 Mini Review
Mini Review
Hyperlipidemia Associations with Hypertension Medications
Andréia Assis Loures Vale, Anita LR Saldanha, Ana Paula Pantoja Margeotto and Tania Leme da Rocha Martinez*
Department of Nephrology, BP – A Beneficência Portuguesa de São Paulo, Brazil
Tania Leme da Rocha Martinez, Department of Nephrology, BP – A Beneficência Portuguesa de São Paulo, Brazil.
Received Date: February 29, 2020s; Published Date: March 11, 2020
Abstract
Simultaneity of hypertension and hyperlipidemia as added risk factors for renal and cardiovascular disease cannot be approached without considering concomitant effect of some antihypertensive agents causing secondary hypercholesterolemia or hypertriglyceridemia. Hypertension and atherosclerosis are two important and related risk factors associated with the morbidity and mortality of patients with chronic renal failure. Increased prevalence of hypertensive nephropathy as a major cause of end stage renal disease has been reported. Among these patients, the cardiovascular morbidity is estimated around 10 to 20 times that observed in the general population and may be present in half of patients under dyalisis. Hypertension accelerates the development of atherosclerosis. On the other hand, dyslipidemias are associated to a higher dammage of hypertensive renal disease, aswell as to myocardial hypertrophy and to the incidence of cardiovascular events in hypertensive patients. Treatment of hypertension can modify the lipid profile and atherosclerosis induced by hyperlipidemia.
Keywords: Dyslipidemia; Hypertension; Risk factors; Cardiovascular disease; Prevention; Atherosclerosis
Abbreviations: LDL-c: Low Density Lipoprotein Cholesterol; TC: Total Cholesterol; VLDL-c: Very Low Density Lipoprotein Cholesterol
Introduction
MIn order to adequately address the treatment of hypertensive patients with dyslipidemia, we have to remember the importance of these two pathologies as risk factors for coronary heart disease. In addition to proven the two main factors [1], Systemic Arterial Hypertension and Dyslipidemia act synergistically, increasing cardiovascular risk [2]. Epidemiological studies [3-5] have shown that the risk of cardiovascular mortality increases with cholesterol levels - in a 55-year-old man, the risk is 0.6%/year for a cholesterol level of 245 mg/dL, dropping to 0.2% if the cholesterol level is reduced to 180 mg/dL. Published data [6] showed that 40% of all individuals with blood pressure greater than 140/90 mmHg or using antihypertensive medication have serum levels of total cholesterol (TC) greater than 240 mg/dL; and 46% of those with TC > 240 mg/ dL also have blood pressure greater than 140/90 mmHg. A frequent association of hypertriglyceridemia and hypoalphalipoproteinemia is also reported as elements of plurimetabolic syndrome described by Reaven, known as X Syndrome. Another relevant data in the recognition of these patients is the presence of metabolic alterations of glucose intolerance and lipid alterations resulting from the treatment of hypertension, reflecting possible adverse effects of hypotensor agents [7,8] on insulin sensitivity; obesity and sedentary lifestyle, factors that can be modified, contribute to a condition conducive to atherogenesis.
Effects of Antihypertensive Medicines
As previously reported, lipid and glucose intolerance alterations are more common in treated hypertensive patients, possibly reflecting the adverse effects of hypotensive agents [9,10] on insulin sensitivity. The possible cause of this condition are diuretics and beta-blockers.
Diuretics [11]
Thiazides are those who have proven to perform a negative action in the lipid profile; act by increasing the action of lipoprotein lipase, which hydrolyzes triglycerides and VLDL-c lipoproteins, increasing the production of LDL-c and TC. These changes are discrete and may return to normal with suspension of treatment.
Beta-blockers
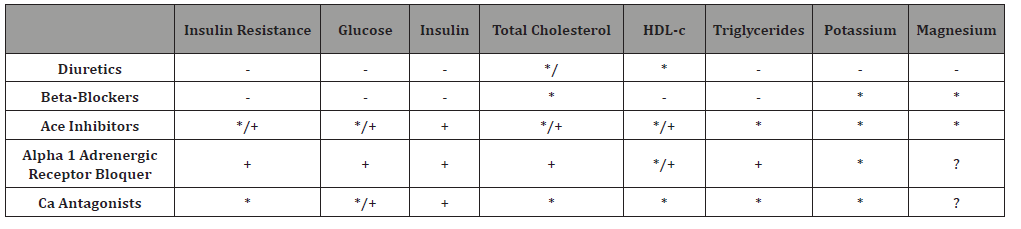
Table 1: Effects of Antihypertensives on Various Metabolic Parameters [8,12,16].
