 Case Report
Case Report
Retrograde Transcatheter Perforation in Adult with Pulmonary Atresia and Single Ventricle: A Unique Case of Ventricular Outflow Tract Opening
Nicolas Hugues*, Bruno Vare, Carine Dommerc and François Bourlon
Centre Cardio-Thoracique de Monaco, Monaco
Nicolas Hugue, Centre Cardio-Thoracique de Monaco, Monaco.
Received Date:May 07, 2021; Published Date:May 25, 2021
Abstract
Radiofrequency-assisted perforation and subsequent balloon dilatation technique is accepted for treating pulmonary stenosis and pulmonary atresia in patients with intact interventricular septum, but its high cost limits the widespread use. Perforation of the atretic pulmonary valve using the stiff end of a coronary wire seems to be an effective alternative to the radiofrequency perforation. We report on a 47-year-old man with a complex cardiopathy including a pulmonary valve atresia, who underwent a partial surgical repair. Due to high surgical risk, a completion could not be foreseen and a percutaneous retrograde perforation of the pulmonary valve was proposed. The perforation was managed by means of BMW wires with stiff tip from the right internal jugular vein because the femoral vein access was not accesible. Following three Armada balloon inflations, an Express stent was properly introduced to keep the ventricular outflow tract (VOT) open. We describe a successful unusual technique of atretic pulmonary valve percutaneous retrograde perforation that can be an efficient alternative when surgery or anterograde percutaneous access are not possible.
Keywords:Transcatheter perforation; Ventricular outflow tract; Coronary guidewire; Atretic pulmonary valve; Stenting; Double outlet ventricle
Abbreviations:PAIVS: Pulmonary Atresia with Intact interVentricular Septum; VOT: Ventricular Outflow Tract; BMW: Balance Middle Weight; CTO: Chronic Total Occlusion; MRI: Magnetic Resonance Imaging
Introduction
Transcatheter perforation of the pulmonary valve is an alternative to treat critical pulmonary stenosis and pulmonary atresia with intact interventricular septum (PAIVS) in neonates [1,2], using radiofrequency-assisted perforation and subsequent balloon dilatation [2-4]. However it requires expertise, is expensive and not available in every center. The usefulness of chronic total occlusion hardware was demonstrated in pulmonary atresia with intact ventricular septum [5-8] or with ventricular septal defect [7]. Previously the use of coronary guidewire with stiff end showed an association with failures and complications [4,5]. Nevertheless, a recent study showed that this technique is probably an effective alternative to radiofrequency wire in resource-limited setting [8]. We drew on this method to treat an atretic pulmonary valve in an adult with a complex congenital heart disease, which underwent a partial surgical repair and for which a Fontan completion was contraindicated because of surgical risks.
Case Presentation
We report on a 47-year-old man who was referred to our Institution for dyspnea on exertion and progressive cyanosais. This patient had a complex cardiopathy with single ventricle, situs solitus, dextrocardia, double inlet left ventricle, pulmonary valve atresia and levo-malposition of great arteries. He underwent several systemico-pulmonary shunts and a termino-lateral superior cavopulmonary anastomosis at the age of 23. Clinical examination revealed a severe cyanosis with oxygen saturation less than 75% and a mild systolic murmur. Sinus rhythm was permanent. The basal echocardiogram showed the complex cardiopathy with a single left ventricle. Aorta was found in front and left-side of the pulmonary artery. A moderate aortic regurgitation was recorded in ascending aorta. Left pulmonary artery could not be analysed and inferior vena cava was connected to the atrium. At the lung scintigraphy an absence of upper left lobe perfusion, with a hypoperfusion of left lower lobe and anterior middle of the right lung was showed. Cardiac catheterization demonstrated a severe aorta desaturation (76%) and low pulmonary pressures (11 mmHg). A cavopulmonary anastomosis complementation was considered, but was not feasible because of dextrocardia and high surgical risk. It was first proposed to test the effect of a transcatheter ventricular outflow tract (VOT) opening on oxygen saturation.
