 Case Report
Case Report
Takotsubo Cardiomyopathy Following Propofol Induction in an Elderly Female Undergoing Coronary Intervention
Dasaad Mulijono*
Department of Cardiology, Bethsaida Hospital, Tangerang, Indonesia
Dasaad Mulijono, Department of Cardiology, Bethsaida Hospital, Tangerang, Indonesia
Received Date: August 21, 2025; Published Date: September 02, 2025
Abstract
We present the case of an 83-year-old frail woman with a prior history of coronary intervention who developed Takotsubo (Tako-Tsubo) cardiomyopathy (TTC) immediately following propofol induction for elective percutaneous coronary intervention (PCI). She initially presented with exertional dyspnea and was found to have severe coronary artery stenoses in the mid-right coronary artery (RCA) and mid-left anterior descending artery (LAD) on multi-slice computed tomography (MSCT). Despite optimal medical therapy for two months, her anginal symptoms persisted, prompting coronary angiography and drug-coated balloon (DCB) angioplasty under general anesthesia. Shortly after propofol administration, she developed hypotension, desaturation, sinus tachycardia, and new anterior T-wave inversions. Post-procedure, echocardiography revealed apical ballooning with severely reduced ejection fraction (<30%). Troponin levels were elevated, while CK-MB remained normal. A diagnosis of propofol-induced Takotsubo cardiomyopathy was made. Her course was complicated by acute kidney injury, requiring prolonged inotropic support and medical optimization. She recovered from cardiac and renal dysfunction and was discharged home in a stable condition. This case highlights the potential for propofol to precipitate TTC in vulnerable elderly patients and emphasizes the importance of peri-procedural vigilance.
Keywords: Takotsubo cardiomyopathy; propofol; elderly; coronary intervention; drug-coated balloon angioplasty; acute kidney injury
Introduction
TTC, also known as stress-induced cardiomyopathy or “broken heart syndrome,” is a reversible form of acute heart failure characterized by transient left ventricular systolic dysfunction, often in the absence of significant obstructive coronary artery disease (CAD). The syndrome is typically precipitated by emotional or physical stress, with a catecholamine surge implicated in its pathophysiology. While anesthesia-related TTC is rare, propofol - a commonly used induction agent - has been occasionally reported as a trigger, likely through hemodynamic instability, direct myocardial depression, and sympathetic activation during hypotension. We report a case of propofol-induced TTC in an elderly woman undergoing elective PCI for severe CAD.
Case Report
An 83-year-old frail female presented with a 3-month history of exertional dyspnea, particularly when climbing stairs. Her weight is only 40 kgs with a height of 148 cm, and all of her vital signs werewithin normal values. She had undergone coronary intervention 10 years prior, with stents placed in the mid left circumflex (LCX) and proximal LAD arteries. She had no history of diabetes or dyslipidemia, and her laboratory results revealed normal lipid and glucose levels. Baseline echocardiography demonstrated preserved ejection fraction (EF) and normal valvular function. Chest X-ray was unremarkable. Laboratory studies revealed mildly impaired renal function (creatinine level 1.3 mg/dL, estimated GFR 70 mL/ min/1.73 m²).
She was on a statin and low-dose aspirin. MSCT coronary angiography revealed 80% stenosis in the mid RCA and 90% stenosis in the mid LAD, with patent prior stents in the LCX and proximal LAD. After two months of optimal medical therapy, her anginal symptoms persisted, and she was scheduled for coronary angiography and PCI. Given her significant procedural anxiety, general anesthesia was selected. Pre-induction vital signs were stable: sinus rhythm 72 bpm, BP 120/80 mmHg, oxygen saturation 100%. Induction with intravenous propofol was followed within minutes by hypotension (80/50 mmHg), oxygen desaturation (90%), a burst of atrial fibrillation (rate >100 bpm), and new anterior T-wave inversions. Initial management included fluid resuscitation, followed by dobutamine and norepinephrine, which restored BP to ~100/50 mmHg [1-5].
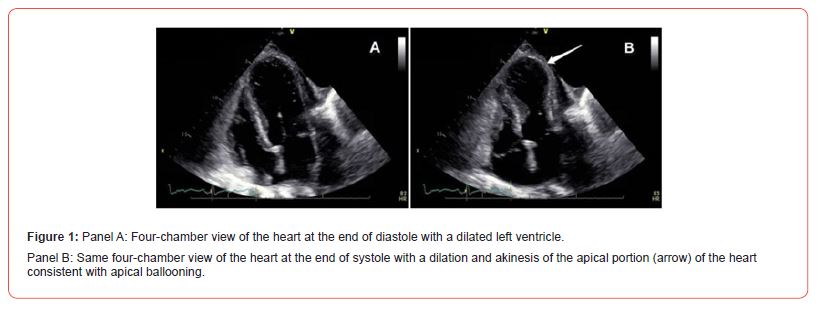
PCI was completed successfully using two DCBs for the mid RCA and mid LAD lesions. Post-procedure, she required moderate inotropic support to maintain systolic BP >100 mmHg. Chest X-Ray consistent with acute heart failure, mild-moderate in severity. Echocardiography revealed apical ballooning and EF <30% (Figure 1). Troponin levels were elevated at four times the upper limit of normal, with normal CK-MB levels. NT-pro-BNP was markedly elevated the following day. She developed acute kidney injury with creatinine peaking at 4 mg/dL (GFR <30 mL/min/1.73m²). The diagnosis of propofol-induced Takotsubo cardiomyopathy was established.
