 Perspective
Perspective
Transforming Cardiac Intervention: Plant-Based Diets Are the Game Changer Post-Drug-Coated Balloon Angioplasty
Dasaad Mulijono*
Department of Cardiology, Bethsaida Hospital, Tangerang, Indonesia
Dasaad Mulijono, Department of Cardiology, Bethsaida Hospital, Tangerang, Indonesia
Received Date: July 25, 2025; Published Date: August 08, 2025
Abstract
Restenosis remains a formidable clinical challenge following coronary artery interventions, significantly impacting patient outcomes and healthcare resources. This review highlights the critical role of Whole-Food Plant-Based Diets (WFPBD) in preventing restenosis, specifically emphasizing its superior efficacy following Drug-Coated Balloon (DCB) angioplasty compared to Drug-Eluting Stent (DES) implantation. While DES interventions are associated with persistent inflammatory responses, chronic allergic reactions, and biomechanical disturbances due to the use of permanent metallic scaffolds, DCB therapy uniquely maintains physiological arterial geometry. It minimizes vascular inflammation, creating an optimal environment for dietary interventions. WFPBD’s potent anti-inflammatory, antioxidative, and endothelial restorative properties synergistically complement the biological advantages of DCB. Dietary nitrates and polyphenols, abundant in PBD, significantly enhance endothelial function and nitric oxide (NO) bioavailability, which are vital for vascular recovery and integrity. Additionally, the metabolic benefits of WFPBD - including improved lipid profiles, increased insulin sensitivity, and optimized body weight - further reduce vascular stress, promoting sustainable arterial health after intervention.
Clinical experiences, notably those from Bethsaida Hospital in Indonesia, led by Prof. Dasaad Mulijono, have demonstrated remarkable outcomes. Combining DCB with aggressive plant-based dietary management achieved restenosis rates below 2% at five years, starkly contrasting with the higher restenosis rates (10–20%) typically observed after DES implantation. Leveraging artificial intelligence (AI) to deliver personalized nutritional guidance, the hospital has documented significant improvements in patient adherence and health metrics, including normalization of blood pressure, substantial weight reduction, optimized lipid control, stabilized renal function, and effective diabetes management. This provocative synthesis underscores the pressing need for the broader adoption of integrative lifestyle medicine approaches in cardiology. It advocates for combining DCB angioplasty and WFPBD as the new standard in preventing restenosis and enhancing cardiovascular care.
Keywords: Restenosis; drug-coated balloon; drug-eluting stent; whole-food plant-based diet; inflammation; endothelial dysfunction; Bethsaida Hospital; Prof. Dasaad Mulijono
Introduction
Coronary artery disease (CAD) remains the leading cause of morbidity and mortality worldwide [1,2], with percutaneous coronary intervention (PCI) widely employed to restore adequate blood flow. Despite significant technological advancements, restenosis - recurrent narrowing of arteries post-intervention— continues to challenge clinicians, adversely affecting patient prognosis and healthcare economics. The prevalent use of DES has been instrumental in reducing acute restenosis rates compared to bare-metal stents; however, long-term complications, such as persistent inflammation, allergic reactions, and altered vascular geometry due to the presence of permanent foreign materials, significantly undermine their sustained effectiveness [3-5]. In contrast, DCB angioplasty has emerged as a promising alternative, offering similar or superior short-term efficacy without the prolonged inflammatory burden or geometric disruption caused by permanent implants. By avoiding the presence of metallic scaffolds and polymer coatings, DCB significantly reduces the chronic inflammatory stimulus and maintains natural vessel geometry, which are crucial factors in the pathogenesis of restenosis [6-9].
Concurrently, nutritional interventions, particularly WFPBD, have garnered increasing recognition for their profound influence on cardiovascular health. These diets are inherently antiinflammatory, rich in antioxidants, and conducive to endothelial health, directly addressing the mechanisms underlying restenosis [10-14]. Recent clinical insights reveal that integrating WFPBD post-DCB interventions yields exceptional clinical outcomes, substantially reducing restenosis rates compared to conventional DES implantation. This comprehensive review aims to elucidate the mechanistic synergies between DCB angioplasty and plantbased dietary interventions, presenting robust clinical evidence supporting their combined application. By advocating this integrated approach, the review seeks to inform clinical practices, stimulate further research, and ultimately improve long-term patient outcomes in cardiovascular disease management (Figure 1).
