor for Dementia: Systematic Review and Meta-Analysis of 21 Observational Studies. BMC Psychiatry 18: 345.
- Hung M, Moffat R, Gill G, Lauren E, Ruiz Negrón B, et al. (2019) Oral health as a gateway to overall health and well-being: Surveillance of the geriatric population in the United States. Spec Care Dent 39: 35-361.
- Linden GJ, Herzberg MC, Working Group 4 of the Joint EFP/AAP Workshop (2013) Periodontitis and systemic diseases: A record of discussions of working group 4 of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol 84: S20-S23.
- Bui FQ, Almeida da Silva CLC, Huynh B, Trinh A, Liu J, et al. (2019) Association between periodontal pathogens and systemic disease. Biomed J 42: 27-35.
- Fine N, Chadwick JW, Sun C, Parbhakar KK, Khoury N, et al. (2021) Periodontal inflammation primes the systemic innate immune response. J Dent Res 100: 318-325.
- Vieira KA, Rosa Júnior LS, Souza MAV, Santos NB, Florêncio TMMT, et al. (2020) Chronic Malnutrition and Oral Health Status in Children Aged 1 to 5 Years: An Observational Study. Medicine 99: e19595.
- Conde WL, Monteiro CA (2014) Nutrition Transition and Double Burden of Undernutrition and Excess of Weight in Brazil. Am J Clin Nutr 100: 1617S-1622S.
- Pitts NB, Zero D (2016) White Paper on Dental Caries Prevention and Management; FDI World Dental Federation: Geneva, Switzerland. p. 3-9.
- Olsen I, Yamazaki K (2019) Can Oral Bacteria Affect the Microbiome of the Gut? J Oral Microbiol 11: 1586422.
- World Health Organization (2015) WHO Global Strategy on People-Centred and Integrated Health Services: Interim Report; World Health Organization: Geneva, Switzerland.
- Van der Putten GJ (2020) The association between oral and general health editor. In: Kossioni AE (ed.), Gerodontology essentials for health care professionals. Switzerland AG: Springer Nature p. 49-65.
- Dal Canto E, Ceriello A, Rydén L, Ferrini M, Hansen TB, et al. (2019) Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol 26 (Suppl S2): 25-32.
- Romandini M, Baima G, Antonoglou G, Bueno J, Figuero E, et al. (2021) Periodontitis, Edentulism, and Risk of Mortality: A Systematic Review with Meta-analyses. J Dent Res 100(1): 37-49.
- Mensi M, Scotti E, Sordillo A, Agosti R, Calza S (2020) Plaque disclosing agent as a guide for professional biofilm removal: A randomized controlled clinical trial. Int J Dent Hyg 18: 285-294.
- Tynan A, Walker D, Tucker T, Fisher B, Fisher T (2020) Factors influencing the perceived importance of oral health within a rural Aboriginal and Torres Strait Islander community in Australia. BMC Public Health 20: 514.
- ABIM Foundation ACP-ASIM Foundation; European Federation of Internal Medicine (2002) Medical professionalism in the new millennium: A physician charter. Ann Intern Med 136: 243-246.
- Beauchamp TL, Childress JF (2001) Principles of Biomedical Ethics; Oxford University Press: New York, NY, USA.
- Selgelid MJ (2009) A moderate pluralist approach to public health policy and ethics. Public Health Ethics 2: 195-205.
- Bernstein JT, Franco Arellano B, Schermel A, Labonté MÈ, Abbé MRL (2017) Healthfulness and nutritional composition of Canadian prepackaged foods with and without sugar claims. Appl Physiol Nutr Metab 42: 1217-1224.
- Popova L (2016) Sugar Sweetened Beverage Warning Labels: Lessons Learned from the Tobacco Industry. J Calif Dent Assoc 44: 633-640.
- Wickramage K, Vearey J, Zwi AB, Robinson C, Knipper M (2018) Migration and health: A global public health research priority. BMC Public Health 18: 987.
- Baskaradoss JK (2018) Relationship between oral health literacy and oral health status. BMC Oral Health 18: 172.
- Ramji R, Carlson E, Brogårdh Roth S, Olofsson AN, Kottorp A, et al. (2020) Understanding behavioral changes through community-based participatory research to promote oral health in socially disadvantaged neighborhoods in Southern Sweden. BMJ Open 10: e035732.
- Ministry of Health (2015) National Oral Health Survey of Preschool Children; Oral Health Division (2017) Federal Territory of Putrajaya, Malaysia.
- Ministry of Health (2011-2020) National Oral Health Plan for Malaysia; Oral Health Division (2010) Federal Territory of Putrajaya, Malaysia.
- Tuncer E, Darby I (2021) Knowledge and attitudes towards periodontal health among Australians diagnosed with diabetes. Aust J Prim Health 27: 509-513.
- Cianetti S, Pagano S, Nardone M, Lombardo G (2020) Model for Taking Care of Patients with Early Childhood Caries during the SARS-CoV-2 Pandemic. Int J Environ Res Public Health 17: 3751.
- Lee KH, Kim BY, Kim CJ, Son JY, Song YJ, et a. (2017) Factors affecting oral health care and toothbrush use in adults. J Korean Soc Dent Hyg 17: 1081-1094.
- CDC announces medical-dental integration partnership (2022) Centers for Disease Control and Prevention.
- Deng X, Wang YJ, Deng F, Liu PL, Wu Y (2018) Psychological well-being, dental esthetics, and psychosocial impacts in adolescent orthodontic patients: a prospective longitudinal study. Am J Orthod Dentofac Orthop 153(1): 87-96.e2.
- Koo S, Cho J, Ahn E, Cho S, Park HY (2016) Use of health information among older adults: Trust and source of health information by gender and region. Health Social Welf Rev 36: 454-479.
- Simpson DD (2011) A framework for implementing sustainable oral health promotion interventions. J Public Health Dent 71: S84-S94.
- Public Health England (2020) Improving oral health: guideline development manual. London: PHE.
- Harnagea H, Lamothe L, Couturier (2018) From theoretical concepts to policies and applied programmes: the landscape of integration of oral health in primary care. BMC Oral Health 18(1): 23.
- Janakiram C, Dye BA (2020) A public health approach for prevention of periodontal disease. Periodontol 2000 84: 202–214.
- Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, et al. (2018) High-Quality Health Systems in the Sustainable Development Goals Era: Time for a Revolution. Lancet Glob Health 6: e1196-e1252.
- Schmeler MR, Schein RM, McCue M, Betz K (2009) Telerehabilitation clinical and vocational applications for assistive technology: Research, opportunities, and challenges. Int J Telerehabil 1(1): 59-72.
-
Shaymaa Hussein Rafat kotb*. Implications of Oral Health Policy Consequent Covid19. On J Dent & Oral Health. 6(4): 2023. OJDOH.MS.ID.000644.
-
Oral health, Dentistry, Oral disease, Oral hygiene, Dental education, Oral healthcare services, Dental practice, Periodontal diseases, Root caries, Dental care
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






