 Research Article
Research Article
Does the Pediatric Dentistry Know About Sensory Processing Disorder? An Integrative Review
Christiana Flávia Fontan Roriz1*, Thadeu Roriz Silva Cruz2, Victor Cavallaro Bottesini3 and Danilo Antonio Duarte4
1DDS, MSc. Department of Pediatric Dentistry, São Leopoldo Mandic College. Campinas-SP, Brazil
2DDS, MSc. Department of Pediatric Dentistry, São Leopoldo Mandic College. Campinas-SP, Brazil
3Master’s student. Department of Restorative Dentistry, São Paulo State University. São José dos Campos-SP, Brazil
4PhD, DDS, MSc. Department of Pediatric Dentistry, São Leopoldo Mandic College. Campinas- SP, Brazil
Christiana Flávia Fontan Roriz, DDS, MSc. Department of Pediatric Dentistry, São Leopoldo Mandic College. Campinas-SP, Brazil.
Received Date:February 23, 2023; Published Date:February 28, 2023
Abstract
Background:Sensory processing disorder (SPD) is a limitation or difficulty in the interpretation of sensory information with reflection in the daily activities of an individual. Its clinical manifestations are represented by decreased social interaction, crying, sleep and changes in eating habits. Dental settings and clinical interventions, particularly in children, may contribute to triggering or exacerbating SPD.
Methods and Results: An integrative review (IR) was performed to evaluate the knowledge of pediatric dentistry about SPD.
Conclusion: It was possible to infer that pediatric dentistry has little knowledge on the subject and that studies and literature reviews with strong scientific evidence should be conducted to encourage the use of SPD in pediatric dentistry.
Keywords:Pediatric dentistry; Autistic disorder; Sensation disorders; Review
Introduction
Sensory processing is a function that organizes and modulates the information captured by the senses, giving the individual the ability to perform executive functions. In this context, sensory sensitivity regulates and manages its own responses to different types of sensory stimuli, such as visual, auditory, tactile, olfactory and proprioceptive stimuli [1].
Sensory processing disorder (SPD) refers to a limitation or difficulty in the interpretation and/or use of sensory information to regulate physiological, motor, affective and attention responses, with a negative impact on the individual’s daily activities [2].
The clinical manifestations of SPD are predominantly represented by crying and changes in eating and sleeping habits. Particularly in children, there is a remarkable decrease in social interaction, low self-esteem and low self-confidence, which may persist into adulthood [3].
Associating sensory sensitivity, SPD and its clinical manifestations with pediatric dentistry practice, it is reasonable to assume that the office environment may trigger SPD child, given that the presence of equipment unfamiliar to the child, excessive light, unusual odors, medications and the physical contact of the professional [4].
In addition, dentists have little knowledge of the sensory changes in children and how these changes produce resistance to pediatric dental procedures, resulting in unresponsive or disruptive behavior [5]. Although there is evidence of sensory processing changes caused during dental procedures and understanding this topic is essential for appropriate clinical management, relatively few studies have been conducted.
Thus, the primary objective of the present study was to evaluate, discuss and summarize the level of knowledge of pediatric dentists about SPD and its impact on clinical interventions.
Methods
This integrative literature review was based on the following guiding question: “Is pediatric dentistry aware of sensory processing disorder?”
To answer the question, the following phases were observed: definition of the guiding question, search for relevant and related studies, selection of articles based on the inclusion criteria, preparation and analysis of data. The IR presentation was designed with respect to the required parameters and quality indicators [6].
The databases used were the US National Library of Medicine (PubMed), Scientific Electronic Library Online (SciELO), Latin American and Caribbean Health Sciences Literature (LILACS), Medical Literature Analysis and Retrieval System Online (MEDLINE) and the Portal of Periodicals of the Coordination for the Improvement of Higher Education Personnel (CAPES).
The descriptors “pediatric dentistry”, “autistic spectrum”, and “sensoriality” were used, associating them with the Boolean operators OR and AND, with the aim of involving as many publications as possible. We included full articles in English and Portuguese that directly addressed the guiding question. Articles that did not correspond to the guiding question and those whose methodological designs were opinion articles, letters, editorials, theses, dissertations and guidelines were excluded. The time frame for publication was begun in 2013, which was the likely period of the first articles that addressed sensory processing disorder and its consequences for the individual. Data extraction and analysis were performed by the principal investigator. Any questions were resolved by consensus among the study coauthors.
