 Review Article
Review Article
Interpreting Troponin Elevation in The Setting of Infective Endocarditis: Causes and Prognostic Value
Ronan Canitrot1, Clement Delmas1, Clémence Delon1, Caroline Biendel1, Lydie Porte2, Fréderic Bouisset1, Clémence Laperche1, François Labaste3, Meyer Elbaz1, Didier Carrié1, Michel Galinier1, Yoan Lavie Badie1,4,5 and Jérôme Roncalli1*
1Department of Cardiology, Institute Cardiomet, University Hospital of Toulouse, France
2Department of Infectious Diseases, University Hospital of Toulouse, Toulouse, France
3Department of Anesthesiology, University Hospital of Toulouse, Toulouse, France
4Department of Nuclear Medicine, University Hospital of Toulouse, France
5Heart Valve Center, University Hospital of Toulouse, France
Jérôme Roncalli, Department of Cardiology, Institute Cardiomet, University Hospital of Toulouse, Toulouse, France.
Received Date:June 21, 2022; Published Date:July 08, 2022
Abstract
Background: Measurement of cardiac troponin (cTn) levels in blood is standard for diagnosis and risk stratification in cardiac emergencies. Our aim is to investigate the causes, the link with the underlying coronary artery disease and prognostic value of cTn release in infective endocarditis (IE).
Method: Eighty-six consecutive patients hospitalized for acute IE, with at least one cTn drawn and a coronary angiogram performed, were reviewed retrospectively. Factors related to the increase of cTn above the 99th percentile or above 10 times normal (>10N), as well as their prognostic impact, were assessed.
Results: The mean patient age was 63 +/ 14 years, the majority were men (n=68, 79%) with staphylococcus IE (n=34, 40%). Cardiac troponins were elevated above the 99th percentile for 74 (86%) patients and >10 N for 25 (29%) patients. There was no statistically significant correlation between elevated cTn and the presence of an underlying coronary artery disease. Cardiac troponin elevation above the 99th percentile was significantly associated with impaired renal function (p=0.04) and staphylococcus infection (p=0.02). A rise of cTn >10N was significantly associated with acute pulmonary edema (p=0.001), myocardial abscess (p=0.01), staphylococcus (p=0.0004), streptococcus (p=0.008), and renal function (p=0.0001). The average follow-up period was 919+/-816 days, and an elevation of cTn>10 N had a clear prognostic impact (HR 2.38, 95%CI 1.18-4.84, p=0.01).
Conclusion: Troponin elevation in IE is frequent and appears to be related to direct and indirect myocardial injury. It is associated with a poor prognosis.
Keywords:Coronary artery disease; Cardiac troponin; Infective endocarditis
Background
Infective endocarditis (IE) is a rare but serious disease. Patients are often referred to intensive cardiac care units, where diagnostic tests are performed. While echocardiography and blood cultures are the cornerstone of diagnosis, many biomarkers can be referenced, such as cardiac troponin (cTn) [1]. The troponin complex is composed of 3 subunits: troponin C, troponin I (cTnI), and troponin T (cTnT), which are located on the thin filament (actin) of the contractile system of striated skeletal and cardiac muscles. These proteins are involved in regulating muscle contraction. Myocardial cell injury results in the release of cTnI and cTnT. It has been demonstrated that elevated levels of these isoforms are associated with increased mortality in acute coronary syndrome, pulmonary embolism, heart failure, and chronic renal failure.
Upon admission to intensive cardiac care units, it is common practice to determine plasma levels of cTn. In IE, the result of this test is often difficult to interpret and can lead to diagnostic confusion, especially with acute coronary syndromes. The aim of this work is to investigate the causes of cTn elevation during IE, particularly the potential link to underlying coronary artery disease.
Materiel and Method
Study population
We performed a retrospective review of all hospital records from consecutive patients hospitalized in the Toulouse University Hospital Center between March 2013 and December 2016 with proven IE (according to the Duke criteria), and a potential indication for cardiac surgery [1]. Among these patients, only patients with a cTn assay performed upon admission and a coronary angiogram performed before discharge were considered for this study. Patients with infective right heart IE secondary to a pacemaker or implantable endocardiac defibrillator infection, as well as patients with IE on left ventricular assist devices were excluded. Microorganisms were proven via blood cultures, in accordance with the current guidelines of the European Society of Cardiology [1]. In cases of negative blood cultures, serologic tests for rare causes of IE were performed.
