 Review Article
Review Article
Prevalence and Impact of Patent Foramen Ovale in Patients with Obstructive Sleep Apnea
Phillip J Camp1*, Abinash Achrekar1, Umar I Malik2, Lee Brown3, Mark J Ricciardi4 and Ihab Alomari5
1Department of Cardiology, The University of New Mexico School of Medicine, USA
2Department of Internal Medicine, The University of New Mexico, USA
3Department of Pulmonary, Critical Care and Sleep Medicine, The University of New Mexico, USA
4Department of Interventional Cardiology, Northwestern Memorial Hospital, USA
5Department of Interventional Cardiology, The University of California Irvine, USA
Phillip J Camp, Department of Cardiology, The University of New Mexico School of Medicine, USA.
Received Date: February 27, 2020; Published Date: March 12, 2020
Abstract
Background: It is well known that obstructive sleep apnea (OSA) prevalence increases as body mass index (BMI) increases. Patients with OSA experience nocturnal apnea episodes which can result in hypoxemia, transient elevation of right atrial pressures, and a possible increase in right to left shunting. As such, OSA diagnosis and therapy may be tailored to address right-to-left shunting in these patients. Whether the prevalence of PFO in OSA patients is or is not increased, it may be appropriate to include transthoracic echocardiography (TTE) testing as a component of routine evaluation of patients with OSA.
Objectives: We hypothesize that patients with hypoxemia related to OSA are more likely to have a PFO than those patients with OSA without hypoxemia.
Methods: 80 patients with OSA verified by 4 different criteria were referred for TTE by the UNM Sleep Center. All patients underwent saline contrast TTE. The prevalence of PFO in our general echo population was calculated over the last year for comparison.
Results: Of 80 patients with varying degrees of OSA, ten (12.5%) had right to left shunting. PFO was not statistically associated with any AHI (Apnea Hypopnea Index). The only statistically significant association was between OSA and BMI (p<0.001). The prevalence of PFO in the control group was found to be 12.2%.
Conclusions: In contrast to previous studies, there was no association between OSA of any severity and PFO in our study population. There however was a statistically significant association between OSA and BMI.
Abbreviations: PFO: Patent Foramen Ovale; OSA: Obstructive Sleep Apnea; TTE: Transthoracic Echocardiogram; BMI: Body Mass Index; AHI: Apnea Hypopnea Index
Introduction
The epidemic of obesity has been well documented. Over 65 percent of U.S. adults are either overweight or obese [1]. Twenty percent of those overweight with a mean body mass index (BMI) of 25 to 28 have been estimated to have mild obstructive sleep apnea (OSA), and 6 percent of the overweight have been estimated to have at least moderate OSA [2]. Further supporting the link between obesity and OSA is the Wisconsin trial which showed that weight loss decreased the severity of OSA.2 However, not all patients with OSA are obese and it is estimated in the general population that 4% of middle aged men and 2% of middle aged women have OSA [3]. OSA has been demonstrated to produce significant adverse health consequences including development of systemic hypertension; increased risk of myocardial infarction; increased insulin resistance; and particularly relevant for the present study, an increased risk of stroke [4]. Patent foramen ovule (PFO) is a prevalent condition found in approximately 20 percent of adults on autopsy [5]. Shunting of venous blood across a PFO occurs when there is a higher right atrial than left atrial pressure and may result in paradoxical emboli [6,7]. Patients with OSA experience nocturnal apnea episodes which can result in systemic arterial oxyhemoglobin desaturation and transient elevation of right atrial pressures. In the presence of complicating cardiopulmonary conditions, there may be persistent pulmonary hypertension. Transesophageal echocardiography (TEE) is thought to be the gold standard for detection of PFO, however, it is semi-invasive and in the sedated patient makes detecting right-to-left shunting more difficult due to the lack of ability to perform the Valsalva maneuver [9]. A study by Lam, et al. in 2011 showed that there was no significant difference in sensitivities between TEE and TTE in detection of PFO when the Valsalva maneuver was employed [9]. Further supporting TTE in screening for PFO is a study which did not show any significant difference in detection of PFO between TTE and TEE [10]. Our hypothesis is there is a correlation between OSA and PFO and that OSA diagnosis and therapy may be tailored to better address potential right-to-left shunting. We believe that available data support routine TTE evaluation of patients with OSA with high proportional desaturation for PFO.