Results
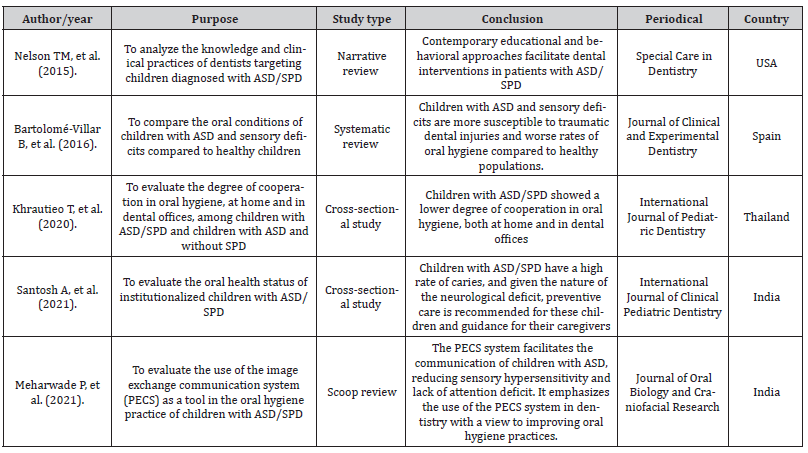
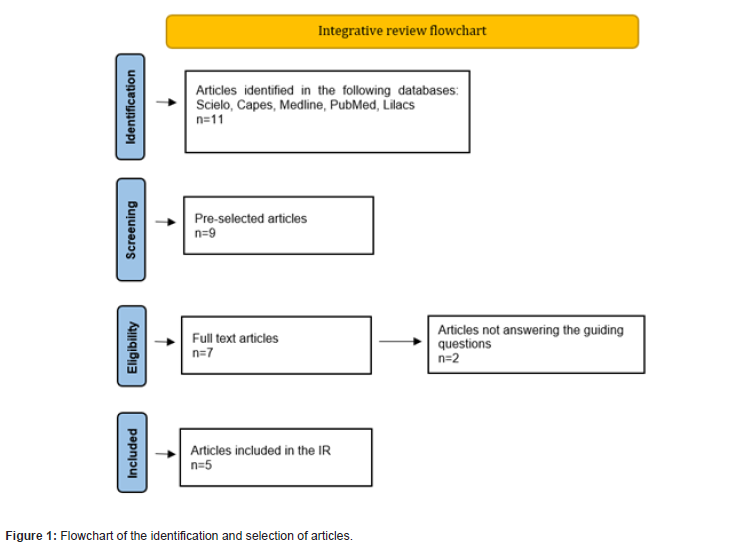
The search of the databases identified 11 potentially eligible articles. The reading of titles included 9 articles, and two were excluded. Based on the reading of abstracts, two other articles were excluded. Two of the remaining 7 were excluded because they did not address the guiding question. Thus, 5 articles were selected for analysis (Figure 1) (Table 1).
Table 1:Articles identified for final composition, according to Roriz CFF/2023.
Discussion
The present IR clearly shows that to date, only five articles directly link PSD and clinical practices to pediatric dentistry [1, 7-10]. Nevertheless, all articles specifically discuss autism spectrum disorder (ASD), although some studies associate SPD with other diagnoses, such as attention deficit hyperactivity disorder (ADHD), Down syndrome and anxiety [11-15].
Thus, an objective and clear answer to the guiding question of the research is not possible. In any case, a careful reading of the selected articles [1, 7-10] allows for an inference that SPD is not a subject of extensive knowledge or research in the field of pediatric dentistry.
Nevertheless, from the perspective of SPD related to pediatric dentistry, there is a lack of multiple and independent studies with methodological designs inserted in the criteria of levels of scientific evidence, revealing a relevant limitation of the present study.
Nevertheless, in the analysis of the mapped and selected studies, there is a concern about the challenges faced by pediatric dentists in relation to SPD, as well as strategies that can minimize its adverse effects [1, 7-10].
It is unquestionable that SPD exacerbates the degree of stress and the level of anxiety of children diagnosed with ASD; the sensory particularities of these children limit their adaptability to hospital and dental environments [16, 17]. Thus, SPD acts as a limiting factor for health professionals and especially for those unaware of these concepts [4].
The development of strategies to create a sensorially adapted dental environment with the help of occupational therapy is essential to overcome these difficulties [18, 19].
In the arsenal of possible strategies, the use of the image exchange communication system (PECS) has been a possibility and strongly recommended in sociocommunicative training for children with ASD [20]. Additionally, a closer relationship between parents/ caregivers and the dental team would enable the family to become promoters of the health of their children [20].
It is important to recognize that dentists require training and prior knowledge to implement adaptations and strategies in their daily practice to address the treatment needs of this group of children [1, 9]. The articles selected in this review did not present a standardized methodology or SPD evaluation tools, which limited an impartial answer to the guiding question. However, this study is relevant due to its probable originality. This is a pioneer study in associating DPT with the knowledge of health professionals in the field of dentistry.
Future studies should be encouraged to help reduce the limitations of the pediatric dentistry approach to children with SPD.
Conclusion
The present study allows us to infer that pediatric dentists have little knowledge about SPT. Therefore, it is urgent to deepen the research and literature on this subject, especially studies conducted with strong levels of evidence that can support the effectiveness of pediatric dentistry actions against the demands of this population.