All patients were assessed via transesophageal echocardiography. Ultrasound data included description of valvular lesions, presence or absence of severe valvular regurgitation, presence of valvular abscess, and left ventricular ejection fraction using the Simpson biplane method. Severe regurgitation was defined according to the current guidelines [2]. An abscess was defined as a thickened, non-homogeneous perivalvular area with an echodense or echolucent appearance [3]. All patients underwent cerebral imaging (computed tomography angiography or magnetic resonance imaging) to assess neurological complications. Glomerular filtration rate (GFR) was calculated using the Cockcroft– Gault formula according to sex.
Determining troponin levels
The cTn assay was performed during the acute phase of IE, as part of a protocolized admission blood test. From March through December 2013, cTnI ultra-sensitive (ADVIA Centaur immunoassay, Siemens) was used, and from January 2014 through December 2016, cTnT high-sensitive (electrochemiluminescence immunoassay, ROCHE) was used. Troponin was considered positive when its blood levels were elevated above the 99th percentile upper reference limit, thus cTn T was considered positive if it was > 14 ng / L, and cTn I was considered positive if it was > 0.05 μg / L. Receiver operating curve (ROC) was performed for assessing the best cut-off of troponin for predicting the primary endpoint. A threshold of 10 times normal (10N) was then added, means > 140 ng / L for cTnT and > 0.5 μg / L for cTnI.
Coronary angiography
Coronary angiography was performed mainly because of the need for surgical management of IE, according to the guidelines [1], as a systematic part of presurgical assessment. All exams were blind reviewed for the study by the same person. Coronary stenosis was considered significant in the presence of coronary artery stenosis > 70% or > 50% for the left main coronary. Three-vessel disease was related to the presence of significant stenosis of the three main coronary arteries.
Outcomes
The primary endpoint of the study was the incidence of all causes of death during follow-up. Clinical event data were collected during the follow-up period for all patients by reviewing medical files and by phone contact with patients, relative or general practitioner.
Ethical statement
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed oral consent was obtained from all individual participants included in the study, in accordance with the French Data Protection Authority (Commission Nationale de l’Informatique et des Libertés, CNIL n° 2206723).
Statistical analysis
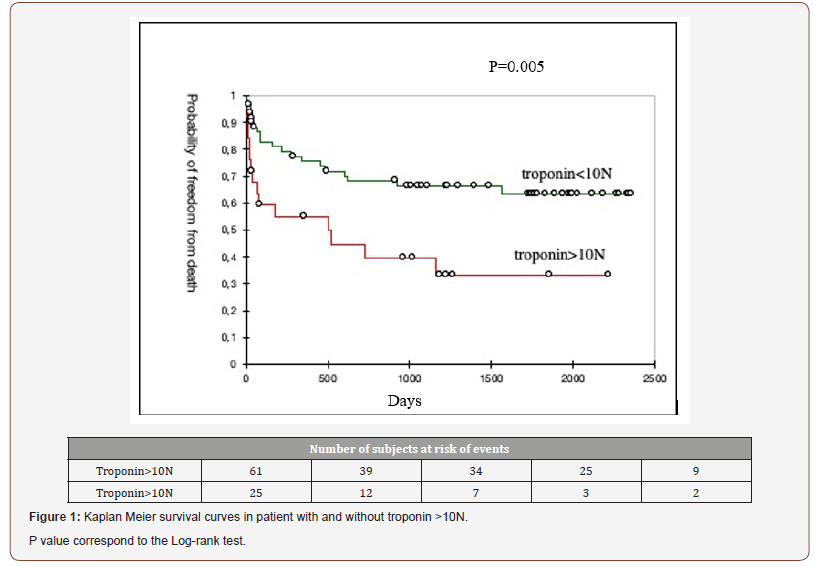
Continuous variables were expressed as mean ± standard deviation. Nominal values were expressed as numbers and percentages. Categorical differences between groups were evaluated using the chi-2 test or the Fisher exact test (for small sample sizes). A value of p<0.05 was considered significant. Kaplan- Meier survival curves and log-rank values were used to assess survival in subgroups. Univariate Cox regression analysis was performed to assess the association of the variables with long-term mortality. Variables that were significant in the univariate analysis were analyzed using the multivariate Cox regression model. Results of the Cox regression analysis were reported with hazards ratios (HR) and 95% confidence intervals (CI). Statistics were analyzed using XLSTAT v2019.1 (Addinsoft, Paris, FR).