Methods
Study population
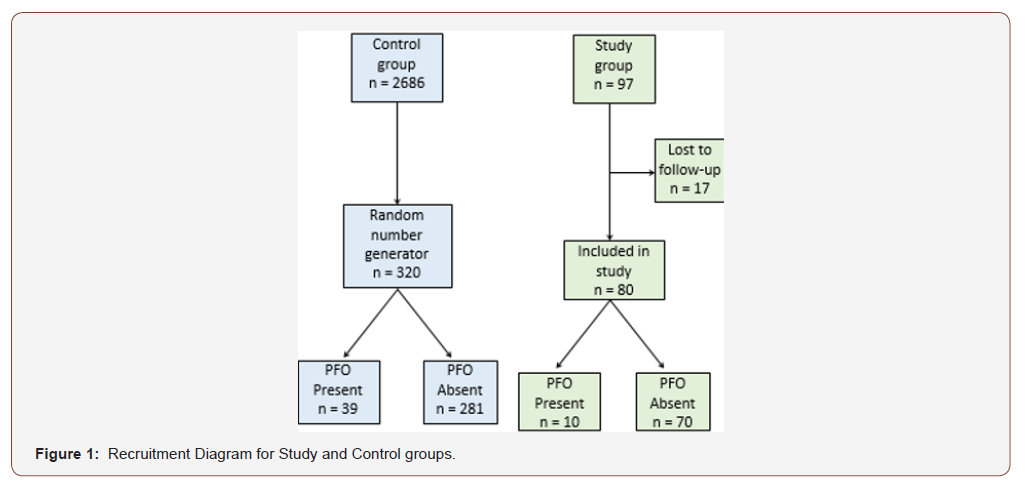
The study was reviewed and approved by the Institutional Review Board at the University Of New Mexico School Of Medicine in Albuquerque New Mexico. The sample included 97 patients (Figure 1). Patients were included if they had documented obstructive sleep apnea by overnight sleep study conducted at the University of New Mexico Sleep Center. Patients then underwent a saline agitated contrast transthoracic echocardiogram to evaluate for the presence of a PFO. Over the last year, 2,686 patients in the general population of patients were referred for TTE with saline bubble study. A random number generator was used (random.org) to select a frequency matched sample (4:1) to serve as the control group. The first 320 patients were selected in order of randomization.
Transthoracic echocardiography
Complete TTE with bubble contrast were performed during Valsalva and Mueller’s maneuver (inhaling against a closed throat) at which time continuous pulse oximetry was measured. Complete TTE includes two-dimensional short and long axis parasternal, four-chamber, two-chamber, three-chamber, subcostal, and Inferior vena cava views. M-mode, pulse wave, continuous-wave, and color-flow Doppler studies were performed. The peak velocity of tricuspid regurgitant flow was recorded and the systolic pulmonary artery pressure was estimated using the modified Bernoulli equation.
Assessment of presence of patent foramen ovale
The transthoracic four-chamber view was utilized to locate the thinnest portion of the interatrial septum and to interrogate for the presence of a PFO. Color flow and pulse Doppler was performed to assess flow patterns across the septum. Echocardiographic contrast was obtained by mixing 10 mL of normal saline solution with 1 mL of air in a syringe. Boluses (large doses of medication given over a short period of time) of agitated saline solution were rapidly injected into a peripheral vein and echogenic microbubbles, which dissipate within the pulmonary circulation, were imaged as they entered the right-sided chambers of the heart. In the presence of a PFO, these microbubbles are seen to traverse the interatrial septum from right-to-left. The passage of these microbubbles is aided by the transient elevation of right atrial pressure produced by either forceful coughing or Valsalva maneuver for 15 seconds. The efficacy of cough or Valsalva maneuver was validated by observing a movement of the interatrial septum toward the left atrium following release of the Valsalva maneuver. At least three contrast injections were performed in each subject, one before, one during Valsalva maneuver, and one during Mueller’s maneuver. Each patient was evaluated for the presence of an atrial septal defect other than a PFO by both color and spectral Doppler.