Distinct Mechanisms of Restenosis in DES and DCB Interventions
Persistent Inflammation and Allergic Reactions Post-
DES
DES implantation involves the use of permanent metal scaffolds and polymer coatings, which can provoke chronic inflammatory responses, delayed hypersensitivity reactions, and persistent eosinophilic infiltration. These reactions perpetuate inflammatory stimuli, promoting restenosis and late stent thrombosis [4,15-20].
Geometric Distortions and Flow Disturbances Induced
by DES
The permanent metallic scaffold of DES disrupts natural arterial geometry, creating areas of disturbed, turbulent blood flow and reduced laminar shear stress. These biomechanical alterations significantly enhance endothelial injury, inflammation, platelet aggregation, and neointimal proliferation, driving restenosis [21- 23].
Advantages of DCB: Natural Vessel Geometry and
Minimal Inflammation
Unlike DES, DCB angioplasty delivers anti-proliferative drugs without leaving a permanent foreign body. Consequently, DCB preserves natural arterial geometry, maintains physiological laminar blood flow, minimizes chronic inflammation, and reduces allergic potential, thereby substantially lowering the risk of restenosis [24-28].
The Enhanced Effectiveness of WFPBD Post-DCB
WFPBD substantially amplifies the effectiveness of DCB interventions through several integrated physiological and biochemical mechanisms. WFPBD significantly reduces systemic and local vascular inflammation by decreasing inflammatory cytokines, such as IL-6, TNF-alpha, and hs-CRP, thereby complementing the inherently low inflammatory profile of DCB and markedly diminishing the risk of restenosis. Concurrently, plantbased diets rich in dietary nitrates (e.g., leafy greens and beets) enhance NO availability, which is essential for endothelial repair and vasodilation, thereby optimizing endothelial regeneration post- DCB. Additionally, the high antioxidant content of plants, including polyphenols, flavonoids, and vitamins, mitigates oxidative stress by neutralizing reactive oxygen species (ROS), thereby preventing neointimal hyperplasia and reinforcing vascular integrity [29-31]. Metabolically, WFPBD improves lipid profiles, reduces insulin resistance, and supports weight management, thereby minimizing vascular stressors that contribute to restenosis. Moreover, a WFPBD counters the detrimental effects of unhealthy diets, such as endothelial dysfunction, oxidative stress, hypertension, and systemic inflammation, through antioxidative, anti-inflammatory, and metabolic regulatory actions.
It enhances endothelial function and blood pressure regulation by leveraging dietary nitrates, antioxidants, and electrolyte balance. Further, a WFPBD optimizes lipid profiles by promoting fibre-induced cholesterol reduction, beneficial fatty acids, and gut microbiome-mediated cholesterol metabolism, while preventing harmful LDL-C elevation and HDL oxidation. Weight management is supported via reduced caloric density, dietary fibre-driven satiety, and improved glycaemic control. Additionally, PBDs enhance insulin sensitivity and blood glucose regulation through fibre-rich dietary interventions, polyphenol-mediated improvements to the insulin receptor, and modulation of the gut microbiota. Systemic inflammation and oxidative stress are effectively attenuated by polyphenols, antioxidants, and omega-3 fatty acids, thereby fostering a robust gut microbiota that produces short-chain fatty acids (SCFAs), which are vital for cardiovascular health. Furthermore, WFPBD enhances mitochondrial efficiency by stimulating mitochondrial biogenesis, reducing oxidative stress, and optimizing cellular energy metabolism. Ultimately, reduced oxidative stress, enhanced DNA repair mechanisms, and metabolic stability contribute to the preservation of telomeres and longevity. Collectively, these mechanisms position WFPBD as a critical dietary intervention for cardiovascular health, significantly improving clinical outcomes after DCB.