Retrograde transcatheter perforation of ventricular outflow tract opening: first attempt
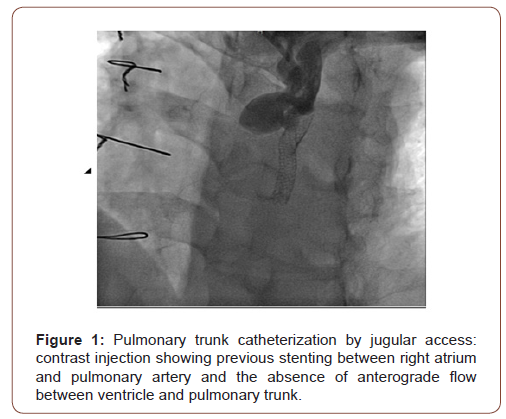
The patient underwent a first percutaneous retrograde procedure that failed. A BMW wireguide was mounted upside down in order to use its rigid distal portion. After perforation, a second flexible wire was introduced in parallel to perform repeated dilatations and stenting (Figure 1). On the contrary to what was foreseen, oxygen saturation did not increase because opening was done through the right atrium and not through the ventricle. Considering the contrast volume required and the duration of the procedure, it was decided to schedule a new intervention. This unsuccessful attempt was complicated by a pulmonary edema managed by intensive care unit.
Retrograde transcatheter perforation of ventricular outflow tract opening : successful procedure
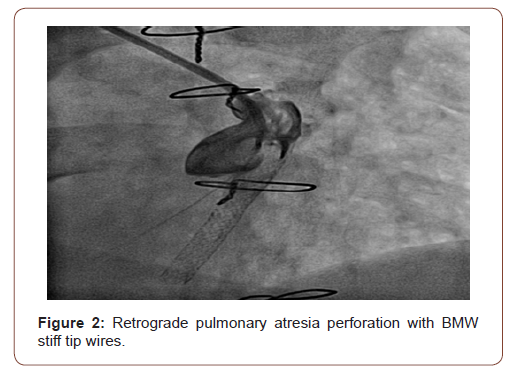
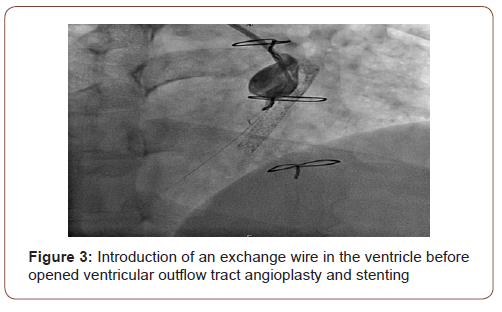
A second percutaneous retrograde procedure was performed under general anesthesia. 7F sheat was introduced into right femoral vein. Because of catheter instability, pulmonary valve perforation from the ventricle was not possible. The right internal jugular vein access across the upper cavo-pulmonary anastomosis was adopted. Right jugular vein and pulmonary artery punctures were carried out with 6F introducers. Several wires with different penetrating power were used. BMW wires with stiff tip were gently manipulated to perforate the pulmonary valve and to enter into the right ventricle using contrast (Figure 2). A 5.0 mm x 20 mm Armada balloon was advanced over an exchange guidewire J0.035 placed in the ventricle. Dilatation was performed three times during 10 seconds with inflation pressure of at least 10 bars. After dilatation, VOT patency was maintained using a stent Express LD 6 mm x 57 mm delivered at 14 bars during 30 seconds (Figure 3). Finally balloon was removed and pressures were checked.
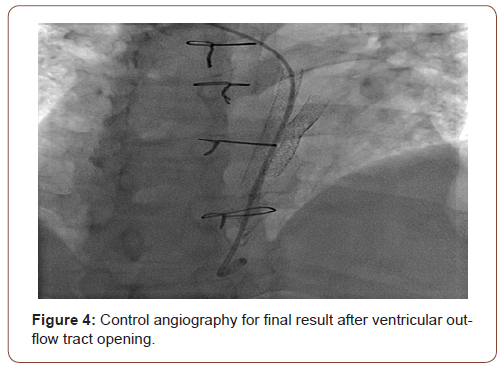
A pigtail catheter placed into the stent was used for angiographic control (Figure 4). Another contrast injection at 25 ccs (15 cc/s) allowed to show ventricular dilatation and perfusion through the aorta and the pulmonary artery. Per-procedure peak oxygen saturation was 90%. Heart rhythm remained sinusal. Oral anticoagulation with Xarelto was introduced in addition to aspirin.