-->
Act by inhibiting the activity of adenyl cyclase in fatty cells, reducing hydrolysis of fatty acids and triglycerides; TC elevation (LDL-c and VLDL-c) and triglycerides [12]. As endothelial injury is the common basis for the actions of these two pathologies in the arterial wall, the ideal is that we try to use drugs that, in addition to not interfering in a negative metabolic form, have an antiproliferative and/or protective role on the arteries [13]. Calcium antagonists and angiotensin-converting enzyme inhibitors are the ones that best fit as a treatment option for dyslipemic hypertensive patients [8,14,15] (Table 1).
Drug Interactions
The known or theoretically possible interactions to occur are [17,18]:
a) Reduction of LDL-c with the use of sequelae of bile acids and thiazides diuretics.
b) Interference in the action of various antihypertensives when used in conjunction with nicotinic acid, aspirin or nonsteroidal anti-inflammatory agents.
c) Potential adverse effect of thiazide diuretics on hyperglycemia when administered together with nicotinic acid.
Acknowledgements
None.
Conflicts of Interest
No conflict of interest.
References
- Faludi AA, Izar COM, Saraiva JFK, Chacra APM, Bianco HT, et al. (2017) Atualização da Diretriz Brasileira de Dislipidemias e Prevenção da Aterosclerose – 2017. Arq Bras Cardiol 109(2Supl.1): 1-76.
- (1993) The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med 153(2): 154-183.
- Castelli WP (1994) Epidemiology of coronary heart disease: the Framingham study. Am J Med 76(2): 4-12.
- Kannel WB, D'Agostino RB, Wilson PW, Belanger AJ, Gagnon DR (1990) Diabetes, fibrinogen, and risk of cardiovascular disease: the Framingham experience. Am Heart J 120(6): 672-676.
- (1990) Mortality rates after 10.5 years for participants in the multiple risk factor intervention trial: findings related to a priori hypotheses of the trial. JAMA 263(13): 1795-1801.
- (1991) National Education Programs Working Group Report on the Management of Patients with Hypertension and High Blood Cholesterol. Working Group on Management of Patients with Hypertension and High Blood Cholesterol. Ann Intern Med 114(3): 224-237.
- Collins R, Peto R, MacMahon S, Hebert P, Fiebach NH, et al. (1990) Blood pressure, stroke and coronary heart disease: Part 2, Short-term reductions in blood pressure: overview of randomized drug trials in their epidemiological context. Lancet 335(8693): 827-838.
- Moan A, Os I, Hjermann I, Kjeldsen SE (1995) Hypertension therapy and risk of coronary heart disease: how do antihypertensives affect metabolic factors. Cardiology 86(2): 89-93.
- Cuttler R (1983) Effect of antihypertensive agents on lipid metabolism. Am J Cardiol 51(4): 628-631.
- Young WF, Calhoun DA, Lenders JWM, Stowasser M, Textor SC (2017) Screening for endocrine hypertension: An Endocrine Society Scientific Statement. Endocrine Reviews 38(2): 103-122.
- Ames RP (1983) Negative effects of diuretic drugs on metabolic risk factors for coronary heart disease: possible alternative drug therapies. Am J Cardiol 51(4): 632-638.
- Ames RP (1986) The effects of antihypertensive drugs on serum lipids and lipoproteins, I. Diuretics. Drugs 32(3): 260-278.
- Levine GN, Keaney JF, Vita JA (1995) Cholesterol reduction in cardiovascular disease. Clinical benefits and possible mechanisms. N Engl J Med 332(8): 512-521.
- Cleland JGF, Krikler DM (1993) Modification of atherosclerosis by agents that do not lower cholesterol. Br Heart J 69(1 Suppl): S54-S62.
- (1993) Summary of the Second Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II). JAMA 269(23): 3015-3023.
- Lardinois CK, Johns JP (1992) Cardiac drug effects on lipids. Current Opinion in Lipidology 3(4): 274-278.
- Peters TK, Mehra M, Muratti EN (1993) Efficacy and safety of fluvastatin in hypertensive patients. An Analysis of a Clinical Trial Database. Am J Hypertens 6(11 Pt 2): 340S-345S.
- Pool JL, Shear CL, Downton M, Schnaper H, Stinnett S, et al. (1992) Lovastatin and coadministered antihypertensive/cardiovascular agents. Hypertension 19: 242-248.
-
Tania Leme da Rocha Martinez, Andréia Assis Loures Vale, Anita LR Saldanha, Ana Paula Pantoja Margeotto. Hyperlipidemia Associations with Hypertension Medications. On J Cardio Res & Rep. 3(4): 2020. OJCRR.MS.ID.000567.
-
Dyslipidemia, Hypertension, Risk factors, Cardiovascular disease, Prevention, Atherosclerosis, Hypertriglyceridemia, Renal disease, Lipoprotein cholesterol, Blood pressure
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