Result
Population characteristics
Eighty-six patients hospitalized for IE with surgical indication, between March 2013 and December 2016 at Toulouse University Hospital, underwent a coronary angiography as a part of presurgical assessment, had a cTn assay upon admission and were included in this study. Mean age was 63±14 years, and 68 patients (79%) were men. From a microbiology perspective, 35 patients (40%) presented with Staphylococcal IE, 29 (33%) with Streptococcus, 12 (14%) with Enterococcus, and 5 patients (5%) had no identified germs (Table 1).
Table 1: Patient characteristics.
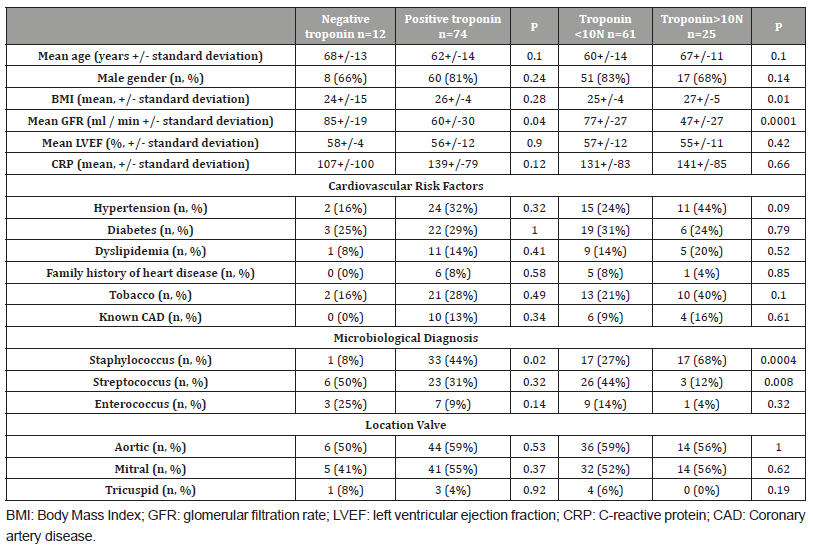
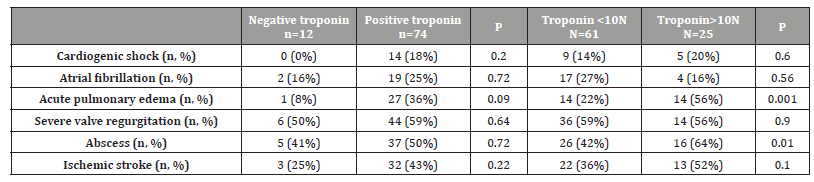
Regarding the complications of IE, 29 patients (33%) presented with acute pulmonary edema, 14 (6%) with cardiogenic shock, 22 (25%) presented with AF, 22 (13%) with type 3 atrioventricular block, and 36 (41%) with ischemic stroke. Forty-five patients (51%) had an abscess (Table 2).
All patients included in the study had an indication for surgical management, and 75 (86%) underwent surgery. The indication for surgical management was secondary to hemodynamic failure for 50 patients (57%), uncontrolled sepsis in 52 patients (59%), and high embolic risk in 32 patients (37%).
Table 2: Troponin elevation and complications of infective endocarditis.