Polysomnography
Sleep Studies were conducted at the University of New Mexico Health Sciences Sleep Disorders Center. Polysomnography was conducted according to established clinical protocols of the UNM Sleep Disorders Center, the New Mexico Sleep Society, and the American Academy of Sleep Medicine.
Recording procedure: Data was collected using Bio-logic digital monitoring systems or a similar upgraded system. EEG was recorded from frontal, central, and occipital scalp regions with simultaneous time-locked continuous recording of eye movements (EOG), cardiac rate and rhythm (EKG), submentalis EMG, right and left leg EMG(anterior tibialis), snoring, body position, arterial oxyhemoglobin saturation and synchronized digital video monitoring. A polysomnographic technologist was in attendance throughout this test. End-tidal or transcutaneous carbon dioxide monitoring was used when appropriate. Expanded but still limited EEG channels were added when indicated.
Scoring criteria: The study was manually scored, using sleep staging criteria of Rechtschaffen and Kales. The scoring of respiratory events, arousals, and leg movements was performed in accordance with standards recommended by the American Academy of Sleep Medicine and New Mexico Sleep Society.
Definition of Terms
Apnea is a cessation of nasal/oral airflow despite continued respiratory effort for a minimum duration of 10 seconds.11 Hypopnea is defined as a 30% or greater reduction in thoraco-abdominal movement or airflow lasting at least 10 seconds terminated by either an arousal or awaking.11 AHI (apnea hypopnea index) is the average number of apneas and hypopneas per hour of sleep with significance determined by both the American Academy of Sleep Medicine and by the Centers for Medicaid and Medicare Services [11]. The oxygen desaturation index (ODI) is defined as the number of desaturation episodes with a reduction in saturation of >4% from baseline per hour of sleep [11]. Proportional desaturation can thus be expressed as the ratio of ODI (desaturations/hour) divided by the AHI (respiratory events/hour), that is, desaturations/event. High proportional desaturation will be defined as ODI/AHI > 0.70 desaturations/event. In addition, prior to lights out (the initiation of the sleep study), pulse oximetry (pulse and oxygen saturation levels) will be measured during intentional breath hold and Valsalva. A patent foraman ovale was considered present if a minimum of five microbubbles were seen in the left atrium within three cardiac cycles after opacification of the right atrium following peripheral echocontrast injection. An atrial septal defect was considered present if a consistent discontinuity of the septum was observed in different echocardiographic views and a left to right Doppler flow signal across the septum was recorded. All studies were interpreted separately by two independent observers who had no prior information about the patient’s clinical status.
Statistical Analysis
Continuous variables are summarized as mean ± SD. Categorical variables are summarized as counts or percentages. Unpaired t tests were used for comparison of continuous variables between defined groups. Chi square tests were used to compare categorical variables between defined groups and to test for bivariate associations. Univariable and multivariable logistic regression was used to test the association between PFO presence and selected independent variables. Statistical significance was defined when p < 0.05. Using a control PFO rate of 12.5%, as observed in our pilot investigations, a sample size of 400 patients with a 4:1 ratio of control to OSA (320 control patients and 80 OSA patients) would be necessary to identify a minimal clinically important different of 12.5% between OSA and control groups with 5% confidence and 80% power.
Result
Table 1: Patient Characteristics.
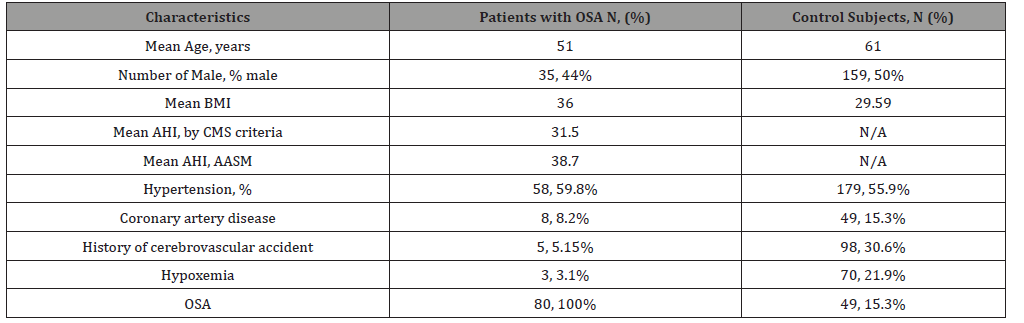
Table 2: ndications for Referral for TTE in Control Group.