Clinical Evidence Supporting DCB and WFPBD Integration
Clinical experiences from a pioneering centre, notably Bethsaida Hospital in Indonesia, led by Prof. Dasaad Mulijono, have demonstrated significantly lower restenosis rates (<2% at five years) with the integration of DCB therapy and aggressive WFPBD management, compared to higher restenosis rates (10– 20%) typically observed with DES interventions. This difference highlights the detrimental effects of persistent inflammatory responses and geometric disturbances associated with DES. At Bethsaida Hospital, we have utilized AI to enhance patient education, deliver evidence-based dietary guidance, and provide personalized meal plans for patients with cardiovascular conditions. This approach has significantly improved patient adherence to WFPBD, resulting in notable improvements in overall health outcomes. Clinically, our patients with hypertension frequently achieve sustained blood pressure normalization, allowing them to discontinue antihypertensive medications. Overweight patients have successfully attained healthy body mass indices (BMI of 21– 22).
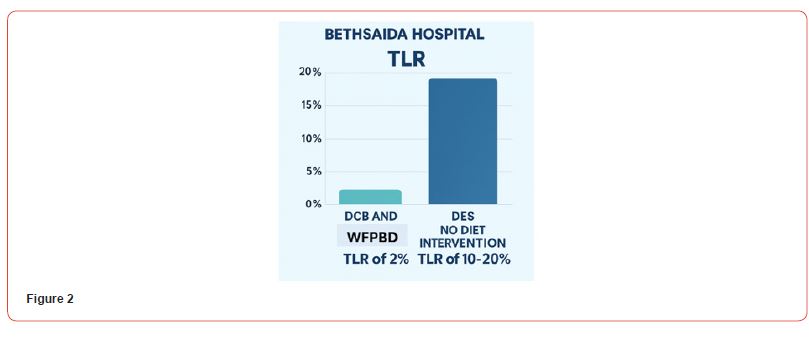
At the same time, those with hyperlipidaemia have consistently reached target LDL-C levels below 30 mg/dL through a combination of WFPBD, high-intensity statins, and ezetimibe therapy. Furthermore, patients with moderate renal impairment have exhibited normalization of serum creatinine levels, and diabetic patients have achieved substantial glycaemic control, with HbA1c consistently maintained below 6%, often enabling a reduction or cessation of insulin therapy. Remarkably, the restenosis rate among our cardiology patients remains approximately 2% over a two-year follow-up, with substantial evidence of atherosclerotic plaque stabilization and regression. Despite these significant clinical outcomes, broader adoption of lifestyle medicine among medical colleagues remains limited. To bridge this gap, our centre is committed to extensive contributions to scientific literature, aiming to inspire future clinicians to adopt this transformative approach. By integrating lifestyle medicine into mainstream clinical practice, we strive to enhance patient care standards and reduce the prevalence of chronic diseases (Figure 2).
Conclusion
The integration of WFPBD following DCB angioplasty significantly enhances the prevention of restenosis, capitalizing on the distinct biological advantages of DCB, which include minimal inflammatory responses, absence of chronic allergic stimuli, and preservation of natural arterial geometry. Unlike DES, DCB avoids persistent inflammation, chronic allergic reactions, and vascular disturbances associated with permanent implants, thereby creating an optimal physiological environment for dietary interventions. The potent anti-inflammatory, antioxidative, and metabolic benefits inherent in WFPBD synergistically complement the mechanisms underlying DCB efficacy, effectively mitigating key pathological drivers of restenosis such as endothelial dysfunction, oxidative stress, systemic inflammation, and metabolic dysregulation. Clinical evidence, particularly from pioneering institutions such as Bethsaida Hospital, underscores the remarkable clinical outcomes achievable through the combined approach of DCB therapy and aggressive plant-based dietary management. Documented restenosis rates below 2% over two years contrast with higher restenosis rates commonly associated with DES.
Leveraging advanced AI technologies further enhances patient adherence to WFPBD, resulting in sustained clinical improvements, including optimal lipid profiles, stabilized blood pressure, effective weight management, improved glycaemic control, and stabilized renal function. These compelling outcomes strongly advocate for the broader integration of lifestyle medicine into conventional cardiology practices. Ultimately, the combination of DCB angioplasty and WFPBD represents a transformative strategy for cardiovascular care, significantly reducing the risk of restenosis and improving long-term patient prognosis. By adopting this integrative approach, healthcare systems and clinical practitioners can substantially improve the quality of cardiovascular management, promoting sustained arterial health and significantly reducing the global burden of coronary artery disease.