Elevation of troponin above the 99th percentile
Seventy-four (86%) patients had elevated cTn levels above the 99th percentile upper reference limit. The cTnT assay involved 74 patients (86%), and cTnI was performed on 12 patients (14%). The mean rate of cTn T was 314 ng/l, and 0.33 μg/L for cTn I. The presence of cTn was significantly associated with impaired renal function (GFR 60+/-30 ml/min vs. 85+/-19 ml/min, p=0.04) and the presence of Staphylococcus (n=33 (44%)) vs. (n=1 (8%) p=0.02).
Elevation of troponin greater than ten times normal levels
Twenty-five (29%) patients had an elevation of cTn>10N. There was a statistically significant relationship with a high BMI (27+/- 5 vs. 25+/-4; p=0.01), impaired renal function, (GFR 47+/-27ml/ min vs. 77+/-27 ml/min, p=0.0001), staphylococcal infection (n=17 (68%), vs. n=17 (27%); p=0.0004) and Streptococcus infection (n=26 (44 %) vs. n=3 (12%), p=0.008).Regarding IE complications, there was a significant association between elevation of cTn > 10N and acute pulmonary edema ((n=14 (56%) vs. n=14 (22%); p=0.001) and the presence of a myocardial abscess (n=16 (64%) vs. n=26 (42%), p=0.01).
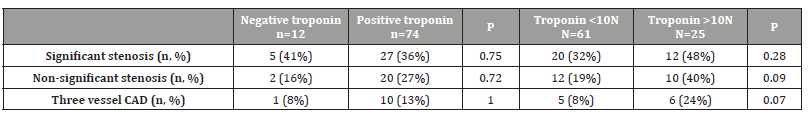
Troponin elevation with respect to coronary status
Thirty-two patients (37%) had a significant coronary lesion, and 11 (13%) had three-vessel disease. Elevation of cTn, whether important or not, was not associated with patients’ coronary status (Table 3). Depending on whether insignificant, significant, or threevessel CAD lesions are present, there is no significant association with elevated cTn levels.
Table 3: Troponin elevation by coronary status.
Outcomes
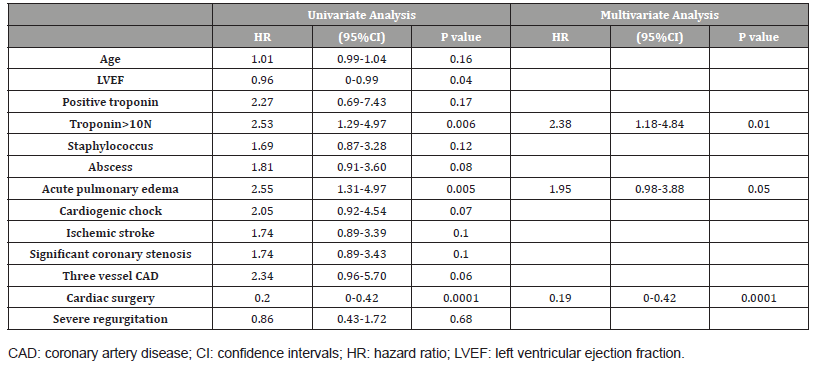
The average follow-up period was 919+/-816 days. Thirty-five patients (40%) died during follow-up. Based on univariate Cox regression analysis (Table 4), cTn >10N (HR 2.53, 95%CI 1.29-4.97, p=0.006), acute pulmonary edema (HR 2.55, 95%CI 1.31-4.97, p=0.005) were significantly associated with mortality, whereas cardiac surgery (HR 0.2, 95%CI 0-0.42, p=0.0001) was significantly associated with survival. The main predictor of mortality, based on multivariate analysis (Table 4), was elevation of cTn greater than 10N (HR 2.38, 95%CI 1.18-4.84, p=0.01), and the main predictor of survival was cardiac surgery (HR 0.19 95%CI 0-0.42, p=0.0001). Similar results were obtained with the Kaplan Meyer curves (Figure 1).
Table 4: Results of univariate and multivariate Cox regression analysis to predict long-term mortality.
Discussion
In IE, elevation of cTn above the 99th percentile upper reference limit is common and not related to atherothrombotic coronary artery disease. Staphylococcal infection and renal failure appear to be the main determinants of cTn rise. A significant elevation of cTn (greater than 10N) seems to have a clear prognostic impact and is associated with more severe complications of IE.