Discussion
We present a difficult case of VOT opening using retrograde transcatheter pulmonary valve perforation. Transcatheter pulmonary valve perforation using radiofrequency or a guidewire were described in neonates or infants, we drew on these techniques [7] to perform a VOT opening on an adult. As surgery was contraindicated for our patient, this technique was therefore a good alternative. Most of published cases of transcatheter pulmonary valve perforation described an anterograde catheterism from right ventricle to main pulmonary artery. In an original way and for reasons of wires stability, we decided to catheterize the internal right jugular vein and to perforate pulmonary valve from the pulmonary trunk to ventricle. Only one example of retrograde crossing of the atretic pulmonary valve was previously described because anterograde approach was not possible [6].
Currently, atretic pulmonary valve mechanical perforations are mainly performed with guidewires adapted for coronary artery chronic total occlusion (CTO) such as: Crossit (Abbott), P-T graphix (Boston), asahi confianza (abbot), Conquest pro (Asahi Intecc), Shinobi (Cordis corporation) and miracle (Abbott) [2,5,8,9]. The use of BMW guidewires not dedicated to CTO was documented in only 3 reported cases (7). CTO guidewire perforation was proved to be safe and efficient [5,6,8], but in most of cases the perforation was eccentric [10]. Recently, the usefulness of microcatheter in perforating the atretic pulmonary valve was reported. Authors showed that the microcatheter facilitates the central perforation and could reduce failures, complications and risk of pulmonary regurgitation [9]. A modified less aggressive technique using a catheter loop and progressive balloon dilatation was carried out successfully on 11 newborns and improves results with mediumterm follow-up [2]. Other studies would be helpful to compare the safety and efficacy of different wires according to their penetrating power.
Radiofrequency remains the reference technique to treat pulmonary valve atresia with intact ventricular septum, but its implementation has a significant cost. More data and experiences from different centers are needed to confirm the accessibility, the safety and the efficacy of mechanical pulmonary valve perforation.
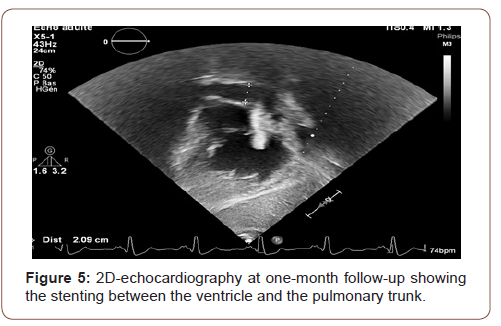
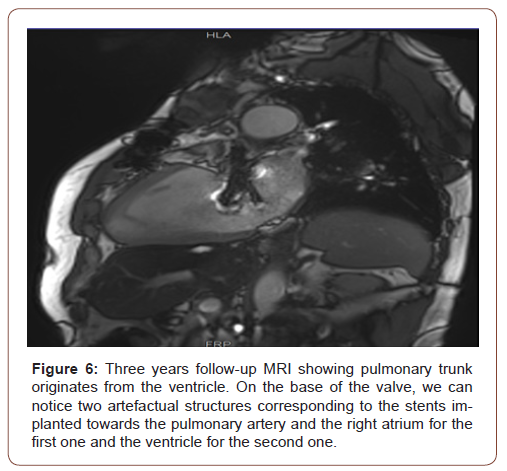
In our case the procedure was safe, without any complication.At one month follow-up, the ventricular function was improved and the patient resumed sport activity. Pulmonary peak gradient measured by echo-Doppler was 66 mmHg and mean gradient was 33 mmHg. Neither pericardial effusion or cardiac tamponade nor atrio-ventricular leak were observed. At three-year and six-year follow-up, the patient was clinically stable and asymptomatic. In (Figure 5) we show the stenting between the ventricle and the pulmonary trunk at the 2D echocardiography. The MRI (Figure 6) demonstrates the patency of the stent between the pulmonary artery and the ventricle. Additionally, it shows that the pulmonary trunk originates from a double outlet left ventricle and that the left and the right pulmonary arteries are confluent.