Author Contributions
D.M.; Conceptualization, writing, review, and editing.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflict of Interest
The authors declare no conflict of interest.
References
- Brown JC, Gerhardt TE, Kwon E (2023) Risk Factors for Coronary Artery Disease. Treasure Island (FL): StatPearls Publishing.
- Shahjehan RD, Sharma S, Bhutta BS (2024) coronary artery disease. Treasure Island (FL): StatPearls Publishing.
- Senst B, Goyal A, Basit H, Borger J (2023) Drug Eluting Stent Compounds. Treasure Island (FL): StatPearls Publishing.
- Hu W, Jiang J (2022) Hypersensitivity and in-stent restenosis in coronary stent materials. Front Bioeng Biotechnol 10: 1003322.
- Fu Y, Zhang S, Du H, Li L, Wang C, et al. (2018) Impact of vessel curvature on neointimal healing after stent implantation as assessed by optical coherence tomography. Medicine (Baltimore) 97(16): e0518.
- Iwańczyk S, Wolny R, Januszek R, Gil RJ, Cortese B, et al. (2024) Long-term outcomes of DCB and DES for the treatment of in-stent restenosis in relation to the vessel size. Catheter Cardiovasc Interv 104(6): 1168-1177. Erratum in: Catheter Cardiovasc Interv 105(5): 1278.
- Funayama N, Muratsubaki S, Ito R, Tobisawa T, Konishi T (2023) Drug-coated balloons versus drug-eluting stents for coronary de novo lesions in dialysis patients. Heart Vessels 38(3): 300-308.
- Mutema M, Shenoy V, Sardar P, Parikh S, Chatterjee S (2024) Systematic Review on Role of Drug Eluting Stent (DES) Versus Drug-Coated Balloon (DCB) in Small Vessel Coronary Artery Disease. Curr Cardiol Rep 26(7): 681-688.
- Caminiti R, Vizzari G, Ielasi A, Vetta G, Parlavecchio A, et al. (2024) Drug-coated balloon versus drug-eluting stent for treating de novo large vessel coronary artery disease: a systematic review and meta-analysis of 13 studies involving 2888 patients. Clin Res Cardiol 114(8): 978-990.
- Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, et al. (1998) Intensive lifestyle changes for reversal of coronary heart disease. JAMA 280(23): 2001-2007. Erratum in: (1999) JAMA 281(15): 1380.
- Esselstyn CB Jr, Gendy G, Doyle J, Golubic M, Roizen MF (2014) A way to reverse CAD? J Fam Pract 63(7): 356-364b.
- Tuso P, Stoll SR, Li WW (2015) A plant-based diet, atherogenesis, and coronary artery disease prevention. Perm J. Winter 19(1): 62-67.
- Mehta P, Tawfeeq S, Padte S, Sunasra R, Desai H, et al. (2023) Plant-based diet and its effect on coronary artery disease: A narrative review. World J Clin Cases 11(20): 4752-4762.
- Peña-Jorquera H, Cid-Jofré V, Landaeta-Díaz L, Petermann-Rocha F, Martorell M, et al. (2023) Plant-Based Nutrition: Exploring Health Benefits for Atherosclerosis, Chronic Diseases, and Metabolic Syndrome-A Comprehensive Review. Nutrients 15(14): 3244.
- Taguchi I, Yoneda S, Abe S, Toyoda S, Nasuno T, et al. (2014) The late-phase inflammatory response after drug-eluting stent implantation. Heart Vessels 29(2): 213-9.
- Gogo PB Jr, Schneider DJ, Watkins MW, Terrien EF, Sobel BE, et al. (2005) Systemic inflammation after drug-eluting stent placement. J Thromb Thrombolysis 19(2):87-92.
- Ochijewicz D, Tomaniak M, Opolski G, Kochman J (2021) Inflammation as a determinant of healing response after coronary stent implantation. Int J Cardiovasc Imaging 37(3): 791-801.
- Ozer N, Tangurek B, Firat F, Ozer S, Tartan Z, et al. (2008) Effects of drug-eluting stents on systemic inflammatory response in patients with unstable angina pectoris undergoing percutaneous coronary intervention. Heart Vessels 23(2): 75-82.