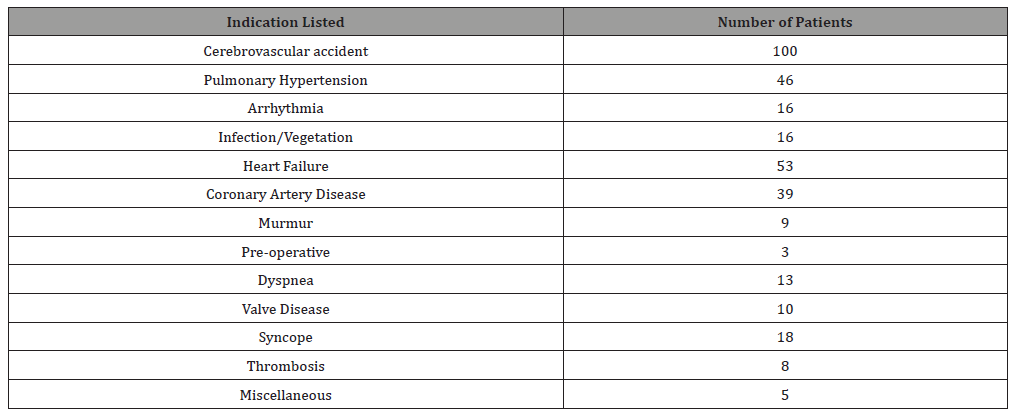
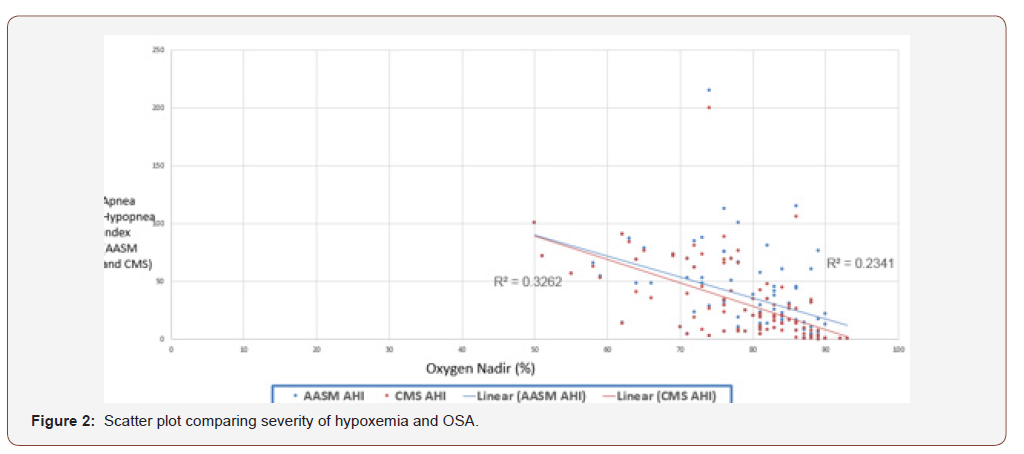
Of the 97 patients initially enrolled in the study, 17 were lost to follow because they did not receive a complete echocardiogram with bubble study. The baseline characteristics of the 97 initially enrolled patients are in (Table 1). The control subjects had higher rates of hypoxemia, coronary artery disease and stroke, similar rate of hypertension and lower BMIs. All of the study patients had OSA in varying degrees of severity while the control group incidence of OSA was 15.3%. (Table 2) lists the different indications for referral in the control group, the vast majority being cerebrovascular accident (100/320 patients) and hypertension (46/320 patients). Any degree of right to left shunting was present in 10 (12.5%) of the 80 patients compared with 39 (12.2%) of the 320 controls (p=0.939). There were statistically significant associations between OSA and BMI (p<0.05), BMI and DI (p=0.017), AASM AHI (p=0.022) and CMS AHI (p=0.005) (Table 3). There was no association between PFO and OSA (p=0.939), BMI (p=0.876), age (p=0.572), DI (p=0.302), AASM AHI (p=0.193) or CMS AHI (p=0.212) (Table 3).
Table 3: Correlation matrix for present study and associated p values from chi square analysis.