Conclusion
This case shows that the retrograde transcatheter perforation emerged as an original and successful option to treat pulmonary atresia in alternative to surgical management. At six years followup, the patient was still stable and asymptomatic.
Acknowledgement
We Thank Dr. Fabiola SOZZI for its advices and suggestions on the manuscript.
Conflict of Interest
No conflict of interest.
References
- Odemis E, Ozyilmaz I, Guzeltas A, Erek E, Haydin S, et al. (2013) Transcatheter management of neonates with pulmonary atresia with intact ventricular septum: a single center experience from Turkey. Artif Organs 37(1): E56‐E61.
- Alcíbar-Villa J, Rubio A, Peña N, Galdeano JM, Luis M, et al. (2007) Pulmonary atresia with intact ventricular septum. Perforation and pulmonary valvuloplasty using a modified mechanical technique. Medium-term follow-up. Rev Esp Cardiol 60(8): 833‐840.
- Rosenthal E, Qureshi SA, Chan KC, Martin RP, Skehan DJ, et al. (1993) Radiofrequency-assisted balloon dilatation in patients with pulmonary valve atresia and an intact ventricular septum. Br Heart J 69(4): 347‐351.
- Pinto RI, Dalvi B (2004) Transcatheter guidewire perforation of the pulmonary valve as a palliative procedure in pulmonary atresia with intact interventricular septum. Indian Heart J 56(6): 661‐663.
- Alwi M, Budi RR, Mood MC, Leong MC, Samion H (2013) Pulmonary atresia with intact septum: the use of Conquest Pro coronary guidewire for perforation of atretic valve and subsequent interventions. Cardiol Young 23(2): 197‐202.
- Patil NC, Saxena A, Gupta SK, Juneja R, Mishra S, et al. (2016) Perforating the atretic pulmonary valve with CTO hardware: Technical aspects. Catheter Cardiovasc Interv 88(5): E145‐E150.
- Hugues N, Abadir S, Dragulescu A, Nassi C, Errera J, et al. (2009) Transcatheter perforation followed by pulmonary valvuloplasty in neonates with pulmonary atresia and ventricular septal defect. Arch Cardiovasc Dis 102(5): 427‐432.
- Bakhru S, Marathe S, Saxena M, Verma S, Saileela R et al. (2017) Transcatheter pulmonary valve perforation using chronic total occlusion wire in pulmonary atresia with intact ventricular septum. Ann Pediatr Cardiol 10(1): 5‐10.
- Gupta SK, Juneja R, Saxena A (2017) Central perforation of atretic pulmonary valve using coronary microcatheter. Ann Pediatr Cardiol 10(3): 304‐305.
- Abrams DJ, Rigby ML, Daubeney PE (2003) Images in cardiovascular medicine. Membranous pulmonary atresia treated by radiofrequency-assisted balloon pulmonary valvotomy. Circulation 107(15): e98‐e99.
-
Nicolas Hugues, Bruno Vare, Carine Dommerc, François Bourlon. Retrograde Transcatheter Perforation in Adult with Pulmonary Atresia and Single Ventricle: A Unique Case of Ventricular Outflow Tract Opening. On J Cardio Res & Rep. 5(2): 2021. OJCRR.MS.ID.000610.
-
Transcatheter perforation, Ventricular outflow tract, Coronary guidewire, Atretic pulmonary valve, Stenting, Double outlet ventricle, Cardiopathy, Echocardiogram, Pericardial effusion, Heart disease, Heart rhythm, Pulmonary artery
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