- Nakajima Y, Itoh T, Morino Y (2016) Metal allergy to everolimus-eluting cobalt chromium stents confirmed by positive skin testing as a cause of recurrent multivessel in-stent restenosis. Catheter Cardiovasc Interv 87(4): E137-142.
- Kounis NG, Kounis GN, Kouni SN, Soufras GD, Niarchos C, et al. (2006) Allergic reactions following implantation of drug-eluting stents: a manifestation of Kounis syndrome? J Am Coll Cardiol 48(3): 592-3.
- Chinikar M, Sadeghipour P (2014) Coronary stent fracture: a recently appreciated phenomenon with clinical relevance. Curr Cardiol Rev 10(4): 349-54.
- Sakamoto A, Jinnouchi H, Torii S, Virmani R, Finn AV (2018) Understanding the Impact of Stent and Scaffold Material and Strut Design on Coronary Artery Thrombosis from the Basic and Clinical Points of View. Bioengineering (Basel). 5(3): 71.
- Pant S, Bressloff NW, Limbert G (2012) Geometry parameterization and multidisciplinary constrained optimization of coronary stents. Biomech Model Mechanobiol 11(1-2): 61-82.
- Verdoia M, Negro F, Kedhi E, Suryapranata H, Marcolongo M, et al. (2021) Benefits with drug-coated balloon as compared to a conventional revascularization strategy for the treatment of coronary and non-coronary arterial disease: a comprehensive meta-analysis of 45 randomized trials. Vascul Pharmacol 138: 106859.
- Cortese B, Malakouti S, Mazhar W, Leontin Lazar F, Munjal A, et al. (2024) Long-term benefits of drug-coated balloons for coronary artery revascularization. Minerva Cardiol Angiol 72(5): 506-516.
- Korjian S, McCarthy KJ, Larnard EA, Cutlip DE, McEntegart MB, et al. (2024) Drug-Coated Balloons in the Management of Coronary Artery Disease. Circ Cardiovasc Interv 17(5): e013302.
- Jeger RV, Eccleshall S, Wan Ahmad WA, Ge J, Poerner TC, et al. (2020) Drug-Coated Balloons for Coronary Artery Disease: Third Report of the International DCB Consensus Group. JACC Cardiovasc Interv 13(12): 1391-1402.
- Shin ES, Jun EJ, Kim S, Kim B, Kim TH, et al. (2023) Clinical Impact of Drug-Coated Balloon-Based Percutaneous Coronary Intervention in Patients with Multivessel Coronary Artery Disease. JACC Cardiovasc Interv 16(3): 292-299.
- Salehin S, Rasmussen P, Mai S, Mushtaq M, Agarwal M, et al. (2023) Plant Based Diet and Its Effect on Cardiovascular Disease. Int J Environ Res Public Health 20(4): 3337.
- Satija A, Hu FB (2018) Plant-based diets and cardiovascular health. Trends Cardiovasc Med 28(7): 437-441.
- Kaiser J, van Daalen KR, Thayyil A, Cocco MTARR, Caputo D, et al. (2021) A Systematic Review of the Association Between Vegan Diets and Risk of Cardiovascular Disease. J Nutr 151(6): 1539-1552.
-
Dasaad Mulijono*. Transforming Cardiac Intervention: Plant-Based Diets Are the Game Changer Post-Drug-Coated Balloon Angioplasty. On J Cardio Res & Rep. 8(2): 2025. OJCRR.MS.ID.000682.
-
Restenosis; drug-coated balloon; drug-eluting stent; whole-food plant-based diet; inflammation; endothelial dysfunction; bethsaida hospital; prof. dasaad mulijono; iris publishers; iris publishers’ group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
- Abstract
- Introduction
- Distinct Mechanisms of Restenosis in DES and DCB Interventions
- The Enhanced Effectiveness of WFPBD Post-DCB
- Clinical Evidence Supporting DCB and WFPBD Integration
- Conclusion
- Author Contributions
- Institutional Review Board Statement
- Informed Consent Statement
- Data Availability Statement
- Conflict of Interest
- References