Management included inotropic support, low-dose captopril (2 × 6.25 mg), and ivabradine to maintain heart rate <80 bpm. By day 14, inotropes were discontinued, and renal function gradually improved, returning to baseline by day 18. Repeat Echo on day 14 revealed an EF of 58%. She was discharged on statin, single antiplatelet therapy (due to gastrointestinal bleeding risk, in which she had an episode of hematemesis and melena during this ICCU admission), trimetazidine modified release 35 mg twice daily, and ivabradine 5 mg twice daily. At one-week follow-up, she was stable, and at one month, she reported improved mobility and no recurrence of symptoms [6-10].
Discussion
TTC is characterized by transient systolic dysfunction of the LV apex or mid-ventricle, often precipitated by catecholamine excess in response to stress. It predominantly affects postmenopausal women and is commonly triggered by emotional or physical stressors. In this case, propofol induction likely precipitated the event through rapid hypotension, reduced coronary perfusion, and subsequent sympathetic overdrive.
Propofol is known for its vasodilatory and adverse inotropic effects, which may cause abrupt hypotension. In susceptible individuals, particularly elderly females with CAD, this can trigger myocardial stunning and TTC. The presentation in our patient was atypical in that it occurred immediately after induction and coexisted with obstructive coronary lesions, which were successfully treated.
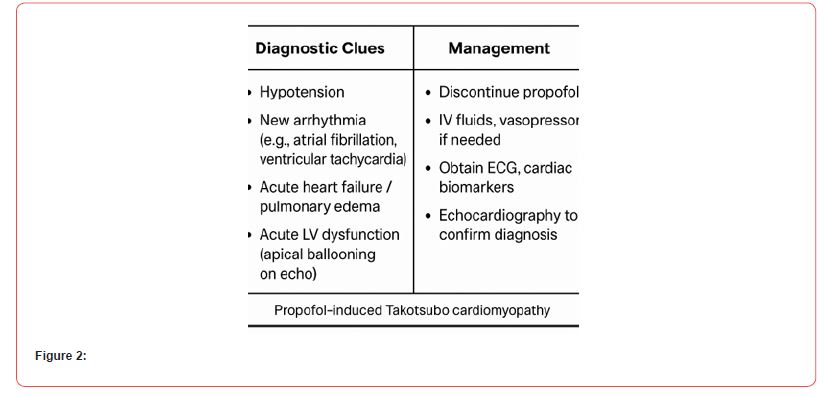
Differentiating TTC from acute myocardial infarction is essential, as management strategies differ. In this case, the absence of a culprit occlusion, the presence of apical ballooning, and the biomarker profile (mildly to moderately elevated troponin with normal to mildly elevated CK-MB and a markedly elevated NT-pro-BNP level) supported the diagnosis of TTC. Complications such as acute kidney injury may occur due to hypotension, low cardiac output, and contrast-induced nephropathy. This case underscores the needfor heightened awareness of TTC as a potential complication of anesthesia induction, particularly in elderly female patients with significant comorbidities. Minimizing peri-induction hemodynamic instability and considering alternative anesthetic approaches may mitigate this risk (Figure 2). The case also highlights the critical role of using DCB in patients with a higher risk of intestinal bleeding, as demonstrated in our case, where a single dose of one antiplatelet agent (Ticagrelor 1 x 90 mg) is sufficient.
Conclusion
Propofol-induced Takotsubo cardiomyopathy is a rare but serious complication in elderly, frail patients undergoing coronary intervention. Early recognition, supportive management, and meticulous perioperative hemodynamic monitoring are crucial for a successful recovery. This case adds to the limited literature on anesthesia-related TTC and highlights the vulnerability of elderly patients to stress-induced cardiac events.
Author Contributions
D.M.; Conceptualization, writing, review, and editing.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflict of Interest
The authors declare no conflict of interest.
References
- Ahmad SA, Khalid N, Ibrahim MA (2023) Takotsubo Cardiomyopathy. StatPearls. Treasure Island (FL): StatPearls Publishing.
- Assad J, Femia G, Pender P, Badie T, Rajaratnam R (2022) Takotsubo Syndrome: A Review of Presentation, Diagnosis and Management. Clin Med Insights Cardiol 16: 11795468211065782.
- Ahmed T, Lodhi SH, Haigh PJ, Sorrell VL (2024) The many faces of takotsubo syndrome: A review. Curr Probl Cardiol 49(3): 102421.
- Del Buono MG, La Vecchia G, Montone RA, Rodriguez-Miguelez P, Leone AM, et al. (2025) The Evolving Features of Takotsubo Syndrome. Curr Cardiol Rep 27(1): 39.
- Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, et al. (2016) Current state of knowledge on Takotsubo syndrome: a Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 18(1): 8-27.
- Bybee KA, Prasad A (2008) Stress-related cardiomyopathy syndromes. Circulation 118(4): 397-409.
- Y-Hassan S, Tornvall P (2018) Epidemiology, pathogenesis, and management of takotsubo syndrome. Clin Auton Res 28(1): 53-65.
- Muthachen NR, Sethuraman M (2017) Anesthetic management of a patient with Takotsubo cardiomyopathy presenting for surgical clipping of intracranial aneurysm. J Anaesthesio Clin Pharmacol 33(4): 547-548.
- (2023) Propofol. Reactions Weekly 1942: 245.
- Dimitriadis K, Pyrpyris N, Iliakis P, Kanatas P, Theofilis P, et al. (2024) Optimal management of high bleeding risk patients undergoing percutaneous coronary interventions: Where do we stand? J Cardiol 85(2): 79-87.
-
Dasaad Mulijono*. Takotsubo Cardiomyopathy Following Propofol Induction in an Elderly Female Undergoing Coronary Intervention. On J Cardio Res & Rep. 8(2): 2025. OJCRR.MS.ID.000684.
-
Takotsubo cardiomyopathy; propofol; elderly; coronary intervention; drug-coated balloon angioplasty; acute kidney injury; iris publications; iris publishers; group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