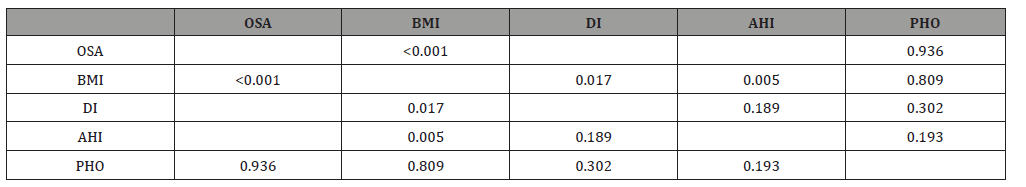
Table 4: Comparison of echocardiography findings and severity of OSA.
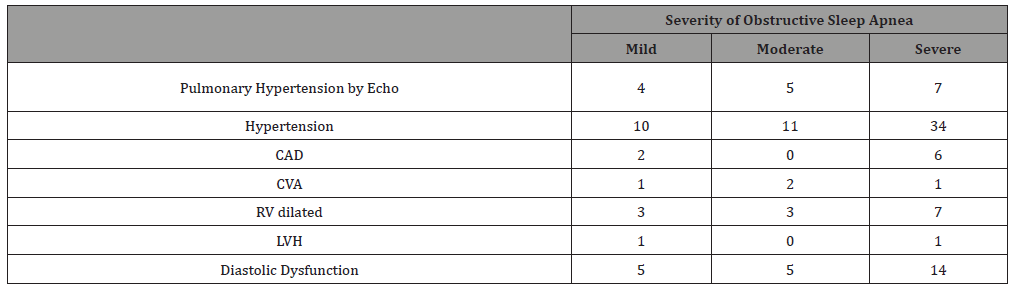
(Table 4) shows the number of patients with different echocardiography findings in relation to severity of OSA. As would be expected severe OSA has a higher number of patients with hypertension, coronary artery disease, right ventricular dilation and diastolic dysfunction. The number of patients with cerebrovascular accident was however not higher in the group OSA.
(Table 4) shows the number of patients with different echocardiography findings in relation to severity of OSA. As would be expected severe OSA has a higher number of patients with hypertension, coronary artery disease, right ventricular dilation and diastolic dysfunction. The number of patients with cerebrovascular accident was however not higher in the group OSA.
Discussion
Table 5: Prior studies of association between PFO and OSA.
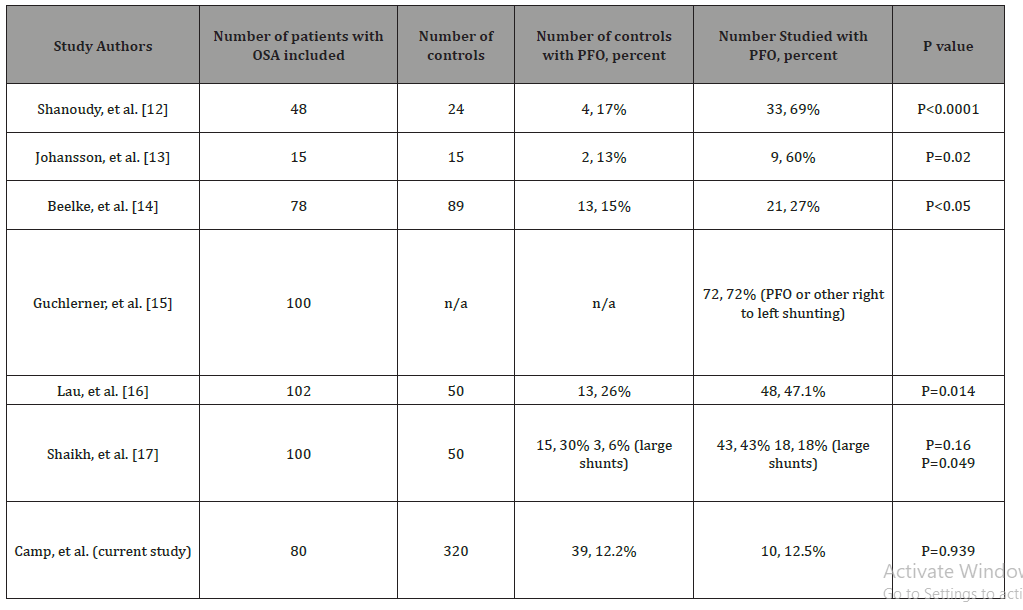
In this study we did not find that PFO is more prevalent in patients with OSA compared to the general population. The main finding in this study is contrary to our hypothesis and contrary to the majority of prior studies looking at the association between OSA and PFO. Multiple studies have evaluated the prevalence and impact of PFOs in patients with OSA and their key findings are found below in (Table 5). The first study followed 48 Veteran’s Affairs patients prospectively using TEE and found 69 percent had a PFO compared to 17 percent of matched controls [12]. This study documented significant hypoxemia after Valsalva maneuver (attempting to forcibly exhale while keeping the glottus closed) in subjects with a PFO. This study included a relatively small number of patients and employed TEE which is a semi-invasive procedure compared to TTE. A similar case control study found that 60 percent of 15 patients with prominent oxyhemoglobin desaturation characterized by proportional desaturation (as defined by a ratio of oxygen desaturation index/ apnea-hypopnea index greater than 0.66) had a PFO as opposed to 15 percent of 15 controls with less desaturation (ODI/AHI<0.33) [13]. This latter study similarly had a small number of patients included compared to our study. Another recent prospective study of 78 OSA patients using transcranial Doppler (TCD) found 27 percent had a PFO compared to 15 percent of matched controls [14]. Two studies in 2011 and 2012 used transcranial Doppler to look for right to left shunting in OSA and found 47.1% and 72% prevalence, respectively [15,16]. It should be noted that TCD cannot distinguish between a PFO and the rarer intra-pulmonary shunt. The most recent study examined 100 patients and compared them with 50 healthy controls using transthoracic echocardiography and found a non-significant difference of 43% compared to 30% prevalence, although they did find that patients