Several observational studies in small cohorts have previously reported that there was an elevation of cTn in the majority of patients with IE (57-73%) [4-7]. According to the 4th universal definition of myocardial infarction [8], a cTn elevation greater than the 99th percentile is considered a myocardial injury, in contrast to myocardial infarction, which is reserved to cTn elevation with clear signs of associated ischemia. Our study does not find any link between cTn elevation and the presence of an underlying coronary artery disease. The mechanism explaining the positivity of cTn does not, therefore, seem to be related to underlying acute coronary syndrome. However, it is likely that the presence of underlying severe coronary artery disease may contribute to myocardial injury (namely through oxygen supply/demand imbalance), as may be suggested by the trend toward an association between cTn elevation greater than 10N and three-vessel coronary disease.
In the setting of acute IE, cTn release appears to be linked mainly to myocardial injury, whose pathophysiological mechanism appears to be poly-factorial. Our study finds an association between renal function and cTn positivity, as well as between cTn elevation >10N and acute pulmonary edema. The associations between renal failure, heart failure, and cTn are well known [9,10]. The potential mechanisms involved in kidney diseases are increased ventricular pressure, small-vessel coronary disease, anemia, and direct toxic effects associated with the uremic state [11,12]. The mechanism of cTn release in heart failure remains unclear, but increased levels of neurohormonal factors, oxidative stress, cytokine release, and mechanic stress may be involved [13]. In sepsis, cTn elevation may be explained by ischemic events, by direct toxicity of inflammatory cytokines (TNF, IL-6 and bacterial endotoxins and reactive oxygen species), or by indirect effect with microvascular thrombosis and the procoagulant state [14]. However, there was no association between CRP level and cTn elevation in our study, even though CRP is a recognized intermediate marker of inflammation and sepsis. Direct myocardial injuries related to the pathogen may also be involved. Indeed, our study shows a link between cTn elevation and staphylococcal infection, with streptococcal infection in a more modest degree, as well as with abscesses. This association between cTn, staphylococcus infection [4], and abscesses [5] has already been proven in small series. Indeed, organisms such as Staphylococcus aureus are more often the cause of abscesses [15] and can enter the endothelial cells directly and be responsible for cell death [16], or damage the vascular endothelium, including the fibronectin, laminin and collagen [17].
Our study showed a clear prognostic impact of cTn elevation >10N. Other studies have previously highlighted the prognostic aspect of cTn assay in IE [5-7,18]. In this population, the performance of cardiac surgery was an important survival factor, which is consistent with current data in the literature [19].
The main limitation of this study is its selected population, which is not representative of all patients with IE. However, the population was chosen because the possibility of analyzing the presence of underlying coronary artery disease could provide important information, and only patients with surgical indications had a systematic coronary angiography. In addition, patients with a theoretical indication for surgery currently represent 75% of IE cases [19]. The method of determining cTn changed during the study, but we chose to use the 99th percentile of each method as a reference to avoid measurement bias.
Conclusion
Troponin elevation in IE is frequent and appears to be more related to direct and indirect myocardial injury and to pathogens and their complications than to a possible underlying coronary artery disease. It is associated with a poor prognosis.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Gilbert Habib, Patrizio Lancellotti, Manuel J Antunes, Maria Grazia Bongiorni, Jean Paul Casalta, et al. (2015) 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 36: 3075-3128.
- William A Zoghbi, David Adams, Robert O Bonow, Maurice Enriquez-Sarano, Elyse Foster, et al. (2017) Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr 30: 303-371.
- Gilbert Habib, Luigi Badano, Christophe Tribouilloy, Isidre Vilacosta, Jose Luis Zamorano, et al. (2010) Recommendations for the practice of echocardiography in infective endocarditis. Eur J Echocardiogr 11: 202-219.
- Watkin RW, Lang S, Smith JM, Elliott TSJ, Littler WA (2004) Role of troponin I in active infective endocarditis. Am J Cardiol 94: 1198-1199.