The permanent search for this knowledge will certainly contribute to clinical decision-making and intervention strategies, from the public and private perspectives, strengthening and creating health promotion skills for these children.
Acknowledgement
None.
Conflict of Interest
The authors declare no conflicts of interest.
References
- Meharwade P, Nookala H, Kajjari S, Malavalli P (2021) Bridging the communication gap in autistic children, one picture at a time. J Oral Biol Craniofacial Res 11(4): 507-510.
- Barton EE, Reichow B, Schnitz A, Smith IC, Sherlock D (2015) Research in Developmental Disabilities Review article A systematic review of sensory-based treatments for children with disabilities. Research in Developmental Disabilities 37: 64-80.
- Machado ACC de P, Oliveira SR de, Magalhães L de C, Miranda DM de, Bouzada MCF (2017) Sensory Processing During Childhood in Preterm Infants : A Systematic Review. Rev Paul Pediatr 35(1): 92-101.
- Cermak SA, Duker LIS, Williams ME, Lane CJ, Dawson ME, et al. (2015) Children With Autism. 69(3).
- Silva ACM da, Costa IM de J, Cardoso JP, Pereira VA de S (2021) Approach and Management of Sensory Alterations in Tea Patients in Dental Treatment. Rev Dialogues in Health 4(2): 13-24.
- Toronto CE, Remington R. A Step-by-Step Guide to Conducting an Integrative Review.
- Nelson TM, Sheller B, Friedman CS, Bernier R (2015) Educational and therapeutic behavioral approaches to providing dental care for patients with Autism Spectrum Disorder. Spec Care Dentist 5: 105-113.
- Bartolomé villar B, Mourelle martínez MR (2016) Incidence of oral health in paediatric patients with disabilities : Sensory disorders and autism spectrum disorder. Systematic review II. J Clin Exp Dent 8(3): e344-351.
- Santosh A, Kakade A, Takate V, Deshmukh B, Juneja A (2021) Oral Health Assessment of Children with Autism Spectrum Disorder in Special Schools. Int J Clin Pediatr Dent 14(4): 548-553.
- Khrautieo T (2020) Association of sensory sensitivities and toothbrushing cooperation in autism spectrum disorder. Int J Paediatr Dent 30(4): 505-513.
- Atlanta, GA UC for DC and PCDC (2018) Centers for Disease Control and Prevention (CDC) Data & Statistics. Autism Spectr Disord.
- Stein LI, Melissa D, Polido JC, Cermak SA, Lane CJ (2022) Association between oral care challenges and sensory responsivity in children with Down syndrome. Int J Paediatr Dent 32(4): 546-557.
- Duker LIS, Grager M, Giffin W, Hikita N (2022) The Relationship between Dental Fear and Anxiety , General Anxiety/Fear , Sensory Over-Responsivity, and Oral Health Behaviors and Outcomes: A Conceptual Model. Int J Environ Res Public Health 19(4): 2380.
- Duker LIS, Richter M, Lane CJ, Polido JC, Cermak SA (2021) Oral Care Experiences and Challenges for Children with Down Syndrome: Reports from Caregivers. Pediatr Dent 42(6): 430-435.
- Lane SJ, Reynolds S, Lane SJ (2019) Sensory Over-Responsivity as an Added Dimension in ADHD. Front Integr Neurosci 13: 1-12.
- Thomas N, Blake S, Morris C, Moles DR (2018) Autism and primary care dentistry : parents ’ experiences of taking children with autism or working diagnosis of autism for dental examinations 226-238.
- Fallea A, Zuccarello R, Roccella M, Quatrosi G, Donadio S, et al. (2020) Sensory-Adapted Dental Environment for the Treatment of Patients with Autism Spectrum Disorder. Children (Basel) 9(3): 393.
- GK, Carrico C, Ivey C, Otr L, PBW (2019) Impact of sensory adapted dental environment on children with developmental disabilities. Spec Care Dentist 180-187.
- Alshatrat SM, Al-bakri IA, Al-omari WM (2020) Dental Service Utilization and Barriers to Dental Care for Individuals with Autism Spectrum Disorder in Jordan : A Case-Control Study.
- Batayneh OB Al, Khader TSNYS (2020) Effectiveness of a tooth‑brushing programme using the picture exchange communication system ( PECS ) on gingival health of children with autism spectrum disorders. Eur Arch Paediatr Dent 21(2): 277-283.
-
Christiana Flávia Fontan Roriz*, Thadeu Roriz Silva Cruz, Victor Cavallaro Bottesini and Danilo Antonio Duarte. Does the Pediatric Dentistry Know About Sensory Processing Disorder? An Integrative Review. On J Dent & Oral Health. 6(5): 2023. OJDOH. MS.ID.000648.
-
Pediatric dentist, Sensory processing disorder, Dental settings, Dentists, Pediatric dentistry, Dental team, Dentistry, Dental environments, Spectrum disorder, Dental procedures.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