with severe OSA had a higher prevalence of PFO with large shunts [17]. Our study included a larger number of controls and the prevalence of PFO in the two groups was much closer, 12.2% compared to 12.5%. More recently there have been studies looking at the efficacy of PFO closure, including the recently mentioned paper by Sheikh, et al. which did not recommend PFO closure. All of these studies reported a correlation between obstructive sleep apnea and PFO with different hypothesis regarding pathophysiology. One hypothesis presented in the previously mentioned studies is that increased intrathoracic pressure as the patient inhales against a closed airway increases the intrathoracic pressure thereby increasing right sided heart pressure. Another theory is that apneic episodes increase pulmonary artery pressure thereby also increasing right sided heart pressures [16]. These increases in right sided heart pressures translate to increased right atrial pressure which can in theory lead to right to left shunting. Our study found no correlation between PFO and even the most severe cases of OSA, and additionally found no correlation between PFO and obesity or the apnea hypopnea indices, all of which argue against each hypothesis.
Given the known potential harms of over testing, we cannot recommend routine screening with echocardiography for the detection of PFO in patients with obstructive sleep apnea as there does not appear to be any correlation between PFO and OSA. The impact of our study is that in the absence of a correlation, other etiologies for increased prevalence of stroke in OSA patients should be evaluated and that desaturation in OSA is not likely related to PFO. This is relevant as new technologies for PFO closure become more frequently employed as a tactic to reduce the incidence of stroke and reduce nocturnal desaturations. The incidence of PFO in OSA is the same as the general population undergoing routine echocardiography in our laboratory.
Study Limitations
This study has several limitations; the first being that patients were recruited over many years, and over that time period techniques in echocardiography and imaging modalities have changed. There is of course variation in the quality of the images obtained due to body habitus as well as technique. The demographics of our control patients were also slightly different, including an increased age and lower BMI, as these factors may have a theoretical contribution to the prevalence of PFO. Our study was powered to identify a 12.5% difference in PFO prevalence rates between control subjects and OSA patients. The observed difference of 0.3% (95% CI, -6.6% to 9.9%) provides assurance that there can be no more than a 10% higher difference in PFO prevalence between OSA and controls under the conditions of this study. A much larger study would be necessary to demonstrate a difference in PFO prevalence less than 10%.