- Jonathan B Purcell, Mahesh Patel, Amit Khera, James A de Lemos, Lisa W Forbess, et al. (2008) Relation of Troponin Elevation to Outcome in Patients With Infective Endocarditis. Am J Cardiol 101: 1479-1481.
- Tsenovoy P, Aronow WS, Joseph J, Kopacz MS (2009) Patients with Infective Endocarditis and Increased Cardiac Troponin I Levels Have a Higher Incidence of In-Hospital Mortality and Valve Replacement than Those with Normal Cardiac Troponin I Levels. Cardiology 112: 202-204.
- Amy B Stancoven, Angela B Shiue, Amit Khera, Kristi Pinkston, Ibrahim A Hashim, et al. (2011) Association of troponin T, detected with highly sensitive assay, and outcomes in infective endocarditis. Am J Cardiol 108: 416-420.
- Kristian Thygesen, Joseph S Alpert, Allan S Jaffe, Bernard R Chaitman, Jeroen J Bax, et al. (2019) Fourth universal definition of myocardial infarction (2018). Eur Heart J 40: 237-269.
- Hamm CW, Giannitsis E, Katus HA (2002) Cardiac Troponin Elevations in Patients Without Acute Coronary Syndrome. Circulation 106: 2871-2872.
- Eduardo Roque Perna, Stella Maris Macín, Jorge Isaac Parras, Rolando Pantich, Eduardo Francisco Farías, et al. (2002) Cardiac troponin T levels are associated with poor short- and long-term prognosis in patients with acute cardiogenic pulmonary edema. Am Heart J 143: 814-820.
- Faeq Husain-Syed, Peter A McCullough, Horst-Walter Birk, Matthias Renker, Alessandra Brocca, et al. (2015) Cardio-Pulmonary-Renal Interactions: A Multidisciplinary Approach. J Am Coll Cardiol 65: 2433-2448.
- de Filippi CR, Herzog CA (2017) Interpreting Cardiac Biomarkers in the Setting of Chronic Kidney Disease. Clin Chem 63: 59-65.
- Roongsritong C, Warraich I, Bradley C (2004) Common Causes of Troponin Elevations in the Absence of Acute Myocardial Infarction: Incidence and Clinical Significance. Chest 125: 1877-1884.
- Maeder M, Fehr T, Rickli H, Ammann P (2006) Sepsis-associated myocardial dysfunction: diagnostic and prognostic impact of cardiac troponins and natriuretic peptides. Chest 129: 1349-1366.
- Holland TL, Baddour LM, Bayer AS, Hoen B, Miro JM, et al. (2016) Infective endocarditis. Nat Rev Dis Primer 2: 1-22.
- Hamill RJ, Vann JM, Proctor RA (1986) Phagocytosis of Staphylococcus aureus by cultured bovine aortic endothelial cells: model for postadherence events in endovascular infections. Infect Immun 54: 833-836.
- Scheld WM, Strunk RW, Balian G, Calderone RA (1985) Microbial Adhesion to Fibronectin in Vitro Correlates with Production of Endocarditis in Rabbits. Proc Soc Exp Biol Med 180: 474-482.
- Snipsøyr MG, Ludvigsen M, Petersen E, Wiggers H, Honoré B (2016) A systematic review of biomarkers in the diagnosis of infective endocarditis. Int J Cardiol 202: 564-570.
- Gilbert Habib, Paola Anna Erba, Bernard Iung, Erwan Donal, Bernard Cosyns, et al. (2019) Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur Heart J 40: 3222-3232.
-
Ronan Canitrot, Clement Delmas, Clémence Delon, Caroline Biendel, Jérôme Roncalli, et al., Interpreting Troponin Elevation in The Setting of Infective Endocarditis: Causes and Prognostic Value. On J Cardio Res & Rep. 6(4): 2022. OJCRR.MS.ID.000645.
-
Coronary artery disease, Cardiac troponin, Infective endocarditis, Myocardial abscess, Cardiac surgery, Coronary stenosis, Renal failure, Heart failure, Acute coronary syndrome, Pulmonary embolism
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