AConclusion
Our results are contrary to previously published articles which document a significant association between OSA and PFO. We found no association between the two, and the incidence of PFO was very similar to the general population of patients studied with TTE at our institution. This is clinically important as percutaneous closure procedures are becoming more common in patients with cryptogenic stroke and a PFO. There is a hypothetical risk of stroke with PFO, but no increasingly identified independent risk with OSA. However, CVA rates were low in both arms and the study was clearly underpowered to look at this different question. Therefore, with no increased association of PFO in OSA, the indication for closure is questionable and may place the patient at greater risk of morbidity and mortality.
Acknowledgements
None.
Conflicts of Interest
No conflict of interest.
References
- Snapshot (2015) Accessed August 31.
- Young T, Peppard PE, Gottlieb DJ (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165(9): 1217-1239.
- Jordan AS, McSharry DG, Malhotra A (2014) Adult obstructive sleep apnoea. Lancet 383(9918): 736-747.
- Quan SF, Gersh BJ (2004) National Center on Sleep Disorders Research, National Heart, Lung, and Blood Institute. Cardiovascular consequences of sleep-disordered breathing: past, present and future: report of a workshop from the National Center on Sleep Disorders Research and the National Heart, Lung, and Blood Institute. Circulation 109(8): 951-957.
- Hagen PT, Scholz DG, Edwards WD (1984) Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc 59(1): 17-20.
- Nootens MT, Berarducci LA, Kaufmann E, Devries S, Rich S (1993) The prevalence and significance of a patent foramen ovale in pulmonary hypertension. Chest 104(6): 1673-1675.
- Parish JM, Shepard JW (1990) Cardiovascular effects of sleep disorders. Chest 97(5): 1220-1226.
- Coccagna G, Pollini A, Provini F (2006) Cardiovascular disorders and obstructive sleep apnea syndrome. Clin Exp Hypertens N Y N 28(3-4): 217-224.
- Lam YY, Yu CM, Zhang Q, Yan BP, Yip GW (2011) Enhanced detection of patent foramen ovale by systematic transthoracic saline contrast echocardiography. Int J Cardiol 152(1): 24-27.
- Marriott K, Manins V, Forshaw A, Wright J, Pascoe R (2013) Detection of right-to-left atrial communication using agitated saline contrast imaging: experience with 1162 patients and recommendations for echocardiography. J Am Soc Echocardiogr 26(1): 96-102.
- (1999) Sleep related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22(5): 667-689.
- Shanoudy H, Soliman A, Raggi P, Liu JW, Russel DC, et al. (1998) Prevalence of patent foramen ovale and its contribution to hypoxemia in patients with obstructive sleep apnea. Chest 113(1): 91-96.
- Johansson MC, Eriksson P, Peker Y, Hedner J, Råstam L, et al. (2007) The influence of patent foramen ovale on oxygen desaturation in obstructive sleep apnoea. Eur Respir J 29(1): 149-155.
- Beelke M, Angeli S, Del Sette M (2003) Prevalence of patent foramen ovale in subjects with obstructive sleep apnea: a transcranial Doppler ultrasound study. Sleep Med 4(3): 219-223.
- Guchlerner M, Kardos P, LissKoch E (2012) PFO and right-to-left shunting in patients with obstructive sleep apnea. J Clin Sleep Med 8(4): 375-380.
- Lau EMT, Jaijee SK, Melehan KL (2013) Prevalence of patent foramen ovale and its impact on oxygen desaturation in obstructive sleep apnea. Int J Cardiol 165(1): 35-40.
- Shaikh ZF, Jaye J, Ward N, Malhotra A, De Villa M, et al. (2013) Patent foramen ovale in severe obstructive sleep apnea: clinical features and effects of closure. Chest 143(1): 56-63.
-
Phillip J Camp, Abinash Achrekar, Umar I Malik, Lee Brown, Mark J Ricciardi, et al. Prevalence and Impact of Patent Foramen Ovale in Patients with Obstructive Sleep Apnea. On J Cardio Res & Rep. 3(4): 2020. OJCRR.MS.ID.000568.
-
Sleep apnea, Echocardiography, Hypoxemia, Patent foramen ovale, Body mass index, Hypertension, Stroke, Cardiopulmonary, Valsalva maneuver, Cardiac rate, Polysomnographic, Pathophysiology
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






